Abstract
Background
Scarcity of data on the health impacts and associated economic costs of heat waves may limit the will to invest in adaptation measures. We assessed the economic impact associated with mortality, morbidity, and loss of well-being during heat waves in France between 2015 and 2019.
Methods
Health indicators monitored by the French national heat wave plan were used to estimate excess visits to emergency rooms and outpatient clinics and hospitalizations for heat-related causes. Total excess mortality and years of life loss were considered, as well as the size of the population that experienced restricted activity. A cost-of-illness and willingness-to-pay approach was used to account for associated costs.
Results
Between 2015 and 2019, the economic impact of selected health effects of heat waves amounts to €25.5 billion, mainly in mortality (€23.2 billion), minor restricted activity days (€2.3 billion), and morbidity (€0.031 billion).
Conclusion
The results highlight a significant economic burden on the French health system and the population. A better understanding of the economic impacts of climate change on health is required to alert decision-makers to the urgency of mitigation and to support concrete adaptation actions.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10198-021-01357-2.
Keywords: Extreme heat, Heat-related illness, Mortality, Economic assessment, Climate change
Introduction
Extreme weather events are among the most direct consequences of climate change [1]. Assessing their economic impacts is challenging, and often the economic valuation only covers the direct consequences on infrastructures, with some additional consideration of the indirect socio-economic impacts. These impacts were found to represent between $94 and $130 billion each year between 2000 and 2012 worldwide, but health impacts and the associated economic burden were reportedly seldom studied [2].
The frequency, intensity, and duration of heat waves are increasing rapidly [1], making adaptation to heat a priority. However, although they are among the deadliest extreme events [3], they are under-represented in the total estimated economic burden of extreme weather events, for several reasons. First, because they are less visible, being more widespread and leading to less easily identifiable deaths than those from hurricanes, floods or wildfires. Second, because they are apparently less costly to society due to their limited impact on insured goods like infrastructures, cultures, and property [4]. Third, because they often hit the most vulnerable segments of the population (the poorest or the oldest), with lower economic impact and visibility, both worldwide and within a specific country [5]. Few studies have focused on estimating the economic burden associated with heat waves (see [6, 7] for recent reviews). The August 2003 record-breaking heat wave led to about 70,000 deaths in Europe [8] and 15,000 in France [9]. The associated direct morbidity and mortality-related medical costs borne by the French National Health Insurance system were estimated at between €10 and €280 million [10], but this did not account for the health-related and intangible effects supported by the population. These intangible effects represent the loss of well-being and quality of life associated with a health event for the patient and his or her family (grief, fear, pain, stress, lost time, etc.) and are not easily measurable in monetary costs. The scarcity of data on the actual health impacts and associated economic costs of heat waves, coupled with low heat-related risk perception among stakeholders, may limit the will to invest in adaptation.
To fill this gap, we performed the first overall assessment of the health-related economic burden of heat waves from 2015 to 2019 in France. We not only considered excess mortality and morbidity based on epidemiological data, which is standard, but also tackled two more rarely addressed issues. First, we evaluated loss of well-being under exposure to heat waves, due to restrictions in daily activities and symptoms such as fatigue, cramps, heat stroke, decreased alertness and cognitive function. Second, we jointly assessed epidemiological and economic uncertainties in an integrated approach. Overall, taking a global perspective on health impacts and economic burden and an innovative methodological approach, our paper contributes to the scanty literature on health effects observed during heat waves. In the discussion, we point out that these health-related effects are largely preventable through cost-beneficial measures, from the most local to the most global level, making inaction absurdly wasteful. This provides support for the approaches of Sheehan et al. [11] or Limaye et al. [4] to how health-cost assessment can be applied to health-protective heat policy, with the aim of making decision-makers aware of the urgency of prioritizing measures to prevent the adverse health consequences of climate change.
Methods
This study was conducted in the 96 metropolitan French departments for the period 2015–2019. Computations were made at the department level and then aggregated at national level. A negative number of excess cases was assumed to represent an absence of heat effect. Consequently, any negative health effect at the department level is set to 0 when computing the health impact and the economic evaluation at the national level. We used the definitions, databases, and indicators developed within the French national heat wave plan to assess the heath burden of heat waves, as described below [12, 13].
Heat wave definition and warning levels
Daily minimum and maximum temperatures were obtained from the French National Meteorological Service (Météo France). Heat waves were defined as periods when the average minimum and maximum temperatures over three consecutive days exceeded predefined departmental thresholds [14]. Within the French heat action plan, each department and each day is classified by Météo-France as green, yellow, orange, and red. Orange and red levels exceed the thresholds defined above (i.e., indicate heat waves), while the yellow level indicates an intermediate situation (e.g., slightly below the thresholds), and the green level absence of risk. All but three departments experienced at least one heat wave over the study period, and many departments underwent several heat waves per summer. The size of the population exposed to each warning level is provided daily [13].
Estimation of health impacts from heat waves
Morbidity
Daily emergency department (ED) visits and outpatient clinic visits (SOS Médecins) were obtained for each department from the French syndromic surveillance system (SurSaUD®). The database provides detailed information such as age, sex, diagnosis, whether the visit led to hospitalization, and covers approximately 93% of ED visits and 95% of outpatient clinic visits in France. We selected visits involving at least one of the heat-related adverse effects: faintness, hyponatremia, hyperthermia, heat stroke, isolated fever, and/or dehydration [15, 16]. Three age groups were considered (0–14, 15–64, 65 and older).
The morbidity impacts were computed strictly for the heat wave periods because of their immediate health impact in terms of adverse effects. We used quasi-Poisson models to assess the daily number of expected cases per age group in the absence of heat waves, and controlled for day of week, month, and year. The total numbers of ED and outpatient clinic visits recorded were also included as an offset to control for a possible confounding effect from variations in the volume of activity and coding quality over time. Morbidity data are highly dependent on the number of hospitals and SOS Médecins emergency care associations reporting daily data.
Excess morbidity during heat waves was estimated at the department level as the daily observed number of cases per age group minus the expected number of cases in the absence of heat waves. The standard 95% confidence interval (CI) of the model provided an estimation of the uncertainties surrounding the estimates. We also tested three alternative models as a robustness check, without significant differences in assessments (data available upon request). Two departments were excluded from the analysis due to data quality issues, and in some departments, analyses by age groups were limited by the very small number of cases.
Mortality
The heat wave periods were extended by three days to account for possible delayed effects [17]. We used yearly estimates of the all-cause excess mortality by age groups during heat waves (https://geodes.santepubliquefrance.fr) [18]. These estimates are based on the daily number of all-cause deaths (for age groups 0–14, 15–44, 45–64, 65–74, 75 and older) provided by the National Institute of Statistics and Economic Studies (INSEE) for a sample of 3,000 municipalities accounting for 80% of deaths in France, and extrapolated to provide estimates for the whole country. Excess mortality during heat waves is computed at the department level as observed mortality minus expected mortality, based on records from previous years, in the absence of heat waves.
For each period studied, the method provides five estimates corresponding to the number of preceding years (from one to five) considered, and summarized using the mean, minimum, and maximum values. We thereby obtained a range of possible values, although not equivalent to a 95% CI. Results are expressed in numbers of excess deaths per age group. We also derived an estimation of the associated years of life lost (YLL) computed as the number of excess deaths in each age group multiplied by the average remaining life expectancy by age group and sex (see supplementary Fig. 1 and supplementary Table 1 for details).
