Figure 2. Interactions of islet macrophages and beta cells in obesity.
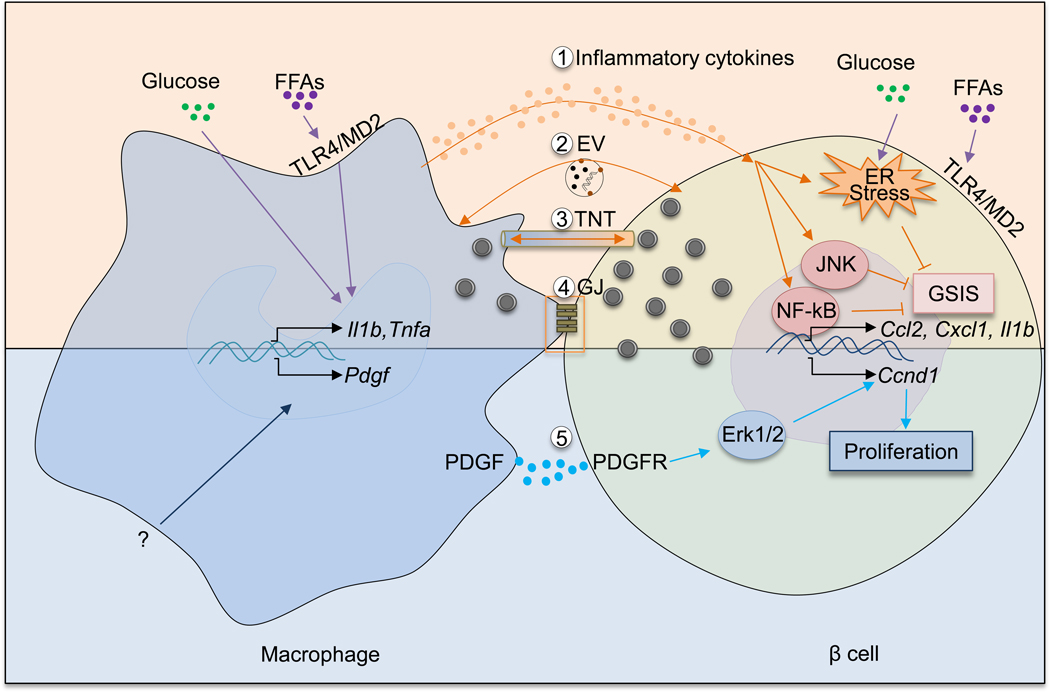
An increasing body of evidence supports the idea that islet macrophages influence beta cells in multiple ways. In obesity, elevated levels of glucose and free fatty acids can induce a pro-inflammatory phenotype of islet macrophages. As a result, macrophages produce increased amounts of proinflammatory cytokines such as IL-1β and TNF-α. These cytokines activate NF-κB and JNK pathways in beta cells and also exacerbate ER stress. Synergistically, these responses dampen beta cell GSIS. In addition to inflammatory cytokines, other mechanisms involving macrophage-mediated beta cell dysfunction exist. There mechanisms include: extracellular vesicles (EV) containing insulin released by beta cells and phagocytosed by islet macrophages; the formation of tunneling nanotubes (TNT) or gap junctions (GJ) between macrophages and beta cells allowing for bidirectional exchange of cellular contents. Obesity increases PDGF expression in islet macrophages via unclear mechanisms. Through PDGFR expressed in beta cells, PDGF promotes beta cell proliferation by activating downstream Erk signaling and inducing cell cycle gene (e.g., Ccnd1) expression.
