Abstract
Tissue-resident mast cells (MCs) have important roles in IgE-associated and -independent allergic reactions. Although microenvironmental alterations in MC phenotypes affect the susceptibility to allergy, understanding of the regulation of MC maturation is still incomplete. We previously reported that group III secreted phospholipase A2 (sPLA2-III) released from immature MCs is functionally coupled with lipocalin-type prostaglandin D2 (PGD2) synthase in neighboring fibroblasts to supply a microenvironmental pool of PGD2, which in turn acts on the PGD2 receptor DP1 on MCs to promote their proper maturation. In the present study, we reevaluated the role of sPLA2-III in MCs using a newly generated MC-specific Pla2g3-deficient mouse strain. Mice lacking sPLA2-III specifically in MCs, like those lacking the enzyme in all tissues, had immature MCs and displayed reduced local and systemic anaphylactic responses. Furthermore, MC-specific Pla2g3-deficient mice, as well as MC-deficient KitW-sh mice reconstituted with MCs prepared from global Pla2g3-null mice, displayed a significant reduction in irritant contact dermatitis (ICD) and an aggravation of contact hypersensitivity (CHS). The increased CHS response by Pla2g3 deficiency depended at least partly on the reduced expression of hematopoietic PGD2 synthase and thereby reduced production of PGD2 due to immaturity of MCs. Overall, our present study has confirmed that MC-secreted sPLA2-III promotes MC maturation, thereby facilitating acute anaphylactic and ICD reactions and limiting delayed CHS response.
Keywords: mast cells, phospholipase A2, lipid mediator, anaphylaxis, contact dermatitis
1. Introduction
Mast cells (MCs) promote acute allergic reactions, including anaphylaxis, a severe and potentially fatal immunoglobulin (IgE)-dependent immediate hypersensitivity reaction to apparently harmless antigen (Ag), as well as certain IgE-independent innate and adaptive immune disorders [1,2,3]. In addition to these detrimental functions, MCs also have beneficial functions by regulating both innate and adaptive immune responses against invading microorganisms, venom, and environmental toxins [1,2,3]. Crosslinking of the high-affinity receptor for IgE (FcεRI) on the surface of MCs with IgE and specific Ag initiates signals leading to the release of preformed, granule-stored molecules (degranulation), such as histamine and proteases, newly synthesized lipid mediators, such as the arachidonic acid (AA) metabolites prostaglandin D2 (PGD2) and leukotriene C4, and prestored or newly transcribed cytokines and chemokines such as tumor necrosis factor-α (TNF-α) and CCL2, all of which can be involved in the IgE-associated diseases [2,4,5]. The secretion of these bioactive factors by MCs can also be directly activated by diverse stimuli independently of IgE, and many of these factors are known to be present locally at sites of allergic inflammation [3,6,7].
Microenvironment alterations in MC phenotypes affect the susceptibility to hypersensitivity reactions [8]. MCs are derived from progenitors that undergo their terminal maturation after migrating into most vascularized tissues [5,8,9,10]. Based on recent studies, at least two different pathways for MC development have been described in mice; MCs in several connective tissues, such as the skin and peritoneum, originate from yolk-sac-derived MC progenitors at the embryonic stage [11,12], while MCs in other tissues arise from classical hematopoietic stem cells in the bone marrow (BM), with precursors traveling through the circulation before they acquire more mature characteristics in peripheral tissues [10,13,14,15]. The local development and maturation of MCs are thought to be regulated by signals provided by stromal cells within local tissue microenvironments. It is well known that the stem cell factor (SCF) and its receptor c-Kit (CD117) system, in cooperation with several transcription factors, is essential for adhesion, homing, proliferation, and differentiation of MCs [14]. However, as SCF alone is insufficient to fully drive the terminal maturation of MCs, it has been hypothesized that some other stromal factor(s) may be additionally required. Besides several accessory cytokines, growth factors, adhesion molecules, and extracellular matrices as potential candidates for these stromal factors [8,10,15], we have recently shown that a signal driven by the lipid mediator PGD2 represents a missing link required for the fibroblast-driven maturation of MCs [16].
The production of PGD2 is initiated by hydrolysis of membrane phospholipids by phospholipase A2 (PLA2). Of many PLA2 enzymes identified to date [17,18], group IVA cytosolic PLA2 (cPLA2α) is essential for the stimulus-coupled release of AA and subsequent production of PGD2 by hematopoietic PGD2 synthase (H-PGDS) in MCs [19,20,21]. The MC-derived, cPLA2α/H-PGDS-driven PGD2 exacerbates or attenuates allergic responses by acting on either of the two PGD2 receptors DP1 and DP2 (also known as CRTH2) expressed on different target cells [16,22,23,24,25,26,27]. In addition to this MC-intrinsic production of PGD2, MCs also regulate the production of a distinct pool of PGD2 by stromal fibroblasts, a process that is mediated by the paracrine action of secreted PLA2 (sPLA2) [16]. The sPLA2 family, which contains 11 isoforms in mammals, is structurally subdivided into group I/II/V/X, group III, and group XII branches [28]. Importantly, we have demonstrated that group III sPLA2 (sPLA2-III; encoded by Pla2g3), which is structurally similar to bee venom sPLA2 [29], is secreted from immature MCs and functionally coupled with lipocalin-type PGDS (L-PGDS) in neighboring fibroblasts as a paracrine factor to supply a microenvironmental pool of PGD2, which in turn acts on the PGD2 receptor DP1 on MCs to coordinate proper MC maturation [16]. Accordingly, mice lacking sPLA2-III, as well as those lacking L-PGDS or DP1, have immature MCs and display reduced local and systemic anaphylaxis in response to IgE-dependent and -independent stimuli. In addition, the defective MC maturation by Pla2g3 deficiency eventually leads to impaired cPLA2α/H-PGDS-driven PGD2 generation by MCs, implying that sPLA2-III drives both PGD2 pools in direct and indirect fashions in the context of MC–fibroblast interaction.
The contribution of MC-derived sPLA2-III to MC maturation was supported by the observation that the engraftment of BM-derived mast cells (BMMCs; an immature population of MCs) prepared from global Pla2g3-deficient (Pla2g3−/−) mice into KitW-sh mice, which are intrinsically devoid of MCs due to a mutation in the SCF receptor Kit [30], resulted in defective MC maturation [16]. However, since Kit-mutant mice have several phenotypic abnormalities in addition to their MC deficiency [30,31] and since adoptively transferred BMMCs into Kit-mutant mice may not be fully identical (in terms of anatomical location, phenotype, or function) to those in the same anatomical location as in the corresponding wild-type (WT) mice [32,33], the use “MC-specific Cre” mice, which enable us to manipulate a target gene only in MCs, has recently been appreciated. In this study, in order to confirm the role of sPLA2-III expressed in MCs but not in any other cell types that potentially express this enzyme, we generated MC-specific Pla2g3 knockout (KO) mice by crossing Pla2g3-floxed (Pla2g3fl/fl) mice with Mcpt5-Cre mice, which have been used for MC-specific deletion of target genes [34,35,36]. We provide evidence that MC-specific Pla2g3 deficiency fully recapitulates the MC maturation defects as observed in global Pla2g3 deficiency. Additionally, by using MC-specific Pla2g3 KO mice as well as KitW-sh mice adoptively transferred with Pla2g3−/− BMMCs, we addressed the roles of MC-derived sPLA2-III in irritant contact dermatitis (ICD), an acute inflammation, and contact hypersensitivity (CHS), a Th1-dependent delayed-type allergic response.
2. Materials and Methods
2.1. Mice
The targeting vector for the Pla2g3 gene was obtained from the Knockout Mouse Project (KOMP) Repository (clone PRPGS00113_A_H09, Project No. 33384; The Knockout Mouse Project, Mouse Biology Program, University of California, Davis, CA, USA; www.KOMP.org (accessed on 4 April 2011)) [37]. The Pla2g3 conditional-ready mutant allele was generated by KOMP through insertion of the promoter-driven L1L2_Bact_P cassette into the mouse Pla2g3 gene at chromosome 11. The functional gene product is composed of 2 FRT sites flanking an IRES:lacZ-trapping cassette and a floxed human β-actin promoter-driven neo cassette inserted into the intron 1 of the Pla2g3 gene and an additional third loxP site downstream of exon 3. The targeting vector was transferred into C57BL/6 mouse-derived embryonic stem (ES) cells (RENKA; Niigata University, Niigata, Japan) [38] via electroporation, and the cells that contained the correctly targeted Pla2g3 locus were identified by PCR and confirmed by Southern blot analysis. Chimeric mice were generated with the recombinant ES cells using an aggregation method. Two chimeras with higher than ~70% coat color chimerism were mated with C57BL/6N mice (Japan SLC, Shizuoka, Japan) to achieve germline transmission. We then generated a conditional KO mouse strain by crossing heterozygous mice with CAG-Flpe mice (The Jackson Laboratory, Bar Harbor, ME, USA) expressing the flippase recombinase under the control of the actin promoter. This resulted in the excision of the IRES:lacZ and neo cassettes and the generation of a floxed allele. We further crossed conditional KO mice with Mcpt5-Cre mice expressing the Cre recombinase under the control of the MC-specific protease Mcpt5 promoter, generously provided by Dr. Axel Roers (Institute for Immunology, Medical Facility Carl Gustav Carus, University of Technology Dresden, Dresden, Germany) [39], to obtain a null allele. MC-specific Pla2g3 KO (Pla2g3fl/flMcpt5-Cre) mice and control littermates (Pla2g3fl/fl) were used for all animal experiments. Mouse genotypes were determined by PCR of tail-snip DNA using GeneAmp Fast PCR Master Mix (Thermo Fisher Scientific-Applied Biosystems, Waltham, MA, USA) and genotyping primers as follows: forward, 5′-GCGCCATTGCTCGAACTGTGGTTG-3′; reverse, 5′-AGGCCAGGCACAGTCTTTCCTCT-3′.
