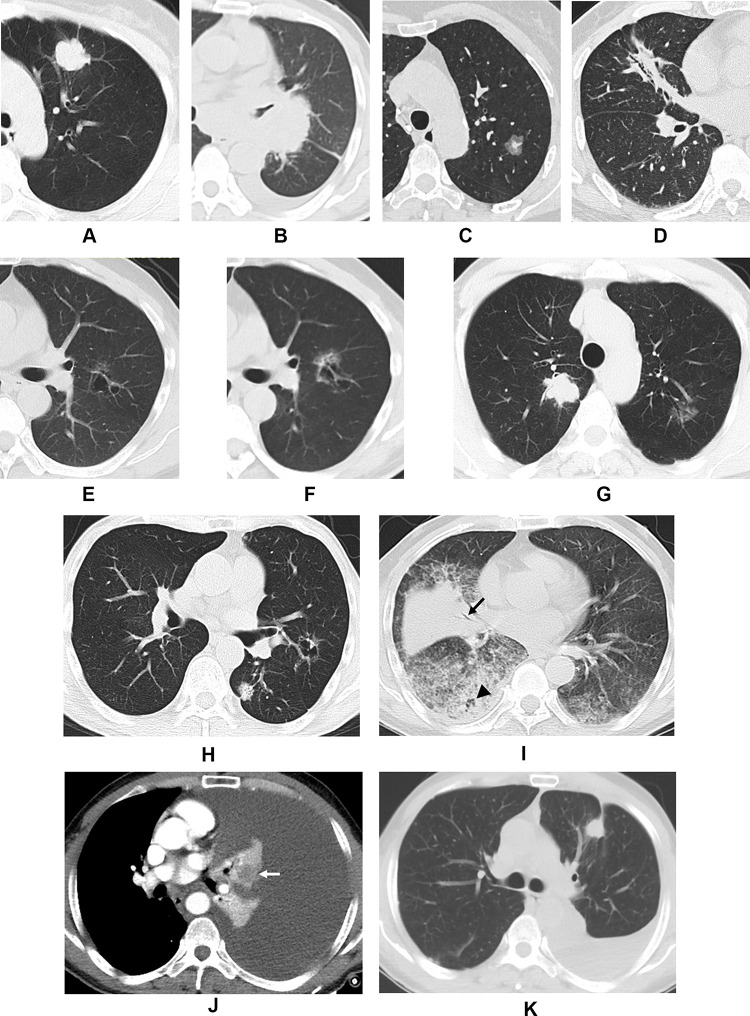
Figure 3.
Computed tomography images demonstrating the morphological classification of lung adenocarcinoma. Representative axial images of (A) Type I, showing a peripheral solid nodule with lobulation and pleural retraction in the left upper lobe; (B) Type II, showing a central solid mass in the left hilum with bronchiostenosis of the left upper lobe; (C) Type III, showing a subsolid nodule with irregular margin in the left upper lobe; (D) Type IV, showing focal triangular consolidation with bronchial leafless tree sign and pleural retraction in the right middle lobe; (E) Type V, showing a cystic airspace with irregular margins, septation, nonuniform cyst wall, and ground-glass opacity in the left upper lobe; (F) second image of (E) taken 45 months later showing an increase in lesion size with thickening of the cyst wall and increased ground-glass opacity; (G) Type VI in a 60-year-old male showing a solid nodule in the right upper lobe and a subsolid nodule in the left upper lobe which were surgically confirmed as adenocarcinoma; (H) Type VI in a 75-year-old male showing a solid nodule and a cystic airspace in the left lung which were surgically confirmed as adenocarcinoma; (I) Type VII, showing multiple consolidations and ground-glass opacity in both lungs with deadwood-like air bronchogram (black arrow) and air space (black arrowhead); (J) Type VIII, showing left massive pleural effusion with atelectasis in which the tumor was embedded, resulting in heterogeneous enhancement (white arrow), adenocarcinoma cells were found by cytological examination of the hydrothorax; (K) Follow-up imaging of (J) revealed the presence of a solid nodule (ie, a tumor) in the left upper lobe with partial absorption of the hydrothorax after two cycles of chemotherapy.