Abstract
Background
Blue zones are longevity hotspots around the world characterized by highest concentrations of healthy centenarians. Certified blue zone communities are designed by implementation of environmental and policy changes that promote healthy behaviors.
Objective
To examine the trends of prevalence of zero CAC, a marker of ideal cardiovascular and overall health status and burden of cardiovascular risk factors in Beach Cities/certified blue zones of Southern California and rest of California.
Methods
This is a population-based cohort study of persons aged 50 years or older in California, who underwent CAC screening between 2000 and 2019. A total of 3864 participants from Beach Cities of Southern California were identified by Zip Codes and compared with 35,537 participants from rest of California. We compared trends of prevalence of zero CAC and cardiovascular risk factors between the two groups, in 5-year intervals.
Results
Among 39,401 participants (mean age, 58.1 years; 36% women), 13,374 (34%) had zero CAC. The prevalence of CAC = 0 was significantly higher in Beach Cities compared to the rest of California (p < 0.001). Across the study period, the prevalence of cardiac risk factors including obesity, smoking, diabetes and hypertension remain significantly lower in Beach Cities. (p < 0.001)
Conclusions
This study, shows for the first time, that higher prevalence of zero CAC in Beach Cities of California, adds validity to excellent prognosis and longevity in these areas. The impact of policy implementation and environmental changes on lifestyle patterns, cardiovascular health and healthy ageing needs to be evaluated.
1. Introduction
“A man is as old as his coronary arteries.” – Thomas Sydenham, Physician (1624–1689).
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in most developed countries and continues to represent a significant public health and economic burden in the United States and worldwide. [1] According to American Heart Association (AHA) reports, every 2 in 10 deaths from coronary artery disease (CAD) happen in adults less than 65 years old [2]. Life expectancy in the United States witnessed a robust growth in the last century; however the expectancy growth rate since 2010 has stalled and most recently been declining [3]. The rate of decline in CVD mortality has since plateaued, likely contributing to decline in overall life expectancy [4]. The stagnating trajectory of life expectancy draws our attention to potential explanations including a concomitant rise in incidence of CVD and related risk factors, mainly obesity, diabetes and smoking epidemic over the last ten years [5].
A policy statement from the AHA on the 2030 Impact Goals further emphasizes the need for a broader view of cardiovascular surveillance metrics that can promote policy implementation and recommendations for ‘healthy ageing’ and increased life expectancy in the United States [6].
Coronary artery calcium (CAC), a validated measure of subclinical atherosclerosis can serve as a potential tool for risk stratification and surveillance for CVD, associated mortality and longevity [7,8]. There is indeed, a growing body of evidence supporting the concept that a CAC score of zero is a marker of not only excellent cardiovascular health, but also for ideal overall health status; zero CAC is associated with very low risk for cancer related and all-cause mortality [9,10]. In a recent meta-analysis, low CAC scores were inversely correlated with early detection of individuals prone to dementia and cognitive decline, an important risk factor contributing to quality of life metrics in older individuals [[11], [12], [13]]. This has led to an increasing interest in CAC as a marker of overall health, with zero CAC score serving as a surrogate measure for ‘healthy ageing’ and longevity [14].
We explore this concept in our study, as we evaluate the population level prevalence of zero CAC and examine the 20-year trends of zero CAC and burden of cardiovascular risk factors, in the Beach Cities of Southern California/Los Angeles (LA) county vs other regions of California, from 2000 to 2020. The Beach Cities of LA have been recently classified as a “certified Blue Zone community” through implementation of community-based public health initiatives focused on well-being and cardiovascular disease (CVD) prevention. These policies are reflective of the combination of lifestyle patterns and environmental changes, that are observed in rare longevity hotspots/blue zones around the world, mainly coastal areas such as the island of Okinawa in Japan, the peninsula of Nicoya in Costa Rica, the island of Ikaria in Greece, and the Mediterranean island of Sardinia [15]. The phenomenon of blue zones, where people live longer, healthier and happier lives have been identified in specific geographical regions worldwide and are characterized by the highest concentrations of healthy centenarians [16].