Global Pla2g3−/− mice were described previously [16,40]. Hpgds−/− mice [41] were provided by Dr. Yoshihiro Urade (Osaka Bioscience Institute, Osaka, Japan). MC-deficient KitW-sh mice (KitW-shHNihrLaeBsmJ, Stock No. 005051) were purchased from the Jackson Laboratory. Age-matched male mice (8–12 weeks of age) were used in each experiment. Mice were maintained in animal facilities in the Tokyo Metropolitan Institute of Medical Science and the University of Tokyo under specific pathogen-free conditions. All animal experiments were approved by the institution and conformed to the Japanese Guide for the Care and Use of Laboratory Animals.
2.2. Maturation and Activation of BMMCs
Mouse BM cells were cultured in Dulbecco’s Modified Eagle Medium (Nissui, Tokyo, Japan) supplemented with 10% (v/v) fetal bovine serum (Thermo Fischer Scientific-gibco), 0.3% (w/v) sodium bicarbonate (Fujifilm Wako, Osaka, Japan), 100 units/mL penicillin, 100 µg/mL streptomycin, 292 µg/mL L-glutamine, 1× nonessential amino acids solution (Thermo Fischer Scientific-gibco), and 10 ng/mL recombinant mouse IL-3, which was obtained by the baculovirus expression system [42]. After 4–6 weeks of culture, >97% of the cells were identified as c-Kit+FcεRIα+ MCs by flow cytometry, as described below.
The fibroblast-directed maturation of immature BMMCs toward connective tissue-type MC (CTMC)-like cells was described previously [16,43,44,45]. Briefly, BMMCs were seeded onto the monolayer of Swiss 3T3 fibroblasts (Japanese Cancer Research Resource Bank, Osaka, Japan) and cocultured for appropriate periods (typically 4 days) in the presence of 100 ng/mL mouse SCF (Peprotech, Cranbury, NJ, USA). The cells were trypsinized and reseeded in culture dishes, and adherent fibroblasts and nonadherent MCs were collected, or pure MCs were isolated using CD117 Microbeads and autoMACS Pro Separator (Miltenyi Biotec, Tokyo, Japan). The maturation of BMMCs into CTMC-like cells was verified by staining of their granules with alcian blue and counterstaining with safranin O (Muto Pure Chemicals, Tokyo, Japan), as described previously [44].
Before or after coculture with 3T3 fibroblasts, 106 BMMCs were preloaded for 2 h with 1 µg/mL anti-dinitrophenyl (DNP) IgE (clone SPE-7, Sigma-Aldrich, St. Louis, MO, USA) in Tyrode’s buffer. After removal of the excess antibody, the cells were stimulated with 100 ng/mL human serum albumin (HSA) conjugated with DNP (DNP-HSA; Sigma-Aldrich) as an Ag for 10 min at 37 °C. As required for experiments, the cells were directly activated by 10 μg/mL Compound 48/80 (C48/80; Sigma-Aldrich), an IgE-independent MC secretagogue. The degree of degranulation was determined by measuring the release of β-hexosaminidase (β-HEX), as described previously [43]. The levels of PGD2 were determined by ELISA in accordance with the manufacturer’s instructions (PGD2-MOX ELISA Kit, Cayman Chemical, Ann Arbor, MI, USA).
2.3. Flow Cytometry
BMMCs were stained with fluorochrome-conjugated monoclonal antibodies specific for CD117/c-Kit (clone 2B8, FITC, BD Biosciences-BD Pharmingen, San Jose, CA, USA) and FcεRIα (clone MAR-1, PE, Thermo Fisher Scientific-eBiosciences). Flow cytometry was performed on a BD FACSAria III flow cytometer (BD Biosciences) and analyzed using FlowJo (LLC, Ashland, OR, USA) software.
2.4. Quantitative RT-PCR
The reagents and instrument required for quantitative RT-PCR were purchased from Thermo Fischer Scientific. Total RNA was isolated from mouse BMMCs, fibroblasts, splenocytes, or ear skin using TRIzol reagent in accordance with the manufacturer’s instruments. First-strand cDNA synthesis was performed using a High-Capacity cDNA Reverse Transcription Kit. Quantitative PCR was performed with a predesigned primer-probe set (TaqMan Gene Expression Assay) and TaqMan Gene Expression Master Mix on a StepOnePlus real-time PCR system. TaqMan Gene Expression Assays for Pla2g3 (Mm01191142_m1), Hpgds (Mm00479846_m1), Ptgds (Mm01330613_m1), Ptgdr (Mm00436050_m1), Hdc (Mm00456104_m1), Mcpt4 (Mm00487636_g1), Mcpt6 (Mm00487645_m1), Kit (Mm00445212_m1), and Ifng (Mm01168134_m1) were used. Expression levels of the transcripts were normalized to Gapdh (Mouse GAPD Endogenous Control) or Kit and fold changes were calculated by the ΔΔCt method. In essence, genes expressed in MCs were normalized with Kit, while those expressed in fibroblasts were normalized with Gapdh, in accordance with our previous paper [16].
2.5. Anaphylaxis
IgE-mediated or C48/80-induced anaphylactic responses were examined as described previously [16,45]. Briefly, in a model of passive cutaneous anaphylaxis (PCA), mouse ears were passively sensitized by subcutaneous injection with 30 ng of anti-DNP IgE monoclonal antibody. On the next day, the mice were challenged by intravenous injection of a mixture of 60 µg of DNP-HSA and 1 mg Evans blue (Fujifilm Wako). In a model of IgE-independent anaphylaxis, mice were intradermally administrated with 250 ng of C48/80 followed by an immediate intravenous injection with Evans blue. Vascular permeability in the mice were measured 30 min after the Ag challenge. The ear tissues were collected and lysed, and amounts of the dye were determined. In a model of passive systemic anaphylaxis (PSA), mice were passively sensitized by intravenous injection with 16.5 µg of anti-DNP IgE. On the next day, the mice were challenged intravenously with 500 µg of DNP-HSA. The rectal temperature was measured over time after Ag challenge with an electronic thermometer (Physitemp Instruments, Clifton, NJ, USA).
2.6. Dermatitis
For an ICD model, mice were directly challenged with 20 µL of 0.3% (v/v) 2,4-dinitrofluorobenzene (DNFB; Sigma-Aldrich) in a vehicle of acetone/olive oil (4:1) to the ear (10 µL to each side). For a CHS model, mice were sensitized on the shaved abdomen with 50 µL of 0.5% (v/v) DNFB. At 5 days after sensitization, mice were challenged with 20 µL of 0.3% (v/v) DNFB to the ear (10 µL to each side), as described previously [46,47]. Ear thickness was measured before and at 4 h in ICD and at several intervals after hapten challenge in CHS with a micrometer (Mitsutoyo, Kanagawa, Japan).
2.7. MC Reconstitution
BMMCs (106) were reconstituted for 6 weeks by intradermal injection into 6-week-old MC-deficient KitW-sh mice [16,30]. The mice were subjected to CHS, as described above. Alternatively, MCs from the base to the tip of the ears from these mice were evaluated histologically by toluidine blue staining, as described below.
2.8. Histology
Ear pinnae from mice were fixed with 10% (v/v) formalin solution and embedded in paraffin, and 4 µm sections were cut and then stained with toluidine blue or hematoxylin and eosin (Merck Millipore, Burlington, MA, USA). For MC quantification, diffuse toluidine blue+ cells with no clearly defined cell membrane indicated MCs.
2.9. Statistical Analysis
Results are presented as box plots with Tukey whiskers or mean ± SEM. Statistical analysis was performed with Prism 9 (GraphPad, San Diego, CA, USA) software. Two-tailed Mann–Whitney test and ordinary one-way or two-way ANOVA with post hoc Tukey multiple comparisons test were performed as noted in the respective figure legends.