Loss of well-being
We approached loss of well-being through activity restriction associated with the red heat wave level (cancellation of various events, warnings to avoid travel and to reduce all physical activities). From a medical perspective, the temperatures during “red” days are likely to lead to symptoms such as fatigue, cramps, faintness, decreased alertness and cognitive function, even in young and healthy people. We considered the situation analogous to a Minor Restricted Activity Day (MRAD), i.e., “when individuals reduce most usual daily activities and replace them with less-strenuous activities or rest, but do not miss work or school” [19]. We defined the population exposed to MRAD as those residing in the departments throughout the red alert days. Data on tourists’ visits by day and department were not available.
Monetary estimates: central values
The overall health burden of heat waves was considered from a societal perspective and expressed through monetary estimates of effects from morbidity, mortality, and loss of well-being in euros 2017, which is the middle of the study period, based on the French national consumer price index.
Morbidity
Morbidity costs were estimated using a “cost-of-illness” (COI) approach that included direct medical costs (ED visits, outpatient clinic visits and hospitalizations), indirect costs (loss of production), and intangible components. We used the French generic cost of an ED visit without hospitalization: €151 [20]. The cost of an outpatient clinic visit was assessed based on the French national health insurance system fees, which depend on the times of day/night and days of the visit. We calculated an average visit cost weighted by the distributions of times and days of consultation during heat waves. We assumed that the hourly distribution of outpatient clinic visits attributable to the heat wave was similar to the hourly distribution of the total visits. We obtained an average cost of €48 per outpatient clinic consultation. We added a €5 additional fee for pediatric consultations (0–6 years) to cover the observed pediatric fraction (33%) of the excess visits during heat waves. Some ED and outpatient clinic visits were followed by hospitalization, but no details of the causes were available. We, therefore, arbitrarily selected the cost of hospitalization for respiratory disease (heat being a known risk factor for respiratory hospitalization [21, 22]). We chose a value of €3866, the total cost of an average hospital stay for a respiratory system condition in France [23].
Production losses were calculated using the average French gross daily salary of €104.24 [24] for the 71.5% of patients aged 15 to 64 in employment [25]. This calculation was also applied to children under 15, assuming that one parent would have to take leave from work to take care of his/her child, so that production losses were assessed for 71.5% of the patients aged 0–65 years. We assumed that one working day was lost for each ED and outpatient clinic visit not followed by hospitalization. For patients who were hospitalized, we considered a number of lost working days equal to twice the average length of hospitalization, to account for the home rest period [26, 27]. We used an average length of hospitalization of 6.7 days (average length of respiratory hospitalizations in France in 2017 [28]), i.e., loss of production for 13.4 days.
To account for the intangible components related to morbidity, we used Willingness-To-Pay (WTP) for reducing the risk of emergency room visits and hospitalization. Since the literature offered no heat-wave-specific WTP, we felt that the most appropriate substitute would be WTP estimated in the air pollution context [21, 22, 29]. We chose a WTP to avoid an ED visit of €267 from Ready et al. [27] and a WTP to avoid hospitalization of €1454, the arithmetic mean of the WTP values of €469 from Ready et al. [27] and €2440 from Chilton et al. [30].
Economists have not yet reached a clear consensus on the best way to jointly account for direct, indirect, and intangible components. Both the market price and the stated preference methods underestimate the actual total health burden, but combining the two methods could lead to a possible overlap (part of administration and medical care costs and economic production losses). We followed various studies [31–33] by grouping them together. Should a separate assessment be preferred, it can easily be obtained from the reported figures: the intangible component / market component ratio is 54/46 for the overall ED visit assessment, and about 23/77 for the overall hospitalization cost.
Mortality
We faced two main difficulties in valuing mortality effects, an essential but delicate exercise. First, no monetary expression of mortality meets with consensus among economists. Although it is common to use Value of a Statistical Life (VSL) and Value of a Life Year (VoLY), the choices are continually evolving with methodological developments [34]. Second, to our knowledge, there is no heat-wave-specific VSL or VoLY. To address the first challenge, we limit the arbitrariness of a choice between valuing excess deaths via VSL or via YLL with VoLY using both, as derived from stated preference methods. In the absence of heat-wave-specific data, we rely on values from the air pollution context, when available. For the VSL, we chose €3.17 million, as recommended for French public policies [35]. This is based on a study from the Organization for Economic Co-operation and Development that proposes a meta-analytical VSL from 856 valuations to be used in the evaluation of environmental, transport, and health policies [36]. For the VoLY, we chose €82,000, the arithmetic mean of the VoLY of €42,000 recommended by Desaigues et al. [37] for air pollution policies in the European Union and the €122,000 recommended by Quinet [35] in France.
In addition, as recently recommended by Hammitt et al. [34], we assessed the mortality impact for each year as an annual risk shared by the population living in departments experiencing heat waves, and expressed it in monetary terms per year and exposed inhabitant:
Loss of well-being
We used a stated preference approach to assess the WTP to avoid a MRAD during red-alert periods. In the absence of heat-wave-specific WTP, we selected the central value proposed by Ready et al. [27] of €43 for a MRAD.
Accounting for uncertainties
Both the estimates of health impacts and the choice of economic values involved uncertainty.
The health impacts were computed as the difference between the observed number of cases during each heat wave, and a theoretical expected number of cases for the same period of the year in the absence of heat waves. For morbidity, the uncertainty surrounding the modeling of the expected numbers was expressed as a 95% CI, whereas for mortality, it was approached by considering several reference years, providing a range of possible estimates. An additional uncertainty regarding mortality arose from the need to extrapolate from the results obtained on a sample of municipalities to the whole population. However, because the difference between the 2015 estimates obtained from the extrapolation and from the exhaustive mortality database was as low as 0.2% [9], extrapolation-related uncertainty can be considered negligible.
We also tried to capture the uncertainties associated with the economic values. When the figures are derived from stated preference methods (VSL, VoLY, MRAD, intangible component of morbidity), uncertainties come from the inherent variability of individual subjective WTP. When using figures derived from medical costs, we tried to take into account the cost ranges whenever possible. A major source of uncertainty lies in our decision to use costs of hospitalizations for respiratory causes. Indeed, our database informed us on the primary reason for an ED visit, but not on the units where people were hospitalized afterwards. This would influence the costs of hospitalization, as would patient age, severity of diagnosis or average length of stay. Merrill et al. found, for example, that a cold-related hospitalization stay is twice as expensive as a heat-related stay in the U.S., mainly due to the doubling of length of stay [38]. More detailed information on the characteristics of hospitalizations for heat-related causes would help reduce the uncertainties surrounding future economic estimates. Finally, for indirect costs (loss of production), the uncertainty comes from the impossibility of attributing a specific income according to the patient’s professional status, as detailed information on occupation was not available.
We accounted for uncertainty using a (standard) independent as well as an integrated approach.
The first approach considered the uncertainties for health outcomes separately from the uncertainties for economic values. For morbidity, the uncertainty comes from the 95% CI around the central estimate; for mortality, it comes from the minimum and maximum values. No health uncertainty is associated with loss of well-being, which is based on observed numbers of red days and population exposed. For the estimates of the unit economic values, we applied a ± 33% range around the economic estimate as a rule of thumb previously recommended [39], to mimic a one-standard-deviation change around the mean for a Normal distribution. Researchers sometimes choose the minimum and maximum unit economic values, like Limaye et al. [40], who obtain a range of USD 1–24.4 million for the VSL. We felt this would introduce too much variability relative to the uncertainty from health outcomes, especially when jointly considering the two sources of uncertainty. For production losses, this range corresponds roughly to decile 3—decile 8 of the gross salary distribution [24]. We obtained a range of monetary valuations (low, central, and high) for each health outcome and each year, providing a range of magnitude for the monetary health benefits associated with heat waves.