3. Results
3.1. Generation of MC-Specific Pla2g3-Deficient Mice
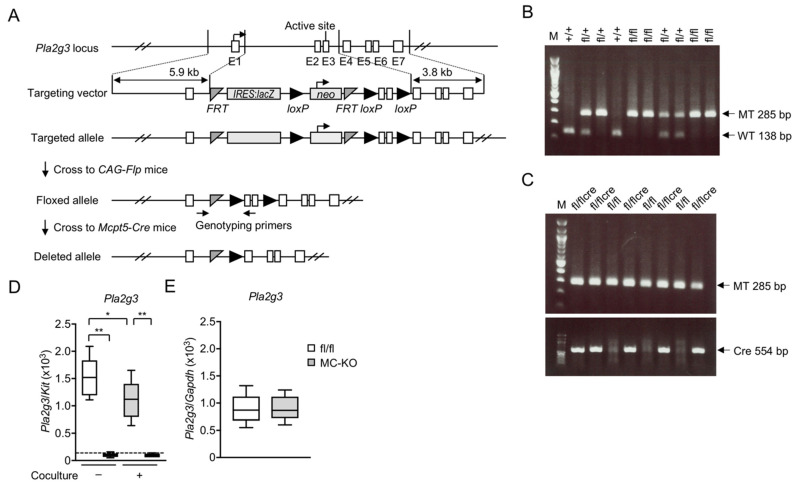
We successfully generated Pla2g3-floxed (Pla2g3fl/fl) mice, in which the exons encompassing the catalytic domain of the Pla2g3 gene were replaced with the IRES:lacZ and neo cassettes and flanked by FRT or loxP sites, for the purpose of conditional inactivation of the gene in a cell- and tissue-specific manner (Figure 1A). To examine the function of Pla2g3 in MCs, we crossed Pla2g3fl/fl mice with Mcpt5-Cre mice [39], which express Cre recombinase selectively in MCs. Mice with conditional deletion of Pla2g3 (Pla2g3fl/flMcpt5-Cre) were screened by genotyping PCR (Figure 1B,C).
Figure 1.
Generation of MC-specific Pla2g3-deficient mice. (A) A schematic representation of the mouse Pla2g3 locus, the targeting vector from KOMP, the targeted Pla2g3 allele with a lacZ/neo cassette, the floxed Pla2g3 allele after removal of the lacZ cassette by flippase, and the Pla2g3-deleted allele after removal of the neo cassette by Cre recombinase. The floxed mice were bred with Mcpt5-Cre mice, and sequences between the two loxP sites were removed from the offspring’s genome in an MC-specific manner. Positions of primers for genotyping are marked with arrows. E1–7 (open boxes), Pla2g3 exons; FRT (gray isosceles triangles), sites for flippase; IRES, internal ribosome entry site; lacZ (gray box), gene encoding β-galactosidase; neo (gray box), neomycin phosphotransferase; loxP sites (black right triangles), target sites for Cre recombinase. Adapted from www.KOMP.org. (B,C) A representative genotyping PCR on agarose gels. The amplified PCR products specific for the floxed allele (MT, 285 bp), WT Pla2g3 allele (WT, 138 bp), and Mcpt5-Cre allele (Cre, 554 bp) are indicated. (D,E) Quantitative RT-PCR of Pla2g3 in BMMCs with (+) or without (−) coculture with 3T3 fibroblasts (n = 6) (D) and splenocytes (n = 8) (E) from Pla2g3fl/fl (fl/fl) and Pla2g3fl/flMcpt-5-Cre mice (MC-KO). The dotted line is the threshold for the detection limit. Data are presented as box plots with Tukey whiskers. *, p < 0.05; **, p < 0.01; one-way ANOVA (D); Mann–Whitney test (E). Data are pooled from 2 independent experiments, each of which gave similar results.
BMMCs represent an immature population of MCs [16,43,44,45]. We took advantage of an in vitro system in which immature BMMCs undergo maturation toward mature CTMC-like cells by coculture with Swiss 3T3 fibroblasts [16,43,44,45]. Mcpt5, encoding an MC-specific protease, was constantly expressed in BMMCs throughout the coculture period [44]. In Pla2g3fl/flMcpt5-Cre mice (fl/flcre in Figure 1C), Pla2g3 expression was largely abrogated in both IL-3-maintained immature BMMCs and cocultured CTMC-like cells (Figure 1D), whereas Pla2g3 was expressed normally in other cells such as splenocytes (Figure 1E), confirming that Cre-mediated recombination efficiently ablated Pla2g3 in MCs.
3.2. MC-Specific Pla2g3 Ablation Impairs MC Maturation
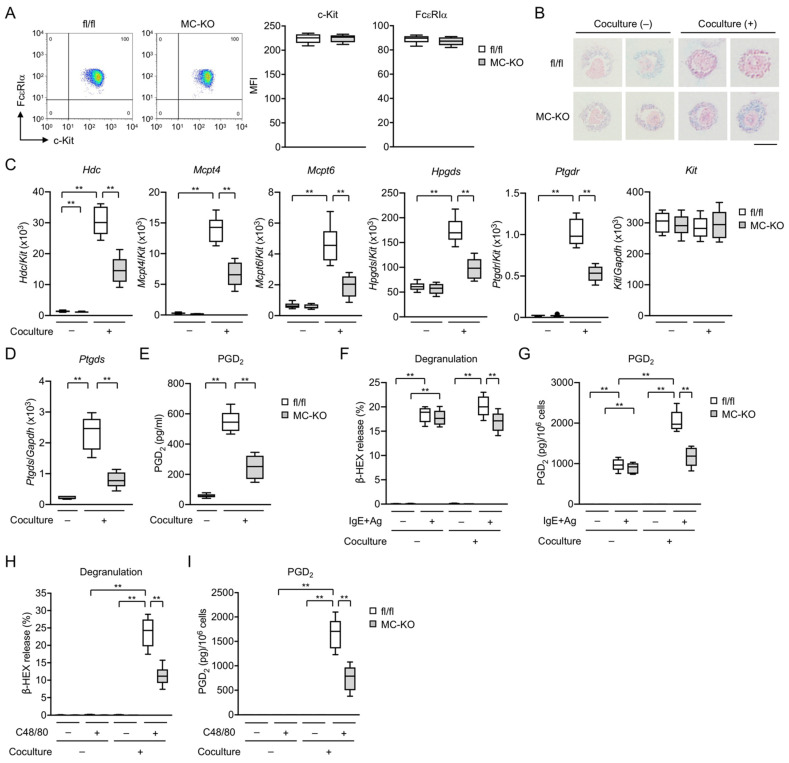
BMMCs prepared from global Pla2g3−/− mice exhibit impaired fibroblast-driven maturation and thereby IgE-dependent and -independent activation in ex vitro culture [16]. To confirm our findings in global Pla2g3−/− mice, we investigated the effects of MC-specific ablation of Pla2g3 on the maturation and activation of BMMCs before and after coculture with Swiss 3T3 fibroblasts. Pla2g3 deficiency in IL-3-maintained BMMCs affected neither proliferation (data not shown), cell surface expression of c-Kit and FcεRIα as assessed by flow cytometry (Figure 2A), nor granule staining with alcian blue (Figure 2B). While Pla2g3fl/fl BMMCs after coculture contained more safranin-positive granules than did the cells before coculture, Pla2g3fl/flMcpt5-Cre BMMCs were stained with safranin only weakly even after coculture (Figure 2B), suggesting immaturity of the granules. The maturation of Pla2g3fl/fl BMMCs to CTMC-like cells resulted in marked induction of Hdc (encoding histidine decarboxylase, a histamine-biosynthetic enzyme), MC-specific proteases Mcpt4 and Mcpt6 (encoding chymase and tryptase, respectively), Hpgds (encoding H-PGDS, which is responsible for PGD2 production in BMMCs but not in fibroblasts), and Ptgdr (encoding DP1, a PGD2 receptor that provides an MC maturation signal) [16]. The induction of these MC maturation markers was markedly impaired, whereas the constitutive expression of Kit was unaffected, in Pla2g3fl/flMcpt5-Cre BMMCs (Figure 2C). In addition, the induction of Ptgds (encoding L-PGDS, which is responsible for PGD2 production in fibroblasts but not in BMMCs) (Figure 2D) and PGD2 production (Figure 2E) were lower in fibroblasts cocultured with Pla2g3fl/flMcpt5-Cre BMMCs than in those cocultured with Pla2g3fl/fl BMMCs, verifying a bidirectional interaction between MCs and fibroblasts.
Figure 2.