The second approach combined the uncertainties related to the health impact estimates and the economic values through an integrated approach based on Monte Carlo simulations [39, 41]. For morbidity, values were sampled from a Normal approximation of the quasi-Poisson distribution whose central value is the central estimate of the models, and the standard deviation is derived from the 95% CI. For mortality, values were equiprobably sampled from 4 estimates considering 2 to 5 years. Expected mortality was not assessed on a 1-year basis due to the large number of missing data (as heat waves are increasingly frequent, it was often impossible to assess mortality in the absence of heat waves based on only 1 year’s data). Epidemiological uncertainty associated with loss of well-being was not assessed, as explained above. For each unit economic value, we used a triangular distribution defined in terms of a central value, a maximum and a minimum (here based on the ± 33% range around the central value), standard practice when knowledge of the variable is more subjective than objective. Once defined, we generated 10,000 Monte Carlo samples from these probability distributions, which provided a probabilized distribution of the economic assessment of the heat-wave-related morbidity and mortality impacts each year.
Results
Table 1 summarizes the economic impacts, detailed below. Losses of well-being were only observed in 2019 following the triggering of the red alert, and represent €2.3 billion that year. Mortality effects account for the largest share, but the valuation differs depending on the metric used. Valuations based on VSL are around two to three times higher than those based on VoLY, partly because almost two-thirds of deaths occurred after the age of 75 and thus with low loss of life expectancy. Morbidity accounts for a very small share (around 0.1%) of the total. Overall, the largest impacts were observed in 2019 (partly due to the loss of well-being) and the smallest in 2016 and 2017.
Table 1.
Summary of health-related economic impacts from 2015 to 2019 heat waves in France
| Year | Morbidity (in million €2017) | Mortality (in billion €2017) based on | Loss of well-being (in billion €2017) | Total (in billion €2017) based on | ||
|---|---|---|---|---|---|---|
| Excess deaths | YLL | Excess deaths | YLL | |||
| 2015 | 6.97 [4.96–9.25] | 5.71 [4.19–7.34] | 1.65 [1.21–2.12] | 0 | 5.72 [4.20–7.35] | 1.66 [1.22–2.13] |
| 2016 | 1.38 [0.98–1.84] | 1.65 [1.23–2.08] | 0.60 [0.44–0.75] | 0 | 1.65 [1.23–2.08] | 0.60 [0.45–0.75] |
| 2017 | 4.24 [3.02–5.65] | 3.33 [2.37–4.39] | 1.34 [1.00–1.69] | 0 | 3.34 [2.38–4.39] | 1.35 [1.00–1.70] |
| 2018 | 7.14 [5.00–9.66] | 5.94 [3.62–8.06] | 2.22 [1.35–3.00] | 0 | 5.95 [3.63–8.06] | 2.22 [1.36–3.01] |
| 2019 | 10.90 [7.54–14.76] | 6.31 [3.51–8.80] | 2.47 [1.59–3.30] | 2.32 [1.72–2.92] | 8.64 [5.72–11.29] | 4.80 [3.71–5.86] |
Figures were obtained from the integrated uncertainty approach, intervals in brackets are based on the Percentile 2.5 (P2.5) and P97.5 of the underlying Monte Carlo distributions
Economic estimate of the impact of heat waves on morbidity
Between 2015 and 2019, 8990 [6883–11,209] excess ED visits and 3363 [2708–4024] excess outpatient clinic visits not followed by hospitalization were observed during heat waves. 4654 [3320–6105] visits were followed by hospitalization (Table 2). The figure for ED visits not followed by hospitalization is €4.290 million [3.277–5.355], and for ED visits followed by hospitalization €24.495 million [17.458–32.299]. There were €0.361 million [0.287–0.435] outpatient clinic visits not followed by hospitalization and €1.506 million [0.882–2.181] visits followed by hospitalization (see Table 2, and supplementary Tables 2 and 3 for details). ED visits followed by hospitalization represented 80% of the morbidity costs, and ED visits not followed by hospitalization 14%. The largest health impacts and the highest costs were observed in 2019, representing 36% of the total morbidity costs observed over the period. 2019 was indeed characterized by very high diurnal temperatures (up to 46 °C) compared to the other years, while nocturnal temperatures remained conducive to body heat dissipation. Thus, the population’s acute diurnal exposure led to a high number of ED visits, especially from the youngest due to their intense daytime physical activities, but these visits were not necessarily followed by hospitalization.
Table 2.
Morbidity impacts and associated costs during heat waves in France 2015–2019
| Health outcomes | Year | Cases | Economic evaluation (in thousand €2017) | ||||
|---|---|---|---|---|---|---|---|
| Total number of visits for selected causes | Expected number of visits in the absence of heat wave [95% CI] | Excess number of visits attributed to heat wave [95% CI] | Low 95% CI | Central 95% CI | High 95% CI | ||
| ED visits not followed by hospitalization | 2015 | 7825 | 5941 [5488–6387] | 1884 [1450–2337] | 606 [466–751] | 904 [696–1121] | 1202 [925–1490] |
| 2016 | 1770 | 1515 [1416–1616] | 274 [196–360] | 89 [64–117] | 133 [95–174] | 176 [126–232] | |
| 2017 | 7001 | 5549 [5182–5912] | 1474 [1147–1826] | 477 [371–590] | 711 [553–881] | 946 [736–1172] | |
| 2018 | 9831 | 8134 [7613–8648] | 1729 [1256–2229] | 550 [398–710] | 821 [594–1060] | 1091 [790–1410] | |
| 2019 | 14,279 | 10,654 [9822–11,483] | 3629 [2834–4457] | 1154 [898–1420] | 1722 [1340–2119] | 2290 [1782–2818] | |
| Outpatient clinic visits not followed by hospitalization | 2015 | 1780 | 1001 [851–1150] | 779 [630–929] | 56 [44–67] | 82 [65–99] | 109 [87–131] |
| 2016 | 342 | 232 [204–262] | 121 [98–146] | 8 [6–10] | 12 [10–15] | 16 [13–20] | |
| 2017 | 1473 | 898 [786–1010] | 585 [482–689] | 45 [36–52] | 66 [54–78] | 87 [71–103] | |
| 2018 | 1890 | 1180 [1041–1319] | 711 [574–849] | 51 [41–61] | 75 [60–91] | 100 [80–120] | |
| 2019 | 2953 | 1786 [1542–2030] | 1167 [924–1411] | 85 [66–104] | 125 [97–153] | 166 [129–203] | |
| ED visits followed by hospitalization | 2015 | 4340 | 3372 [3061–3680] | 1005 [744–1286] | 3757 [2750–4858] | 5607 [4104–7251] | 7458 [5458–9644] |
| 2016 | 955 | 768 [703–833] | 211 [161–263] | 786 [596–986] | 1173 [889–1472] | 1561 [1183–1958] | |
| 2017 | 3304 | 2821 [2594–3048] | 569 [407–757] | 2145 [1515–2882] | 3202 [2261–4300] | 4259 [3007–5720] | |
| 2018 | 5218 | 4209 [3874–4545] | 1072 [781–1379] | 3985 [2873–5186] | 5948 [4288–7741] | 7911 [5703–10,295] | |
| 2019 | 6891 | 5407 [4871–5941] | 1534 [1071–2044] | 5738 [3963–7728] | 8564 [5915–11,534] | 11,391 [7868–15,341] | |
| Outpatient clinic visits followed by hospitalization | 2015 | 151 | 89 [54–128] | 67 [33–97] | 254 [122–376] | 380 [182–560] | 505 [242–746] |
| 2016 | 24 | 16 [8–21] | 11 [10–16] | 42 [37–60] | 62 [55–90] | 83 [73–120] | |
| 2017 | 104 | 64 [43–86] | 47 [27–63] | 183 [105–249] | 272 [156–371] | 362 [207–494] | |
| 2018 | 142 | 93 [60–119] | 56 [37–83] | 213 [139–319] | 318 [208–477] | 423 [276–634] | |
| 2019 | 184 | 110 [69–155] | 82 [49–117] | 318 [188–457] | 474 [281–682] | 631 [374–907] | |
All intervals in brackets are standard 95% confidence interval (CI) of the underlying epidemiological models. Excess numbers attributed to heat wave is not exactly equal to total numbers minus expected numbers due to negative number of excess cases
Economic estimate of the impact of heat waves on mortality
Between 2015 and 2019, 7309 [5018–10,105] excess deaths were observed during heat waves, representing 102,108 YLL [67,005–147,931] (Table 3). In absolute numbers, the largest impacts were observed in 2015, 2018, and 2019, and when expressed in an excess death rate per 100, 000 exposed inhabitants, in 2015 (5.37 [4.21–6.54]) and 2018 (4.09 [2.92–5.51]). Mortality by age group is detailed in Supplementary Table 4. Estimates for children are to be interpreted with caution due to the small number of cases. The total economic valuation of excess mortality was estimated at €23 billion using the VSL approach and €8.3 billion using the VoLY approach. Under the VSL approach, the estimated economic impact of mortality during heat waves ranged from €68 per capita in 2017 to €170 per capita in 2015.