Defective fibroblast-directed maturation of MC-specific Pla2g3-null BMMCs. (A) FACS analysis of FcεRIα (vertical axis) and c-Kit (horizontal axis) expression on the surface of BMMCs from Pla2g3fl/fl (fl/fl) and Pla2g3fl/flMcpt5-Cre (MC-KO) mice. Representative FACS profiles and mean fluorescence intensities (MFI) of FcεRIα or c-Kit expression on the cell surface (n = 6) are shown. (B) Alcian blue/safranin staining of BMMCs with (+) or without (−) culture for 4 days with 3T3 fibroblasts. Scale bar, 5 µm. (C) mRNA expression levels for Hdc, Mcpt4, Mcpt6, Hpgds, Ptgdr, and Kit in Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre BMMCs cultured with or without 3T3 fibroblasts (n = 6). (D) Ptgds mRNA levels and (E) PGD2 production in 3T3 fibroblasts cultured with or without Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre BMMCs (n = 6). (F–I) Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre BMMCs cultured with or without 3T3 fibroblasts were sensitized with anti-DNP IgE and then stimulated with DNP-HSA (IgE + Ag), or activated directly with C48/80. Degranulation as assessed by β-HEX release (F,H) and PGD2 production (G,I) were measured 10 min after MC activation (n = 6). Data are compiled from 2 experiments (box plots with Tukey whiskers; **, p < 0.01).
After but not before coculture, FcεRI-dependent release of β-HEX (a degranulation marker) following sensitization with DNP-specific IgE and challenge with DNP-HSA as an Ag was significantly lower in Pla2g3fl/flMcpt5-Cre BMMCs than in Pla2g3fl/fl BMMCs (Figure 2F). Because Hdc expression was markedly reduced in Pla2g3fl/flMcpt5-Cre BMMCs after coculture (Figure 2C), it is likely that histamine synthesis and release were concomitantly reduced in these cells, as seen in global Pla2g3−/− mice [16]. The maturation of Pla2g3fl/fl BMMCs to CTMC-like cells increased IgE-dependent PGD2 synthesis (Figure 2G), with a concomitant increase in Hpgds expression (Figure 2C). However, the coculture-driven elevation of IgE-mediated PGD2 generation occurred only modestly in Pla2g3fl/flMcpt5-Cre cells (Figure 2G), most likely due to the reduced induction of Hpgds (Figure 2C). Although cocultured Pla2g3fl/fl CTMC-like cells acquired sensitivity to C48/80, which acts on mouse Mas-related G protein-coupled receptor B2 (Mrgprb2; the ortholog of human MRGPRX2 [48]), C48/80-induced degranulation and PGD2 production were markedly lower in cocultured Pla2g3fl/flMcpt5-Cre cells (Figure 2H,I). Thus, as in the case of global Pla2g3 deletion [16], MC-specific Pla2g3 deletion impairs fibroblast-directed maturation and thereby IgE-mediated and even -independent activation of BMMCs in ex vitro culture.
3.3. MC-Specific Pla2g3 Ablation Ameliorates MC-Associated Anaphylaxis and Irritant Dermatitis
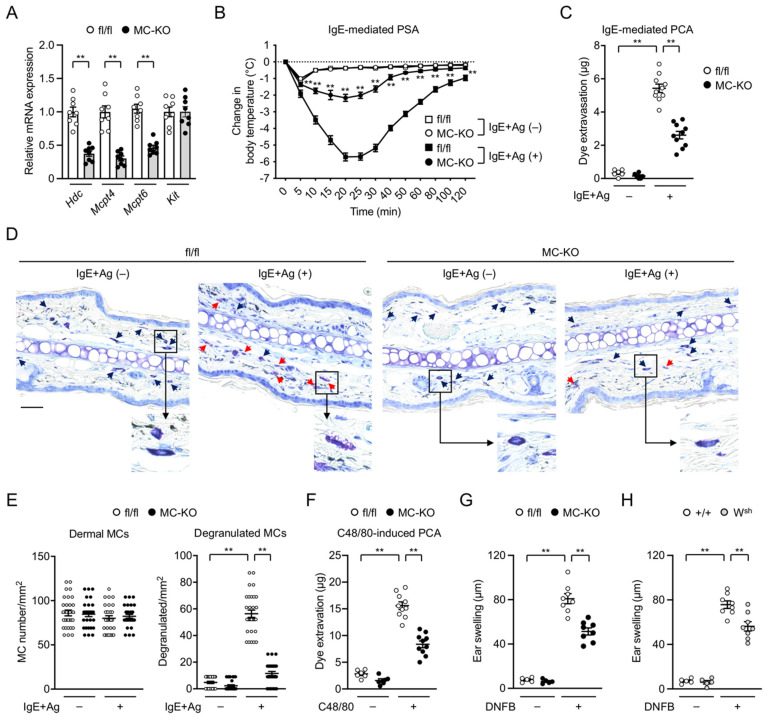
We then evaluated the impacts of MC-specific Pla2g3 deficiency on anaphylactic responses in vivo. In agreement with the ex vivo experiments (Figure 2), the expression levels of Hdc, Mcpt4, and Mcpt6 were notably lower, while that of Kit was unaffected, in the ear skin of Pla2g3fl/flMcpt5-Cre mice relative to Pla2g3fl/fl mice (Figure 3A), confirming the defective MC maturation by the MC-specific absence of sPLA2-III in vivo. To evaluate systemic anaphylaxis, we monitored the changes in body temperature after intravenous injections of Ag-specific IgE followed by that of Ag. Pla2g3fl/fl mice showed a severe transient drop in rectal temperature after systemic Ag challenge, whereas this response was markedly impaired in Pla2g3fl/flMcpt5-Cre mice (Figure 3B). As for local anaphylaxis, mouse ears were injected intradermally with IgE, followed by systemic Ag challenge with Evans blue as an extravasation tracer. Extravasation of the dye in response to Ag challenge was markedly lower in Pla2g3fl/flMcpt5-Cre mice than in Pla2g3fl/fl mice (Figure 3C). Although the ear skin of Pla2g3fl/flMcpt5-Cre and Pla2g3fl/fl mice contained an equivalent number of toluidine blue+ MCs, cells showing signs of Ag-induced degranulation were fewer in Pla2g3fl/flMcpt5-Cre mice than in Pla2g3fl/fl mice (Figure 3D,E).
Figure 3.
Impaired anaphylaxis and irritant dermatitis in MC-specific Pla2g3-deficient mice. (A) Expression of Hdc, Mcpt4, Mcpt6, and Kit in ear skin of Pla2g3fl/fl (fl/fl) and Pla2g3fl/flMcpt5-Cre (MC-KO) mice (n = 8). Gapdh was used as a reference gene for normalization. Expression levels of individual genes in fl/fl were regarded as 1. (B) IgE-mediated PSA. Changes in rectal temperatures over time after challenge with vehicle (IgE + Ag (−), n = 5) or DNP-HSA (IgE + Ag (+), n = 8) in Pla2g3fl/fl (squares) and Pla2g3fl/flMcpt5-Cre (circles) mice. **, p < 0.01 for Pla2g3fl/flMcpt5-Cre mice versus Pla2g3fl/fl mice. (C) IgE-mediated PCA. Dye extravasation 30 min after challenge with vehicle (IgE + Ag (−), n = 5) or DNP-HSA (IgE + Ag (+), n = 10) in Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre mice. (D) Photomicrographs of representative toluidine blue-stained sections of ear pinnae from Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre mice 2 min after vehicle or Ag challenge. Insets show higher magnification of each boxed area. Arrowheads indicate MCs (resting, black arrows; degranulated, red arrows). Scale bar, 25 µm. (E) The number of dermal MCs/mm2 after vehicle or Ag challenge. Thirty views for each group (n = 5). (F) C48/80-induced PCA. Dye extravasation 30 min after administration with vehicle (−, n = 5) or C48/80 (+, n = 10) in Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre mice. (G,H) DNFB-induced ICD. Ear swelling after treatment for 4 h with vehicle (−, n = 5) or DNFB (+, n = 8) in Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre mice (G) or KitW-sh (Wsh) and Kit+/+ (+/+) controls (H). Data, mean ± SEM. **, p < 0.01; (A) two-tailed Mann–Whitney test; (B) two-way and (C,E–H) one-way ANOVA. Data are pooled from 2 independent experiments, each of which gave similar results.
It has recently been shown that ICD requires CTMC activation in a manner dependent on substance P released from nociceptive neurons and MrgprB2 expressed on MCs [49]. MrgprB2 functions as an activating receptor for IgE-independent CTMC degranulation in response to multiple exogenous and endogenous ligands such as C48/80 and substance P [48,49,50,51]. We observed that the IgE-independent, C48/80-induced anaphylactic response was markedly lower in Pla2g3fl/flMcpt5-Cre mice than in Pla2g3fl/fl mice (Figure 3F). Upon ICD, acute ear swelling in response to a single challenge with DNFB was significantly attenuated in Pla2g3fl/flMcpt5-Cre mice compared with Pla2g3fl/fl mice (Figure 3G) as well as in MC-deficient KitW-sh mice compared with Kit+/+ mice (Figure 3H). Collectively, these results indicate that the ablation of Pla2g3 specifically in MCs leads to impaired MC maturation, accompanied by reduced MC-associated anaphylaxis and irritant dermatitis, in vivo.
3.4. MC-Specific Pla2g3 Ablation Excacerbates CHS
The contribution of MCs to CHS, a delayed-type allergic response that depends on Th1 immunity, remains controversial. Indeed, the use of different MC-deficient animals has suggested a positive immunostimulatory role [52,53,54,55,56], a negative immunomodulatory role [35,57,58,59], or no role [60,61,62] of MCs in several CHS models depending on the experimental conditions used. In this study, to evaluate how MC-derived sPLA2-III would contribute to CHS, we subjected MC-specific Pla2g3fl/fl-deficient mice to a model of DNFB-induced CHS.
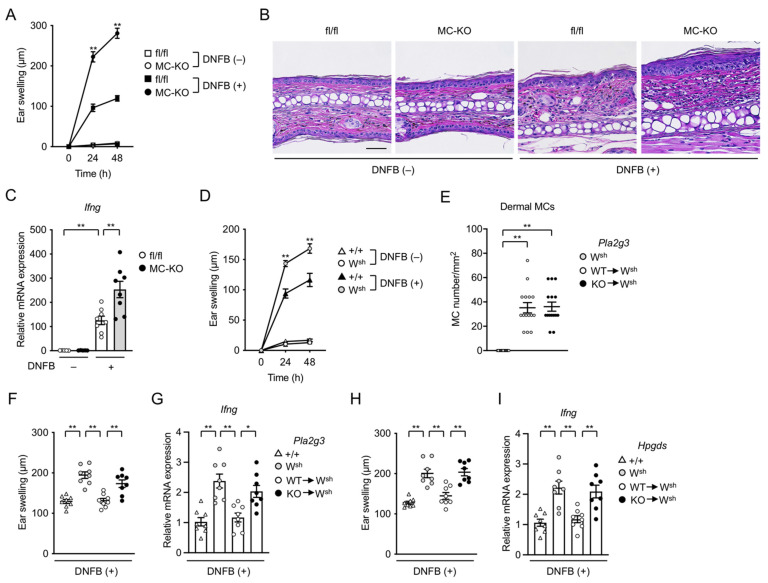
After the second challenge (elicitation) with DNFB, ear swelling was markedly increased in Pla2g3fl/flMcpt5-Cre mice compared to their Pla2g3fl/fl counterparts (Figure 4A). Histological examination of tissue sections revealed that DNFB-induced epidermal and dermal hyperplasia and immune cell recruitment were considerably greater in Pla2g3fl/flMcpt5-Cre mice than in Pla2g3fl/fl mice (Figure 4B). Consistent with the dependence of CHS on IFN-γ-producing CD8+ T cells [63], the DNFB-induced induction of Ifng was higher in the ear of Pla2g3fl/flMcpt5-Cre mice than in that of Pla2g3fl/fl mice (Figure 4C).
Figure 4.
Exacerbated hapten-induced CHS by deficiency of Pla2g3 or Hpgds in MCs. (A) Changes in ear thickness over time after second challenge with vehicle (−, n = 5) or DNFB (+, n = 8) in Pla2g3fl/fl (fl/fl, squares) and Pla2g3fl/flMcpt5-Cre (MC-KO, circles) mice. (B) Representative photomicrographs of sections of ear pinnae in Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre mice sacrificed at 48 h with (+) or without (−) the second DNFB challenge. Scale bar, 25 µm. (C) Expression of Ifng in ear skin of vehicle (n = 5) or DNFB (n = 8)-treated Pla2g3fl/fl and Pla2g3fl/flMcpt5-Cre mice. Gapdh was used as a reference gene for normalization. Expression level in fl/fl without DNFB treatment was regarded as 1. (D) Ear swelling in response to vehicle (n = 5) or DNFB (n = 8) in sensitized KitW-sh (Wsh, circles) and Kit+/+ (+/+, triangles) mice. (E) The number of dermal MCs/mm2 in ear pinnae of KitW-sh mice that had been reconstituted locally with Pla2g3+/+ (WT→Wsh) or Pla2g3−/− (KO→Wsh) BMMCs. Thirty views for each group (n = 5). (F–I) Ear swelling (F,H) and Ifng expression (G,I) in response to the second DNFB challenge in ear skin of Kit+/+ (+/+) and KitW-sh mice that had been reconstituted with or without Pla2g3 WT and Pla2g3 KO BMMCs (F,G) or Hpgds WT and Hpgds KO BMMCs (H,I) (n = 8). In (G,H), expression level of Ifng (normalized to Gapdh) in +/+ was regarded as 1. Data, mean ± SEM; *, p < 0.05; **, p < 0.01; two-way (A,D) and one-way (E–I) ANOVA. Data are pooled from 2 independent experiments performed, each of which gave similar results.
In agreement with previous studies demonstrating the exacerbation of DNFB-induced CHS in MC-deficient KitW-sh mice [55,57,59], KitW-sh mice exhibited greater ear swelling than did MC-sufficient Kit+/+ mice in our CHS settings (Figure 4D). When KitW-sh mice had been intradermally engrafted with BMMCs from global Pla2g3−/− mice or those from WT littermates, the numbers of reconstituted MCs in the ear skin were similar between the two groups (Figure 4E). After reconstitution with WT BMMCs, DNFB-increased ear swelling and Ifng expression in KitW-sh mice were reduced to levels similar to those in Kit+/+ mice, whereas these ameliorating effects were scarcely seen in replicate KitW-sh mice reconstituted with Pla2g3−/− BMMCs (Figure 4F,G). Thus, our present study using two types of MC-specific Pla2g3 deletion models indicates that Pla2g3 in MCs can substantially limit the magnitude of CHS responses.
We have previously shown that sPLA2-III secreted from MCs regulates the spatiotemporal mobilization of distinct PGD2 pools in tissue microenvironments; it is directly coupled with L-PGDS in adjacent fibroblasts to generate a pool of PGD2 that participates in MC maturation, and indirectly affects H-PGDS-driven production of another pool of PGD2 in MCs that counteracts the anaphylactic response [16]. PGD2 can suppress inflammation by limiting neutrophil infiltration, dendritic cell activation, or other mechanisms [24,25,26,27,64]. To assess the possibility that the increased CHS by MC-specific depletion of Pla2g3 might be due to the reduced generation of PGD2, we tested the CHS response in KitW-sh mice engrafted with BMMCs from Hpgds-deficient mice. Although a similar number of MCs was present in the ear of KitW-sh mice that had been reconstituted with Hpgds-sufficient or -deficient BMMCs (data not shown), KitW-sh mice transferred with Hpgds−/− BMMCs, like those transferred with Pla2g3−/− BMMCs (Figure 4F,G), displayed more severe DNFB-induced ear swelling and Ifng induction than replicate KitW-sh mice transferred with WT BMMCs (Figure 4H,I). These results suggest that MC-derived sPLA2-III limits the CHS response at least in part by a mechanism that depends on the promotion of MC maturation and thereby H-PGDS-driven production of anti-inflammatory PGD2.
4. Discussion
Global Pla2g3−/− mice display reduced anaphylactic responses, which could be attributed to impairment of MC maturation [16]. sPLA2-III, which is likely to be secreted from MCs, acts on adjacent fibroblasts as a paracrine factor to promote the biosynthesis of PGD2, an AA-derived lipid mediator that in turn acts on its receptor DP1 on MCs to coordinate proper MC maturation. In this study, using a conditional KO strain in which the Pla2g3 gene is disrupted specifically in MCs under the Mcpt5 promoter, we have provided compelling evidence that MC-derived sPLA2-III is indeed a critical regulator of MC maturation. Although several studies have reported that Mcpt5 is not expressed in all MC populations and recommended to use Cpa3-Cre mice rather than Mcpt5-Cre mice [39,65,66], our present study shows that, as in the case of global Pla2g3 deletion [16], MC-specific Pla2g3 deletion in Pla2g3fl/flMcpt5-Cre mice leads to reduced upregulation of several MC maturation markers, accompanied by decreased degranulation, PGD2 generation, C48/80 sensitivity, and safranin staining, in BMMCs after coculture with fibroblasts ex vivo, as well as reduced IgE-dependent and -independent systemic and local anaphylactic responses in vivo. These results confirm the crucial role of MC-expressed sPLA2-III in the proper maturation of MCs and underline the future use of Pla2g3fl/fl mice to clarify the cell/tissue-specific functions of sPLA2-III in various pathophysiological circumstances.