Table 3.
Economic evaluation of excess mortality during 2015–2019 heat waves in France
| Year | Exposed population to heat waves | Health impacts | Economic evaluation of excess deaths (in billion €2017) | Economic evaluation per exposed inhabitant (in €2017) | Economic evaluation of YLL (in billion €2017) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of excess deaths [min–max] | Excess death rate (per 100 000 exposed inhabitants) | Number of YLL [min–max] | Low [min–max] | Central [min–max] | High [min–max] | Low [min–max] | Central [min–max] | High [min–max] | Low [min–max] | Central [min–max] | High [min–max] | ||
| 2015 | 33,181,782 | 1782 [1396–2169] | 5.37 [4.21–6.54] | 19,844 [14,443–25,628] | 3.8 [3.0–4.6] | 5.6 [4.4–6.9] | 7.5 [5.9–9.1] | 114 [89–139] | 170 [133–207] | 226 [177–276] | 1.1 [0.8–1.4] | 1.6 [1.2–2.1] | 2.2 [1.6–2.8] |
| 2016 | 20,511,564 | 516 [376–677] | 2.52 [1.83–3.30] | 7261 [5020–10,036] | 1.1 [0.80–1.4] | 1.6 [1.2–2.1] | 2.2 [1.6–2.9] | 53 [39–70] | 80 [58–105] | 106 [77–139] | 0.4 [0.3–0.6] | 0.6 [0.4–0.8] | 0.8 [0.55–1.1] |
| 2017 | 46,306,151 | 991 [596–1532] | 2.14 [1.29–3.31] | 15,679 [9705–24,720] | 2.1 [1.3–3.3] | 3.1 [1.9–4.9] | 4.2 [2.5–6.5] | 45 [27–70] | 68 [41–105] | 90 [54–139] | 0.9 [0.5–1.4] | 1.3 [0.8–2.0] | 1.7 [1.1–2.7] |
| 2018 | 48,547,206 | 1988 [1416–2674] | 4.09 [2.92–5.51] | 28,547 [19,093–40,367] | 4.2 [3.0–5.7] | 6.3 [4.5–8.5] | 8.4 [6.0–11.3] | 87 [62–117] | 130 [92–175] | 173 [123–232] | 1.6 [1.0–2.2] | 2.3 [1.6–3.3] | 3.1 [2.1–4.4] |
| 2019 | 60,375,314 | 2032 [1234–3053] | 3.37 [2.04–5.06] | 30,777 [18,744–47,181] | 4.3 [2.6–6.5] | 6.4 [3.9–9.7] | 8.6 [5.2–12.9] | 71 [43–107] | 107 [65–160] | 142 [86–213] | 1.7 [1.0–2.6] | 2.5 [1.5–3.9] | 3.4 [2.0–5.1] |
All intervals in brackets are the minimum and maximum estimates of the underlying models used to estimate excess deaths and YLL
Economic estimate of the impact of heat waves on well-being
The red alert was only observed for two days in 2019, affecting almost 27 million French citizens and economically estimated at €2.3 billion [1.5–3.1].
Accounting for uncertainties
Uncertainties of an epidemiological nature are shown as 95% CI for morbidity (Table 2) and as min–max values for mortality (Table 3). Uncertainties of an economic nature are shown as low and high estimates (Tables 2, 3), and associated with the range of health outcomes to provide a separate treatment of uncertainties.
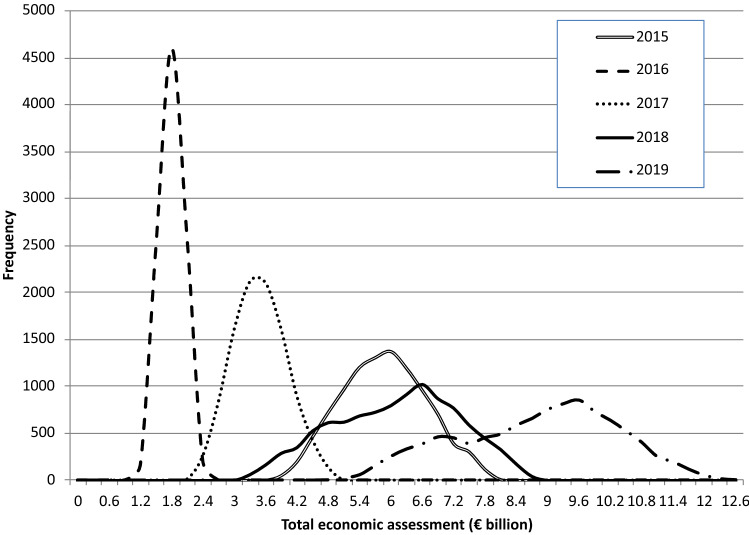
Figure 1 represents a more thorough treatment of uncertainty, considered jointly thanks to Monte Carlo simulations. For each year, the probabilized distribution of the total economic assessment is plotted based on combined morbidity, mortality (measured by excess deaths), and well-being impacts, although mortality effects obviously dominate. Years 2015, 2018, and 2019 have the highest total (health) impacts, the latter mainly because it is the only year where heat reached red-alert levels, for which loss of well-being due to MRAD is assessed.
Fig. 1.
Monte Carlo simulated probability distribution of total economic assessment by year (€ billion)
Discussion
Between 2015 and 2019, we estimate that the selected health impacts of heat waves amount to €25.5 billion, the majority through mortality (€23.2 billion) and the remainder through minor restricted activity days (€2.3 billion) and morbidity (€0.031 billion). These results highlight a significant economic burden on the French health system and society. Most of these impacts come from premature mortality, which simply means earlier medical and funeral costs associated with a death, but whose intangible component represents a societal burden often under-estimated and invisible. Also important are intangible effects due to the loss of well-being (MRAD), which raises questions about the social acceptability of using restrictions to prevent the impacts of heat waves [13]. Morbidity hence represents a tiny fraction of the economic burden, which suggests that the health system is only slightly impacted.