Our present study has also provided additional insight into the role of MCs in CHS. On the basis of recent research, the roles of MCs in the sensitization and elicitation phases of CHS have been considered as follows: First, during the sensitization phase (which is equivalent to the condition of ICD), MCs are activated directly or indirectly by haptens to release a diverse spectrum of mediators, including histamine and TNF-α, which induce vasodilatation and neutrophil recruitment [53,55]. Consistently, ICD-induced ear swelling, which depends on Mrgprb2 activation [49], is substantially reduced in MC-specific Pla2g3-deficient mice. Interactions between MCs and dendritic cells (DCs) by direct contact or MC-secreted TNF-α can amplify DC migration into the draining lymph nodes, where DCs prime naïve T cells to become effector T cells via Ag presentation [67]. Second, during moderate CHS responses, MCs amplify ear swelling, epidermal hyperplasia, and recruitment of neutrophils and CD8+ T cells through releasing TNF-α [34]. Third, during more severe CHS responses, MCs represent an early source of IL-10, which amplifies subsequent recruitment of regulatory T (Treg) cells and limits ear swelling and epidermal hyperplasia [35,57]. Additionally, MCs can migrate into lymphoid organs, where they produce IL-2, which contributes to maintaining Treg cells and thereby ameliorating CHS [58]. The CHS model employed in the present study fits with the third case, where MCs limit the severity of CHS inflammation. Importantly, the absence of sPLA2-III in MCs dampens the suppressive effect of these cells on ear swelling and Ifng induction in CHS, revealing a novel role of this particular sPLA2 in a specific pathological event. This function appears to depend at least partly on the sPLA2-III-driven, indirect mobilization of PGD2 by MCs, where MC-derived sPLA2-III is coupled with L-PGDS-dependent production of the first pool of PGD2 in fibroblasts, which then facilitates the proper maturation of MCs and thereby H-PGDS-dependent production of the second pool of PGD2 by these cells. Indeed, Hpgds deficiency in MCs also abrogates the suppressive effect of MCs on CHS, highlighting that, in addition to the cytokines IL-2 and IL-10 [33,35,57,58], the lipid mediator PGD2 acts as another negative modulator of the CHS responses. In support of this view, mice lacking DP1 (Ptgdr−/−) also display an exacerbation of CHS by affecting the expression of IL-10 in DCs [26].
Individual sPLA2s exhibit unique tissue or cellular distributions and enzymatic properties and exert their specific functions by producing lipid mediators; by altering membrane phospholipid composition; by degrading foreign phospholipids from microorganisms or diet; or by modifying extracellular noncellular lipid compounds such as lipoproteins, pulmonary surfactant, or extracellular vesicles in response to given microenvironmental cues [68,69,70,71]. Currently, two sPLA2 isoforms have been reported to participate in the regulation of CHS. sPLA2-IID, which is expressed in lymph node DCs, protects against CHS by putting a brake on Th1 immunity through mobilization of ω3 polyunsaturated fatty acids and their anti-inflammatory/proresolving metabolites [46]. sPLA2-IIF, which is expressed in keratinocytes, exacerbates CHS by facilitating epidermal hyperplasia through the generation of a unique lysophospholipid [47]. The present study showing that sPLA2-III in MCs plays a role in limiting CHS by mobilizing anti-inflammatory PGD2 in a feed-forward loop of MC–fibroblast communication represents the third example of the sPLA2-mediated regulation of CHS, further highlighting the diverse functions of individual sPLA2 isoforms in mobilizing distinct lipids in different cells and tissues.
Acknowledgments
We thank Axel Roers (Institute for Immunology, Medical Facility Carl Gustav Carus, University of Technology Dresden, Dresden, Germany) for providing the Mcpt5-Cre mice and Kenji Sakimura (Department of Animal Model Development, Brain Research Institute, Niigata University, Niigata, Japan) for providing RENKA ES cells.
Author Contributions
Y.T. and M.M. designed and interpreted experiments; Y.T., Y.E. and T.H. performed experiments; T.O. and C.T. generated Pla2g3 conditional knockout mice; R.M. and T.K. provided technical and conceptual assistance; Y.T. and M.M. wrote the manuscript, and all authors edited it. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Grants-in-Aid for Scientific Research JP18K06624, JP16K15122 (to Y.T.), JP20H05691, and JP20H04939 (to M.M.) from Japan Society for the Promotion of Science; AMED-CREST 18gm0710006 and 21gm1210013 (to M.M.) and FORCE 20gm4010005 (to M.M.) from the Japan Agency for Medical Research and Development; Takeda Science Foundation; and the Naito Foundation, Japan.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Tokyo Metropolitan Institute of Medical Science and the University of Tokyo under the Japanese Guide for the Care and Use of Laboratory Animals.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Galli S.J., Grimbaldeston M., Tsai M. Immunomodulatory mast cells: Negative, as well as positive, regulators of immunity. Nat. Rev. Immunol. 2008;8:478–486. doi: 10.1038/nri2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galli S.J., Tsai M. IgE and mast cells in allergic disease. Nat. Med. 2012;18:693–704. doi: 10.1038/nm.2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galli S.J., Gaudenzio N., Tsai M. Mast cells in inflammation and disease: Recent progress and ongoing concerns. Annu. Rev. Immunol. 2020;38:49–77. doi: 10.1146/annurev-immunol-071719-094903. [DOI] [PubMed] [Google Scholar]
- 4.Boyce J.A. Mast cells and eicosanoid mediators: A system of reciprocal paracrine and autocrine regulation. Immunol. Rev. 2007;217:168–185. doi: 10.1111/j.1600-065X.2007.00512.x. [DOI] [PubMed] [Google Scholar]
- 5.Metcalfe D.D., Baram D., Mekori Y.A. Mast cells. Physiol. Rev. 1997;77:1033–1079. doi: 10.1152/physrev.1997.77.4.1033. [DOI] [PubMed] [Google Scholar]
- 6.Olivera A., Beaven M.A., Metcalfe D.D. Mast cells signal their importance in health and disease. J. Allergy Clin. Immunol. 2018;142:381–393. doi: 10.1016/j.jaci.2018.01.034. [DOI] [PubMed] [Google Scholar]
- 7.Gilfillan A.M., Beaven M.A. Regulation of mast cell responses in health and disease. Crit. Rev. Immunol. 2011;31:475–529. doi: 10.1615/CritRevImmunol.v31.i6.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gurish M.F., Austen K.F. Developmental origin and functional specialization of mast cell subsets. Immunity. 2012;37:25–33. doi: 10.1016/j.immuni.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Hallgren J., Gurish M.F. Mast cell progenitor trafficking and maturation. Adv. Exp. Med. Biol. 2011;716:14–28. doi: 10.1007/978-1-4419-9533-9_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kitamura Y. Heterogeneity of mast cells and phenotypic change between subpopulations. Annu. Rev. Immunol. 1989;7:59–76. doi: 10.1146/annurev.iy.07.040189.000423. [DOI] [PubMed] [Google Scholar]
- 11.Gentek R., Ghigo C., Hoeffel G., Bulle M.J., Msallam R., Gautier G., Launay P., Chen J., Ginhoux F., Bajenoff M. Hemogenic endothelial fate mapping reveals dual developmental origin of mast cells. Immunity. 2018;48:1160–1171.e5. doi: 10.1016/j.immuni.2018.04.025. [DOI] [PubMed] [Google Scholar]
- 12.Li Z., Liu S., Xu J., Zhang X., Han D., Liu J., Xia M., Yi L., Shen Q., Xu S., et al. Adult connective tissue-resident mast cells originate from late erythro-myeloid progenitors. Immunity. 2018;49:640–653.e5. doi: 10.1016/j.immuni.2018.09.023. [DOI] [PubMed] [Google Scholar]
- 13.Dahlin J.S., Hallgren J. Mast cell progenitors: Origin, development and migration to tissues. Mol. Immunol. 2015;63:9–17. doi: 10.1016/j.molimm.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 14.Kitamura Y., Oboki K., Ito A. Development of mast cells. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2007;83:164–174. doi: 10.2183/pjab.83.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hallgren J., Gurish M.F. Pathways of murine mast cell development and trafficking: Tracking the roots and routes of the mast cell. Immunol. Rev. 2007;217:8–18. doi: 10.1111/j.1600-065X.2007.00502.x. [DOI] [PubMed] [Google Scholar]
- 16.Taketomi Y., Ueno N., Kojima T., Sato H., Murase R., Yamamoto K., Tanaka S., Sakanaka M., Nakamura M., Nishito Y., et al. Mast cell maturation is driven via a group III phospholipase A2-prostaglandin D2-DP1 receptor paracrine axis. Nat. Immunol. 2013;14:554–563. doi: 10.1038/ni.2586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murakami M. Lipoquality control by phospholipase A2 enzymes. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2017;93:677–702. doi: 10.2183/pjab.93.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murakami M., Taketomi Y., Miki Y., Sato H., Hirabayashi T., Yamamoto K. Recent progress in phospholipase A2 research: From cells to animals to humans. Prog. Lipid Res. 2011;50:152–192. doi: 10.1016/j.plipres.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Fujishima H., Sanchez Mejia R.O., Bingham C.O., 3rd, Lam B.K., Sapirstein A., Bonventre J.V., Austen K.F., Arm J.P. Cytosolic phospholipase A2 is essential for both the immediate and the delayed phases of eicosanoid generation in mouse bone marrow-derived mast cells. Proc. Natl. Acad. Sci. USA. 1999;96:4803–4807. doi: 10.1073/pnas.96.9.4803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakatani N., Uozumi N., Kume K., Murakami M., Kudo I., Shimizu T. Role of cytosolic phospholipase A2 in the production of lipid mediators and histamine release in mouse bone-marrow-derived mast cells. Biochem. J. 2000;352:311–317. doi: 10.1042/bj3520311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murakami M., Taketomi Y. Secreted phospholipase A2 and mast cells. Allergol. Int. 2015;64:4–10. doi: 10.1016/j.alit.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 22.Matsuoka T., Hirata M., Tanaka H., Takahashi Y., Murata T., Kabashima K., Sugimoto Y., Kobayashi T., Ushikubi F., Aze Y., et al. Prostaglandin D2 as a mediator of allergic asthma. Science. 2000;287:2013–2017. doi: 10.1126/science.287.5460.2013. [DOI] [PubMed] [Google Scholar]
- 23.Spik I., Brenuchon C., Angeli V., Staumont D., Fleury S., Capron M., Trottein F., Dombrowicz D. Activation of the prostaglandin D2 receptor DP2/CRTH2 increases allergic inflammation in mouse. J. Immunol. 2005;174:3703–3708. doi: 10.4049/jimmunol.174.6.3703. [DOI] [PubMed] [Google Scholar]
- 24.Trivedi S.G., Newson J., Rajakariar R., Jacques T.S., Hannon R., Kanaoka Y., Eguchi N., Colville-Nash P., Gilroy D.W. Essential role for hematopoietic prostaglandin D2 synthase in the control of delayed type hypersensitivity. Proc. Natl. Acad. Sci. USA. 2006;103:5179–5184. doi: 10.1073/pnas.0507175103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hammad H., Kool M., Soullie T., Narumiya S., Trottein F., Hoogsteden H.C., Lambrecht B.N. Activation of the D prostanoid 1 receptor suppresses asthma by modulation of lung dendritic cell function and induction of regulatory T cells. J. Exp. Med. 2007;204:357–367. doi: 10.1084/jem.20061196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yamamoto Y., Otani S., Hirai H., Nagata K., Aritake K., Urade Y., Narumiya S., Yokozeki H., Nakamura M., Satoh T. Dual functions of prostaglandin D2 in murine contact hypersensitivity via DP and CRTH2. Am. J. Pathol. 2011;179:302–314. doi: 10.1016/j.ajpath.2011.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakamura T., Maeda S., Horiguchi K., Maehara T., Aritake K., Choi B.I., Iwakura Y., Urade Y., Murata T. PGD2 deficiency exacerbates food antigen-induced mast cell hyperplasia. Nat. Commun. 2015;6:7514. doi: 10.1038/ncomms8514. [DOI] [PubMed] [Google Scholar]
- 28.Lambeau G., Gelb M.H. Biochemistry and physiology of mammalian secreted phospholipases A2. Annu. Rev. Biochem. 2008;77:495–520. doi: 10.1146/annurev.biochem.76.062405.154007. [DOI] [PubMed] [Google Scholar]
- 29.Valentin E., Ghomashchi F., Gelb M.H., Lazdunski M., Lambeau G. Novel human secreted phospholipase A2 with homology to the group III bee venom enzyme. J. Biol. Chem. 2000;275:7492–7496. doi: 10.1074/jbc.275.11.7492. [DOI] [PubMed] [Google Scholar]
- 30.Grimbaldeston M.A., Chen C.C., Piliponsky A.M., Tsai M., Tam S.Y., Galli S.J. Mast cell-deficient W-sash c-kit mutant KitW-sh/W-sh mice as a model for investigating mast cell biology in vivo. Am. J. Pathol. 2005;167:835–848. doi: 10.1016/S0002-9440(10)62055-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nigrovic P.A., Gray D.H., Jones T., Hallgren J., Kuo F.C., Chaletzky B., Gurish M., Mathis D., Benoist C., Lee D.M. Genetic inversion in mast cell-deficient Wsh mice interrupts corin and manifests as hematopoietic and cardiac aberrancy. Am. J. Pathol. 2008;173:1693–1701. doi: 10.2353/ajpath.2008.080407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reber L.L., Marichal T., Galli S.J. New models for analyzing mast cell functions in vivo. Trends Immunol. 2012;33:613–625. doi: 10.1016/j.it.2012.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gaudenzio N., Marichal T., Galli S.J., Reber L.L. Genetic and imaging approaches reveal pro-inflammatory and immunoregulatory roles of mast cells in contact hypersensitivity. Front. Immunol. 2018;9:1275. doi: 10.3389/fimmu.2018.01275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dudeck J., Ghouse S.M., Lehmann C.H., Hoppe A., Schubert N., Nedospasov S.A., Dudziak D., Dudeck A. Mast-cell-derived TNF amplifies CD8+ dendritic cell functionality and CD8+ T cell priming. Cell Rep. 2015;13:399–411. doi: 10.1016/j.celrep.2015.08.078. [DOI] [PubMed] [Google Scholar]
- 35.Reber L.L., Sibilano R., Starkl P., Roers A., Grimbaldeston M.A., Tsai M., Gaudenzio N., Galli S.J. Imaging protective mast cells in living mice during severe contact hypersensitivity. JCI Insight. 2017;2 doi: 10.1172/jci.insight.92900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Y., Liu B., Harmacek L., Long Z., Liang J., Lukin K., Leach S.M., O’Connor B., Gerber A.N., Hagman J., et al. The transcription factors GATA2 and microphthalmia-associated transcription factor regulate Hdc gene expression in mast cells and are required for IgE/mast cell-mediated anaphylaxis. J. Allergy Clin. Immunol. 2018;142:1173–1184. doi: 10.1016/j.jaci.2017.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Skarnes W.C., Rosen B., West A.P., Koutsourakis M., Bushell W., Iyer V., Mujica A.O., Thomas M., Harrow J., Cox T., et al. A conditional knockout resource for the genome-wide study of mouse gene function. Nature. 2011;474:337–342. doi: 10.1038/nature10163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mishina M., Sakimura K. Conditional gene targeting on the pure C57BL/6 genetic background. Neurosci. Res. 2007;58:105–112. doi: 10.1016/j.neures.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 39.Scholten J., Hartmann K., Gerbaulet A., Krieg T., Muller W., Testa G., Roers A. Mast cell-specific Cre/loxP-mediated recombination in vivo. Transgenic Res. 2008;17:307–315. doi: 10.1007/s11248-007-9153-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sato H., Taketomi Y., Isogai Y., Miki Y., Yamamoto K., Masuda S., Hosono T., Arata S., Ishikawa Y., Ishii T., et al. Group III secreted phospholipase A2 regulates epididymal sperm maturation and fertility in mice. J. Clin. Invest. 2010;120:1400–1414. doi: 10.1172/JCI40493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mohri I., Taniike M., Taniguchi H., Kanekiyo T., Aritake K., Inui T., Fukumoto N., Eguchi N., Kushi A., Sasai H., et al. Prostaglandin D2-mediated microglia/astrocyte interaction enhances astrogliosis and demyelination in twitcher. J. Neurosci. 2006;26:4383–4393. doi: 10.1523/JNEUROSCI.4531-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murakami M., Matsumoto R., Austen K.F., Arm J.P. Prostaglandin endoperoxide synthase-1 and -2 couple to different transmembrane stimuli to generate prostaglandin D2 in mouse bone marrow-derived mast cells. J. Biol. Chem. 1994;269:22269–22275. doi: 10.1016/S0021-9258(17)31786-6. [DOI] [PubMed] [Google Scholar]
- 43.Ogasawara T., Murakami M., Suzuki-Nishimura T., Uchida M.K., Kudo I. Mouse bone marrow-derived mast cells undergo exocytosis, prostanoid generation, and cytokine expression in response to G protein-activating polybasic compounds after coculture with fibroblasts in the presence of c-kit ligand. J. Immunol. 1997;158:393–404. [PubMed] [Google Scholar]