However, there are several additional factors to consider. First, these heat-related health impacts occur over a very short time span, which can lead to health system congestion with potential costly indirect consequences. Second, only certain health impacts were explored here, not all possible adverse outcomes. A growing literature links heat with a wide range of adverse health outcomes (cardiorespiratory effects [42], mental health [43], pregnancy outcome [44], occupational health, and productivity loss [45, 46]). In particular, the loss of productivity and of working time directly affects the private sector: Vanos et al. [47] show for Canadian outdoor industrial workers that the loss may be about 1% of the annual number of hours worked, Orlov et al. [48] estimate the hourly mean costs for agricultural and construction workers in 10 European countries at about $4.4 in July 2015, and Zhang et al. [49] estimate US labor losses due to temperature differences between 2006–2016 and 1980–1990 at about $1.7 billion per year. However, lack of epidemiological data prevented us from including more health outcomes. Finally, our focus on heat waves certainly underestimates the total burden of heat-related health impacts: high temperatures, even when not classified as heat waves, impact health too, not only directly but also indirectly through an increase in ozone pollution, allergenic risks, and vector-borne diseases.
Monte Carlo simulations offer a way to combine uncertainties associated with methodological choices in epidemiological modeling and economic evaluation. When the simulated mean and 95% CI are compared with the economic evaluations (in Tables 2, 3, central, min, and max values), the absolute average difference (over the 5 years) for the central value is 3.03% using the VSL approach and 2.44% using the VoLY approach. The average 95% CI interval ranges are smaller for the Monte Carlo simulations, by about 24% in the VoLY approach and 5% in the VSL approach. Overall, jointly accounting for uncertainty provides a better (and narrower) representation of the distribution of the economic impacts.
The values we found may appear low in comparison to other public health issues. For example, Chanel et al. [50] estimated the economic impact of avoiding 48,283 premature deaths from chronic exposure to fine particles (PM2.5) at €145 billion for France. Heat waves are rare events happening on a few days per year—therefore with a much smaller impact—but the expected rise in temperatures and in the number of heat waves should sharply increase the associated economic burden.
The World Meteorological Organization reported that almost all attribution studies investigating major heat waves since 2015 found that their probability was significantly increased by anthropogenic climate change [51]. For instance, the heat wave of July 2019 was actually determined to be almost impossible in the absence of climate change (less than once every 1000 years) [52]. In France, daily departmental warnings rose from 607 between 2010 and 2014, to 2252 between 2015 and 2019 [13]. It is noteworthy that summer 2020 also saw exceptional heat waves, resulting in the highest mortality burden observed since the implementation of the French heat action plan [13]. Therefore, our economic evaluation adds further evidence of the overall economic burden associated with climate change and underlines the urgent need for concrete adaptation actions.
Our study is subject to inherent uncertainties linked to the choice and modeling of health impacts, as well as to the economic values we used, often derived from air pollution studies in the absence of heat-wave-specific values. First, we assumed the entire excess deaths and health care utilization calculated to be attributable to the heat waves. An alternative would have been to model the fraction of mortality and morbidity attributable to each heat wave, but such models also involve high uncertainty, given the rarity of heat waves, the strong non-linearity of the temperature-mortality relationship, and its sensitivity to contextual factors (e.g., adverse effect prevention campaigns, summer months when heat waves occur). Models were previously shown to be unable to capture all heat wave mortality impacts, especially during the most extreme events [18, 53]. The capacity to model morbidity has seldom been studied in the literature.
The mortality estimates we used were extrapolated from a sample of municipalities, as it takes approximately 5 years to obtain a complete mortality database in France. Comparison of observed and extrapolated data for the 2015 heat wave showed that this extrapolation provided a reliable order of magnitude of total mortality impact in France (data not shown). Our morbidity data came from an almost exhaustive sample of hospitals. Extrapolating these to the whole country yields €30.8 million in excess ED visits and €1.96 million in excess outpatient clinic visits for 2015–19.
Second, regarding economic values, we implicitly assumed that life expectancy at death for excess heat-wave-related deaths was similar to that observed for all causes of death, in the absence of relevant data. Clearly, a different life expectancy value would change the share of mortality in the total economic assessment, especially in the extreme case of only one YLL per death [54, 55]. Less importantly, losses of production were only included for the 0–64 age group, although the French employed population aged 65–69 was estimated at 7.8% in 2019 [36].
In the literature, we found about 20 studies investigating the economic impacts of adverse health outcomes due to heat waves, 12 at single-country level and 7 for the European Union (see [7] for a recent review of 10 of them). They varied widely in their approach to heat wave definition, type of health indicators used, computation of excess cases, thus limiting comparability. Most of the studies only included direct impacts in the economic valuation: mortality [40, 54, 56–68], hospital admissions or outpatient visits (emergency room visits, hospitalizations, outpatient consultations, etc.) [38, 40, 54, 56–58, 62–64, 67, 69–72] or the loss of production associated with morbidity [40, 56, 58, 63, 66, 71]. Fourteen studies built a model to obtain the number of hospital admissions or outpatient visits associated with heat waves [40, 54, 56–64, 69, 71, 72], while the others did not specify their method of calculation. All the studies found the estimated health costs of heat waves to be significant.
These studies, together with our wider perspective that includes intangible effects, argue for stronger actions to prevent adverse health consequences of heat waves. Such actions are essential for several reasons. First, heat-related health effects are generally preventable. Unlike other natural hazards—like volcanoes, landslides, tsunamis or earthquakes—or other extreme weather events—like hurricanes, floods or wildfires—heat waves can be anticipated, and preventive behaviors are relatively simple to implement.
Second, heat-related health impacts may increase because of climate change. The already-observed increased frequency, duration, and intensity of heat waves [73] makes adaptation desirable. In addition, the period when heat waves occur is also extending; while events were historically observed in July and August, they are now also recorded earlier, in June, and later, in September.
Third, the most vulnerable in the population—the poorest, the elderly, people socially isolated or suffering from chronic diseases—are more severely affected than the rest of the population, and it is the responsibility of public decision-makers to protect them. Inequities in heat-exposure [74] can be combined with higher individual susceptibility to heat [4, 70] and with limited access to protective behaviors [5]. The increase in vulnerability due to aging, health inequities or socio-economic disadvantage associated with the COVID-19 outbreak is likely to worsen the health consequences of heat waves [75].
Fourth, most actions aimed at preventing heat-related health consequences are likely to be cost-effective, especially low-cost action such as heat-health action plans and warning systems or behavioral changes at the individual and community level. Heat-health early warning systems are generally found to be cost-effective [76]. In Philadelphia, 117 lives are estimated to have been saved in 3 years [77], with an annual benefit in terms of reduction in mortality estimated at €157 million per year, and an operating cost of €154,000 per year after an initial development cost of €80,000 [78]. In France, the preparation and development cost of the national heat-wave and health alert system initiated in 2005 was €287,000 and it involves an annual operating cost of €454,000 [79]. Its health benefits were not evaluated in terms of mortality. However, 75% of the French population reported adopting at least one heat-related protective behavior during heat waves [80]. Education and communication can trigger positive behavioral changes at the individual level, like resting in cool places for a few hours, avoiding extreme heat exposure for outdoor workers or enhancing medical staff efficiency in treating heat-related diseases [4, 11]. Actions on housing or on the urban heat island are more costly, but they can take a broader approach aimed at promoting a healthier lifestyle and increasing resilience, while mitigating climate change. From a decision process perspective, there is a need for novel approaches that manage a wide range of climate- and non-climate-related risks by focusing on receptor systems instead of conventional means, and monetizing wider/cross-sectoral impacts [81]. Overall, allocating more resources in the short term would reduce longer-term health spending.
Supporting the implementation of these adaptation actions and alerting decision-makers to the urgency of the situation will require a better understanding of the economic impacts of climate change’s effects on health. Further research on the health impacts of heat waves is needed, together with their economic evaluation, to better understand the non-linear effect of extreme temperatures and events with no historical precedent. Efforts should be made to obtain robust fractions attributable to mortality and morbidity, to assess the risk of onset or exacerbation of chronic heat-related diseases during heat waves and to estimate heat-wave-specific monetary values. Attempts to predict the magnitude of future heat waves would also be welcome.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank Guillaume Boulanger and two anonymous reviewers for helpful comments and suggestions, and Marjorie Sweetko for her thorough re-reading of the English.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by LA and OC. The first draft of the manuscript was written by LA and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the French National Research Agency Grants ANR-17-EURE-0020 and ANR-16-CE03-0005 (GREEN-Econ), and by the Excellence Initiative of Aix-Marseille University—A*MIDEX.
Data availability
Data are available upon request to the authors.
Code availability
Code are available upon request to the authors.
Declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Core Writing Team, Pachauri, R.K., Meyer, L.A.: Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. IPCC, Geneva, Switzerland (2014)
- 2.Kousky C. Informing climate adaptation: A review of the economic costs of natural disasters. Energy Econ. 2014;46:576–592. doi: 10.1016/j.eneco.2013.09.029. [DOI] [Google Scholar]
- 3.WMO: WMO Statement on the State of the Global Climate in 2019. World Meteorological Organization (WMO), Geneva, Switzerland (2020)
- 4.Limaye VS, Max W, Constible J, Knowlton K. Estimating the costs of inaction and the economic benefits of addressing the health harms of climate change. Health Aff. (Millwood) 2020;39:2098–2104. doi: 10.1377/hlthaff.2020.01109. [DOI] [PubMed] [Google Scholar]
- 5.Bone A, O’Connell E. Health and high temperatures. Public Health. 2018;161:117–118. doi: 10.1016/j.puhe.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Schmitt LHM, Graham HM, White PCL. Economic evaluations of the health impacts of weather-related extreme events: A scoping review. Int. J. Environ. Res. Public. Health. 2016;13:1105. doi: 10.3390/ijerph13111105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wondmagegn BY, Xiang J, Williams S, Pisaniello D, Bi P. What do we know about the healthcare costs of extreme heat exposure? A comprehensive literature review. Sci. Total Environ. 2019;657:608–618. doi: 10.1016/j.scitotenv.2018.11.479. [DOI] [PubMed] [Google Scholar]
- 8.Robine J-M, Cheung SLK, Le Roy S, Van Oyen H, Griffiths C, Michel J-P, Herrmann FR. Death toll exceeded 70,000 in Europe during the summer of 2003. C. R. Biol. 2008;331:171–178. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Ung A, Corso M, Pascal M, Laaidi K, Wagner V, Beaudeau P, Le Tertre A. Évaluation de la surmortalité pendant les canicules des étés 2006 et 2015 en France métropolitaine. Saint-Maurice, France: Santé publique France; 2019. [Google Scholar]
- 10.DGS: Impacts du changement climatique sur la santé en France : Eléments de coûts. Direction Générale de la Santé (DGS) (2009)
- 11.Sheehan MC, Fox MA, Kaye C, Resnick B. Integrating health into local climate response: lessons from the U.S. CDC climate-ready states and cities initiative. Environ. Health Perspect. 2017;125:094501. doi: 10.1289/EHP1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ministère des Solidarités et de la Santé: Le Plan national canicule, https://solidarites-sante.gouv.fr/sante-et-environnement/risques-climatiques/article/le-plan-national-canicule
- 13.Pascal M, Lagarrigue R, Tabai A, Bonmarin I, Camail S, Laaidi K, Le Tertre A, Denys S. Evolving heat waves characteristics challenge heat warning systems and prevention plans. Int. J. Biometeorol. 2021 doi: 10.1007/s00484-021-02123-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pascal M, Laaidi K, Ledrans M, Baffert E, Caserio-Schönemann C, Le Tertre A, Manach J, Medina S, Rudant J, Empereur-Bissonnet P. France’s heat health watch warning system. Int. J. Biometeorol. 2006;50:144–153. doi: 10.1007/s00484-005-0003-x. [DOI] [PubMed] [Google Scholar]
- 15.Atiki N, Pascal M, Wagner V. Influence de la chaleur sur quelques causes de recours aux soins d’urgences en France métropolitaine durant les étés 2015–2017. Bull Epidémiol Hebd. 2018;1:9–14. [Google Scholar]
- 16.Kovats RS, Kristie LE. Heatwaves and public health in Europe. Eur. J. Public Health. 2006;16:592–599. doi: 10.1093/eurpub/ckl049. [DOI] [PubMed] [Google Scholar]
- 17.Pascal M, Wagner V, Corso M, Laaidi K, Ung A, Beaudeau P. Heat and cold related-mortality in 18 French cities. Environ. Int. 2018;121:189–198. doi: 10.1016/j.envint.2018.08.049. [DOI] [PubMed] [Google Scholar]
- 18.Antics A, Pascal M, Laaidi K, Wagner V, Corso M, Declercq C, Beaudeau P. A simple indicator to rapidly assess the short-term impact of heat waves on mortality within the French heat warning system. Int. J. Biometeorol. 2013;57:75–81. doi: 10.1007/s00484-012-0535-9. [DOI] [PubMed] [Google Scholar]
- 19.EPA: Final Ozone NAAQS Regulatory Impact Analysis. U.S. Environmental Protection Agency, North Carolina, US (2008)
- 20.Ccomptes: Les urgences hospitalières : des services toujours trop sollicités. Cour des comptes (2019)
- 21.Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y, Tian J, Shang K. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Sci. Total Environ. 2017;586:241–254. doi: 10.1016/j.scitotenv.2017.01.212. [DOI] [PubMed] [Google Scholar]
- 22.Martínez-Solanas È, Basagaña X. Temporal changes in the effects of ambient temperatures on hospital admissions in Spain. PLoS ONE. 2019;14:e0218262. doi: 10.1371/journal.pone.0218262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rafenberg, C.: Estimations des coûts pour le système de soins français de cinq maladies respiratoires et des hospitalisations attribuables à la pollution de l’air. Commissariat Général au Développement Durable (CGDD), La Défense, France (2015)
- 24.Insee: Salaires dans les entreprises 2018., https://www.insee.fr/fr/statistiques/3303417?sommaire=3353488.
- 25.Insee: Population active 2018., https://www.insee.fr/fr/statistiques/3303384?sommaire=3353488.