- 44.Taketomi Y., Sugiki T., Saito T., Ishii S., Hisada M., Suzuki-Nishimura T., Uchida M.K., Moon T.C., Chang H.W., Natori Y., et al. Identification of NDRG1 as an early inducible gene during in vitro maturation of cultured mast cells. Biochem. Biophys. Res. Commun. 2003;306:339–346. doi: 10.1016/S0006-291X(03)00942-2. [DOI] [PubMed] [Google Scholar]
- 45.Taketomi Y., Sunaga K., Tanaka S., Nakamura M., Arata S., Okuda T., Moon T.C., Chang H.W., Sugimoto Y., Kokame K., et al. Impaired mast cell maturation and degranulation and attenuated allergic responses in Ndrg1-deficient mice. J. Immunol. 2007;178:7042–7053. doi: 10.4049/jimmunol.178.11.7042. [DOI] [PubMed] [Google Scholar]
- 46.Miki Y., Yamamoto K., Taketomi Y., Sato H., Shimo K., Kobayashi T., Ishikawa Y., Ishii T., Nakanishi H., Ikeda K., et al. Lymphoid tissue phospholipase A2 group IID resolves contact hypersensitivity by driving antiinflammatory lipid mediators. J. Exp. Med. 2013;210:1217–1234. doi: 10.1084/jem.20121887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yamamoto K., Miki Y., Sato M., Taketomi Y., Nishito Y., Taya C., Muramatsu K., Ikeda K., Nakanishi H., Taguchi R., et al. The role of group IIF-secreted phospholipase A2 in epidermal homeostasis and hyperplasia. J. Exp. Med. 2015;212:1901–1919. doi: 10.1084/jem.20141904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McNeil B.D., Pundir P., Meeker S., Han L., Undem B.J., Kulka M., Dong X. Identification of a mast-cell-specific receptor crucial for pseudo-allergic drug reactions. Nature. 2015;519:237–241. doi: 10.1038/nature14022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang S., Edwards T.N., Chaudhri V.K., Wu J., Cohen J.A., Hirai T., Rittenhouse N., Schmitz E.G., Zhou P.Y., McNeil B.D., et al. Nonpeptidergic neurons suppress mast cells via glutamate to maintain skin homeostasis. Cell. 2021;184:2151–2166.e16. doi: 10.1016/j.cell.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Serhan C.N., Levy B.D. Resolvins in inflammation: Emergence of the pro-resolving superfamily of mediators. J. Clin. Invest. 2018;128:2657–2669. doi: 10.1172/JCI97943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Green D.P., Limjunyawong N., Gour N., Pundir P., Dong X. A mast-cell-specific receptor mediates neurogenic inflammation and pain. Neuron. 2019;101:412–420.e3. doi: 10.1016/j.neuron.2019.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Askenase P.W., Van Loveren H., Kraeuter-Kops S., Ron Y., Meade R., Theoharides T.C., Nordlund J.J., Scovern H., Gerhson M.D., Ptak W. Defective elicitation of delayed-type hypersensitivity in W/Wv and SI/SId mast cell-deficient mice. J. Immunol. 1983;131:2687–2694. [PubMed] [Google Scholar]
- 53.Biedermann T., Kneilling M., Mailhammer R., Maier K., Sander C.A., Kollias G., Kunkel S.L., Hultner L., Rocken M. Mast cells control neutrophil recruitment during T cell-mediated delayed-type hypersensitivity reactions through tumor necrosis factor and macrophage inflammatory protein 2. J. Exp. Med. 2000;192:1441–1452. doi: 10.1084/jem.192.10.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bryce P.J., Miller M.L., Miyajima I., Tsai M., Galli S.J., Oettgen H.C. Immune sensitization in the skin is enhanced by antigen-independent effects of IgE. Immunity. 2004;20:381–392. doi: 10.1016/S1074-7613(04)00080-9. [DOI] [PubMed] [Google Scholar]
- 55.Dudeck A., Dudeck J., Scholten J., Petzold A., Surianarayanan S., Kohler A., Peschke K., Vohringer D., Waskow C., Krieg T., et al. Mast cells are key promoters of contact allergy that mediate the adjuvant effects of haptens. Immunity. 2011;34:973–984. doi: 10.1016/j.immuni.2011.03.028. [DOI] [PubMed] [Google Scholar]
- 56.Otsuka A., Kubo M., Honda T., Egawa G., Nakajima S., Tanizaki H., Kim B., Matsuoka S., Watanabe T., Nakae S., et al. Requirement of interaction between mast cells and skin dendritic cells to establish contact hypersensitivity. PLoS ONE. 2011;6:e25538. doi: 10.1371/journal.pone.0025538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Grimbaldeston M.A., Nakae S., Kalesnikoff J., Tsai M., Galli S.J. Mast cell-derived interleukin 10 limits skin pathology in contact dermatitis and chronic irradiation with ultraviolet B. Nat. Immunol. 2007;8:1095–1104. doi: 10.1038/ni1503. [DOI] [PubMed] [Google Scholar]
- 58.Hershko A.Y., Suzuki R., Charles N., Alvarez-Errico D., Sargent J.L., Laurence A., Rivera J. Mast cell interleukin-2 production contributes to suppression of chronic allergic dermatitis. Immunity. 2011;35:562–571. doi: 10.1016/j.immuni.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gimenez-Rivera V.A., Siebenhaar F., Zimmermann C., Siiskonen H., Metz M., Maurer M. Mast cells limit the exacerbation of chronic allergic contact dermatitis in response to repeated allergen exposure. J. Immunol. 2016;197:4240–4246. doi: 10.4049/jimmunol.1600236. [DOI] [PubMed] [Google Scholar]
- 60.Galli S.J., Hammel I. Unequivocal delayed hypersensitivity in mast cell-deficient and beige mice. Science. 1984;226:710–713. doi: 10.1126/science.6494907. [DOI] [PubMed] [Google Scholar]
- 61.Mekori Y.A., Galli S.J. Undiminished immunologic tolerance to contact sensitivity in mast cell-deficient W/Wv and Sl/Sld mice. J. Immunol. 1985;135:879–885. [PubMed] [Google Scholar]
- 62.Mekori Y.A., Chang J.C., Wershil B.K., Galli S.J. Studies of the role of mast cells in contact sensitivity responses. Passive transfer of the reaction into mast cell-deficient mice locally reconstituted with cultured mast cells: Effect of reserpine on transfer of the reaction with DNP-specific cloned T cells. Cell. Immunol. 1987;109:39–52. doi: 10.1016/0008-8749(87)90290-5. [DOI] [PubMed] [Google Scholar]
- 63.Xu H., DiIulio N.A., Fairchild R.L. T cell populations primed by hapten sensitization in contact sensitivity are distinguished by polarized patterns of cytokine production: Interferon gamma-producing (Tc1) effector CD8+ T cells and interleukin (Il) 4/Il-10-producing (Th2) negative regulatory CD4+ T cells. J. Exp. Med. 1996;183:1001–1012. doi: 10.1084/jem.183.3.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Levy B.D., Clish C.B., Schmidt B., Gronert K., Serhan C.N. Lipid mediator class switching during acute inflammation: Signals in resolution. Nat. Immunol. 2001;2:612–619. doi: 10.1038/89759. [DOI] [PubMed] [Google Scholar]
- 65.Wei Y., Chhiba K.D., Zhang F., Ye X., Wang L., Zhang L., Robida P.A., Moreno-Vinasco L., Schnaar R.L., Roers A., et al. Mast cell-specific expression of human Siglec-8 in conditional knock-in mice. Int. J. Mol. Sci. 2018;20:19. doi: 10.3390/ijms20010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lilla J.N., Chen C.C., Mukai K., BenBarak M.J., Franco C.B., Kalesnikoff J., Yu M., Tsai M., Piliponsky A.M., Galli S.J. Reduced mast cell and basophil numbers and function in Cpa3-Cre; Mcl-1fl/fl mice. Blood. 2011;118:6930–6938. doi: 10.1182/blood-2011-03-343962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Suto H., Nakae S., Kakurai M., Sedgwick J.D., Tsai M., Galli S.J. Mast cell-associated TNF promotes dendritic cell migration. J. Immunol. 2006;176:4102–4112. doi: 10.4049/jimmunol.176.7.4102. [DOI] [PubMed] [Google Scholar]
- 68.Murakami M., Sato H., Miki Y., Yamamoto K., Taketomi Y. A new era of secreted phospholipase A2. J. Lipid Res. 2015;56:1248–1261. doi: 10.1194/jlr.R058123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Murakami M., Yamamoto K., Miki Y., Murase R., Sato H., Taketomi Y. The roles of the secreted phospholipase A2 gene family in immunology. Adv. Immunol. 2016;132:91–134. doi: 10.1016/bs.ai.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Murakami M., Miki Y., Sato H., Murase R., Taketomi Y., Yamamoto K. Group IID, IIE, IIF and III secreted phospholipase A2s. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2019;1864:803–818. doi: 10.1016/j.bbalip.2018.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Murakami M., Sato H., Taketomi Y. Updating phospholipase A2 biology. Biomolecules. 2020;10:1457. doi: 10.3390/biom10101457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.