- 26.Chanel, O.: Guidelines on monetary cost calculations related to air-pollution health impacts. (2011)
- 27.Ready R, Navrud S, Day B, Dubourg R, Machado F, Mourato S, Spanninks F, Rodriquez MXV. Benefit transfer in Europe: How reliable are transfers between countries? Environ. Resour. Econ. 2004;29:67–82. doi: 10.1023/B:EARE.0000035441.37039.8a. [DOI] [Google Scholar]
- 28.OECD: OECD Health Data 2019
- 29.Chiabai A, Spadaro JV, Neumann MB. Valuing deaths or years of life lost? Economic benefits of avoided mortality from early heat warning systems. Mitig. Adapt. Strateg. Glob. Change. 2018;23:1159–1176. doi: 10.1007/s11027-017-9778-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chilton, S., Covey, J., Jones-Lee, M., Loomes, G., Metcalf, H.: Valuation of Health Benefits Associated with Reductions in Air Pollution. Department for Environment, Food and Rural Affairs (Defra), London, UK (2004)
- 31.Defra: An Economic Analysis to inform the Air Quality Strategy. Updated Third Report of the Interdepartmental Group on Costs and Benefits. Department of Environment, Food and Rural Affairs (Defra), London, UK (2007)
- 32.de Ayala, A., Spadaro, J.V.: Economic costs of health effects PURGE project (2014)
- 33.Ortiz RA, Hunt A, da Motta RS, MacKnight V. Morbidity costs associated with ambient air pollution exposure in Sao Paulo. Brazil. Atmospheric Pollut. Res. 2011;2:520–529. doi: 10.5094/APR.2011.059. [DOI] [Google Scholar]
- 34.Hammitt JK, Morfeld P, Tuomisto JT, Erren TC. Premature deaths, statistical lives, and years of life lost: identification, quantification, and valuation of mortality risks. Risk Anal. 2020;40:674–695. doi: 10.1111/risa.13427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Quinet, E.: L’évaluation socioéconomique des investissements publics. Commissariat général à la stratégie et à la prospective (2013)
- 36.Lindhjem H, Navrud S, Braathen NA, Biausque V. Valuing mortality risk reductions from environmental, transport, and health policies: a global meta-analysis of stated preference studies. Risk Anal. 2011;31:1381–1407. doi: 10.1111/j.1539-6924.2011.01694.x. [DOI] [PubMed] [Google Scholar]
- 37.Desaigues B, Ami D, Bartczak A, Braun-Kohlová M, Chilton S, Czajkowski M, Farreras V, Hunt A, Hutchison M, Jeanrenaud C, Kaderjak P, Máca V, Markiewicz O, Markowska A, Metcalf H, Navrud S, Nielsen JS, Ortiz R, Pellegrini S, Rabl A, Riera R, Scasny M, Stoeckel M-E, Szántó R, Urban J. Economic valuation of air pollution mortality: A 9-country contingent valuation survey of value of a life year (VOLY) Ecol. Indic. 2011;11:902–910. doi: 10.1016/j.ecolind.2010.12.006. [DOI] [Google Scholar]
- 38.Merrill CT, Miller M, Steiner C. Hospital Stays Resulting from Excessive Heat and Cold Exposure Due to Weather Conditions in US Community Hospitals, 2005: Statistical Brief #55. In: Merrill CT, Miller M, Steiner C, editors. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville MD: Agency for Healthcare Research and Quality (US); 2008. [PubMed] [Google Scholar]
- 39.CAFE: Methodology for the Cost-Benefit Analysis for CAFE - Volume 3: Uncertainty in the CAFE. (2005)
- 40.Limaye VS, Max W, Constible J, Knowlton K. Estimating the health-related costs of 10 climate-sensitive U.S. events during 2012. GeoHealth. 2019;3:245–265. doi: 10.1029/2019GH000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chanel O, Henschel S, Goodman P, Analitis A, Atkinson R, Le Tertre A, Zeka A, Medina S. Economic valuation of the mortality benefits of a regulation on SO2 in 20 European cities. Eur. J. Public Health. 2014;24:631–637. doi: 10.1093/eurpub/cku018. [DOI] [PubMed] [Google Scholar]
- 42.Cheng J, Xu Z, Bambrick H, Prescott V, Wang N, Zhang Y, Su H, Tong S, Hu W. Cardiorespiratory effects of heatwaves: A systematic review and meta-analysis of global epidemiological evidence. Environ. Res. 2019;177:108610. doi: 10.1016/j.envres.2019.108610. [DOI] [PubMed] [Google Scholar]
- 43.Thompson R, Hornigold R, Page L, Waite T. Associations between high ambient temperatures and heat waves with mental health outcomes: a systematic review. Public Health. 2018;161:171–191. doi: 10.1016/j.puhe.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 44.Bekkar B, Pacheco S, Basu R, DeNicola N. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: A systematic review. JAMA Netw. Open. 2020;3:e208243–e208243. doi: 10.1001/jamanetworkopen.2020.8243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Flouris AD, Dinas PC, Ioannou LG, Nybo L, Havenith G, Kenny GP, Kjellstrom T. Workers’ health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet. Health. 2018;2:e521–e531. doi: 10.1016/S2542-5196(18)30237-7. [DOI] [PubMed] [Google Scholar]
- 46.Borg MA, Xiang J, Anikeeva O, Pisaniello D, Hansen A, Zander K, Dear K, Sim MR, Bi P. Occupational heat stress and economic burden: A review of global evidence. Environ. Res. 2021;195:110781. doi: 10.1016/j.envres.2021.110781. [DOI] [PubMed] [Google Scholar]
- 47.Vanos J, Vecellio DJ, Kjellstrom T. Workplace heat exposure, health protection, and economic impacts: A case study in Canada. Am. J. Ind. Med. 2019;62:1024–1037. doi: 10.1002/ajim.22966. [DOI] [PubMed] [Google Scholar]
- 48.Orlov A, Sillmann J, Aaheim A, Aunan K, de Bruin K. Economic losses of heat-induced reductions in outdoor worker productivity: A case study of Europe. Econ. Disasters Clim. Change. 2019;3:191–211. doi: 10.1007/s41885-019-00044-0. [DOI] [Google Scholar]
- 49.Zhang Y, Shindell DT. Costs from labor losses due to extreme heat in the USA attributable to climate change. Clim. Change. 2021;164:35. doi: 10.1007/s10584-021-03014-2. [DOI] [Google Scholar]
- 50.Chanel O, Medina S, Pascal M. Évaluation économique de la mortalité liée à la pollution atmosphérique en France. J. Gest. Economie Santé. 2020;2:77–92. doi: 10.3917/jges.202.0077. [DOI] [Google Scholar]
- 51.WMO: The Global Climate in 2015–2019. World Meteorological Organization (WMO), Geneva, Switzerland (2019)
- 52.Vautard R, Boucher O, Jan van Oldenborgh G, Otto F, Haustein K, Vogel M, Seneviratne S, Soubeyroux J-M, Schneider M, Drouin A, Ribes A, Kreienkamp F, Stott P, van Aalst M. Human contribution to the record-breaking July 2019 heat wave in Western Europe. Environ. Res. Lett. 2019;15:094077. doi: 10.1088/1748-9326/aba3d4. [DOI] [Google Scholar]
- 53.Le Tertre A, Lefranc A, Eilstein D, Declercq C, Medina S, Blanchard M, Chardon B, Fabre P, Filleul L, Jusot J-F, Pascal L, Prouvost H, Cassadou S, Ledrans M. Impact of the 2003 Heatwave on all-cause mortality in 9 French cities. Epidemiology. 2006;17:75–79. doi: 10.1097/01.ede.0000187650.36636.1f. [DOI] [PubMed] [Google Scholar]
- 54.Hunt, A., Boyd, R., Taylor, T., Kovats, S., Lachowyz, K., Watkiss, P., Horrocks, L.: Report on costs of the hot summer of 2003. Project E – Quantify the cost of impacts and adaptation, Climate Change Impacts and Adaptation: Cross-Regional Research Programme. Department of Environment, Food and Rural Affairs (Defra), UK (2007)
- 55.Kovats S, Lloyd S, Hunt A, Watkiss P. Technical Policy Briefing Note 5: The impacts and economic costs on health in Europe and the costs and benefits of adaptation. Results of the ECRTD Climate Cost Project. In: Watkiss P, editor. The Climate Cost Project Final Report. Sweden: Stockholm Environment Institute; 2011. [Google Scholar]
- 56.Liu Y, Saha S, Hoppe BO, Convertino M. Degrees and dollars – Health costs associated with suboptimal ambient temperature exposure. Sci. Total Environ. 2019;678:702–711. doi: 10.1016/j.scitotenv.2019.04.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gronlund CJ, Cameron L, Shea C, O’Neill MS. Assessing the magnitude and uncertainties of the burden of selected diseases attributable to extreme heat and extreme precipitation under a climate change scenario in Michigan for the period 2041–2070. Environ. Health. 2019;18:40. doi: 10.1186/s12940-019-0483-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Knowlton K, Rotkin-Ellman M, Geballe L, Max W, Solomon GM. Six climate change-related events in the United States accounted for about $14 billion in lost lives and health costs. Health Aff. (Millwood) 2011;30:2167–2176. doi: 10.1377/hlthaff.2011.0229. [DOI] [PubMed] [Google Scholar]
- 59.Díaz J, Sáez M, Carmona R, Mirón IJ, Barceló MA, Luna MY, Linares C. Mortality attributable to high temperatures over the 2021–2050 and 2051–2100 time horizons in Spain: Adaptation and economic estimate. Environ. Res. 2019;172:475–485. doi: 10.1016/j.envres.2019.02.041. [DOI] [PubMed] [Google Scholar]
- 60.Carmona R, Díaz J, Mirón IJ, Ortiz C, Luna MY, Linares C. Mortality attributable to extreme temperatures in Spain: A comparative analysis by city. Environ. Int. 2016;91:22–28. doi: 10.1016/j.envint.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 61.Roldán E, Gómez M, Pino MR, Díaz J. The impact of extremely high temperatures on mortality and mortality cost. Int. J. Environ. Health Res. 2015;25:277–287. doi: 10.1080/09603123.2014.938028. [DOI] [PubMed] [Google Scholar]
- 62.Hübler M, Klepper G, Peterson S. Costs of climate change: The effects of rising temperatures on health and productivity in Germany. Ecol. Econ. 2008;68:381–393. doi: 10.1016/j.ecolecon.2008.04.010. [DOI] [Google Scholar]
- 63.Karlsson M, Ziebarth NR. Population health effects and health-related costs of extreme temperatures: Comprehensive evidence from Germany. J. Environ. Econ. Manag. 2018;91:93–117. doi: 10.1016/j.jeem.2018.06.004. [DOI] [Google Scholar]
- 64.Yoon S-J, Oh I-H, Seo H-Y, Kim E-J. Measuring the burden of disease due to climate change and developing a forecast model in South Korea. Public Health. 2014;128:725–733. doi: 10.1016/j.puhe.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 65.Pantea, V., Overcenco, A., Osman, R.: Social and economic losses associated with extreme high temperatures of summer 2007 in the Republic of Moldova. Presented at the National Scientific and Practical Conference (2015)
- 66.Limaye VS, Vargo J, Harkey M, Holloway T, Patz JA. Climate change and heat-related excess mortality in the Eastern USA. EcoHealth. 2018;15:485–496. doi: 10.1007/s10393-018-1363-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wald A. Emergency department visits and costs for heat-related illness due to extreme heat or heat waves in the United States: An integrated review. Nurs. Econ. 2019;37:35–48. [Google Scholar]
- 68.Alberini A, Chiabai A, Nocella G. Valuing the mortality effects of heat waves. In: Menne B, Ebi K, editors. Climate Change Adaptation Strategies for Human Health. Berlin Germany: Steinkopff; 2006. [Google Scholar]
- 69.Jagai JS, Grossman E, Navon L, Sambanis A, Dorevitch S. Hospitalizations for heat-stress illness varies between rural and urban areas: an analysis of Illinois data, 1987–2014. Environ. Health. 2017;16:38. doi: 10.1186/s12940-017-0245-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schmeltz MT, Petkova EP, Gamble JL. Economic Burden of hospitalizations for heat-related illnesses in the United States, 2001–2010. Int. J. Environ. Res. Public. Health. 2016;13(9):894. doi: 10.3390/ijerph13090894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lin S, Hsu W-H, Van Zutphen AR, Saha S, Luber G, Hwang S-A. Excessive heat and respiratory hospitalizations in New York State: estimating current and future public health burden related to climate change. Environ. Health Perspect. 2012;120:1571–1577. doi: 10.1289/ehp.1104728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Toloo G, Hu W, FitzGerald G, Aitken P, Tong S. Projecting excess emergency department visits and associated costs in Brisbane, Australia, under population growth and climate change scenarios. Sci. Rep. 2015;5:12860. doi: 10.1038/srep12860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wagner V, Ung A, Calmet C, Pascal M. Evolution des vagues de chaleur et de la mortalité associée en France, 2004–2014. Bull Epidémiol Hebd. 2018;16–17:320–325. [Google Scholar]
- 74.Dialesandro J, Brazil N, Wheeler S, Abunnasr Y. Dimensions of thermal inequity: neighborhood social demographics and urban heat in the Southwestern U.S. Int. J. Environ. Res. Public. Health. 2021;18:941. doi: 10.3390/ijerph18030941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pascal M, Lagarrigue R, Laaidi K, Boulanger G, Denys S. Have health inequities, the COVID-19 pandemic and climate change led to the deadliest heatwave in France since 2003? Public Health. 2021;194:143–145. doi: 10.1016/j.puhe.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Toloo G, FitzGerald G, Aitken P, Verrall K, Tong S. Are heat warning systems effective? Environ. Health. 2013;12:27. doi: 10.1186/1476-069X-12-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ebi K, Teisberg T, Kalkstein L, Robinson L, Weiher R. Heat watch/warning systems save lives. Epidemiology. 2003;14(5):S35. doi: 10.1097/00001648-200309001-00064. [DOI] [Google Scholar]
- 78.Hutton G, Menne B. Economic evidence on the health impacts of climate change in Europe. Environ. Health Insights. 2014;8:43–52. doi: 10.4137/EHI.S16486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.ONERC: Climate Change: Costs of Impacts and Lines of Adaptation. Report to the Prime Minister and Parliament. Observatoire National sur les Effets du Réchauffement Climatique (National Observatory for the Impacts of Global Warming) (2009)
- 80.Laaidi K, Perrey C, Léon C, Mazzoni M, Beaudeau P. Connaissances et comportements des Français face à la canicule. Santé En Action. 2019;448:47–48. [Google Scholar]
- 81.Warren RF, Wilby RL, Brown K, Watkiss P, Betts RA, Murphy JM, Lowe JA. Advancing national climate change risk assessment to deliver national adaptation plans. Philos. Trans. R. Soc. A. 2018;376:20170295. doi: 10.1098/rsta.2017.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon request to the authors.
Code are available upon request to the authors.