2. Methods
2.1. Study population
We included 39,401 study participants who live in California and underwent CAC scoring on non-contrast Cardiac CT from January 1, 2000 to December 31, 2019 at Lundquist Institute of Biomedical Innovation and Research at Harbor UCLA (Torrance, CA, USA). A total of 3864 participants from Beach Cities of Los Angeles were identified by zip codes (90254 for Hermosa Beach, 90277 and 90278 for Redondo Beach, 90266 and 90267 for Manhattan Beach) and compared with 35,537 participants from rest of California. Study cohort included patients who were asymptomatic with intermediate risk profile for cardiac disease risk assessment and patients with atypical chest pain who had a CAC score done along with a coronary CTA. All participants completed a self-reported questionnaire for collection of demographic information and major cardiovascular risk factors including diabetes, hypertension, hypercholesterolemia, cigarette smoking, and family history of premature CVD. Gender was self-identified by participants as “male” or “female” in the predefined questionnaire. Cigarette smoking was considered present if an individual was a smoker at the time of scanning and a past smoker included individuals who had smoked greater than 100 cigarettes during their lifetime, but quit at time of scanning. Dyslipidemia was considered to be present for any individual reporting a history of high total cholesterol, high low-density lipoprotein-cholesterol, low high-density lipoprotein-cholesterol, and high triglycerides, or current use of lipid-lowering therapy; Diabetes mellitus was considered present if participant answered “yes” to history of diabetes or to the use of oral anti–diabetes mellitus medications or insulin; Hypertension was defined as a self-reported history of high blood pressure or use of medications for treating high blood pressure. This study was approved by the ethics committee of Lundquist Institute. All patients gave written informed consent before taking part in the study.
2.2. Acquisition of non-contrast computed tomography for calcium scoring
Participants underwent ECG-gated CAC assessment on electron beam computed tomography (EBCT) with an Imatron C-150XL Ultrafast-computed tomography scanner (GE-Imatron, South San Francisco, CA), multi-detector 64-slice coronary computed tomography (CT) (Lightspeed VCT, General Electric Healthcare Technologies, Milwaukee, WI) and GE 256.
Each scan extended from 1 cm below the carina to the bottom of the heart for a complete acquisition. Scan parameters included prospective electrocardiogram-triggering (typically 60–80% of the R–R interval for EBCT, 65–80% for multi-detector CT), field of view was fixed at 35 cm, 512 × 512 matrix size, and a peak tube voltage of 120 kV. Slice thickness was 3 mm. CAC was quantified using the validated Agatston score method [17]. CAC measurements were performed on dedicated workstations using AW Volume Share TM, GE Medical Systems, Milwaukee, WI.
2.3. Statistical analysis
We performed cross sectional analysis to understand prevalence and distribution of CAC scores and CV risk factor burden across the two groups. Study period (Jan 1, 2000–Dec 31, 2019) was divided into 5 year intervals. Continuous variables are stated as the mean +SD, while categorical variables are reported as count and percentages. A Student’s t-test or chi-square test was used to test characteristics differences in the Beach Cities of Los Angeles versus the rest of California. CAC scores were categorized as zero, less than 100 and greater than 100. Age groups were categorized as less than 52 years, 52–59 years, 59–67 years and greater than 67 years old. A Z Test of proportions used to compare the cohorts when stratified by age groups.
Cochran-Armitage Trend Test was used to assess characteristics across time intervals and characteristic severity. Two-sided P values less than 0.05 were considered statistically significant. All statistical calculations were performed using SAS (Version 9.4, SAS Inc., Cary, NC).
3. Results
3.1. Baseline characteristics
Baseline characteristics of the study cohort are presented in Table 1. We included 39,401 consecutive study participants who live in California, 3864 participants from Beach Cities of Los Angeles were compared with 35,537 participants from rest of California. Mean (SD) age of participants was 58.1 (11.4) years and 36% were female.
Table 1.
Demographics in all subjects, the Rest of California Zone and the Beach Cities of California.
| All Subjects | Rest of California Zone | Beach Cities of California | P value | ||
|---|---|---|---|---|---|
| Age, years | 58.1 ± 11.4 | 58.2 ± 11.5 | 57.2 ± 10.5 | <.0001 | a |
| Body Mass Index >25, kg/m2 | 20,120 (51%) | 18,212 (51%) | 1908 (49%) | 0.0273 | b |
| Gender, Female | 14,168 (36%) | 12,818 (36%) | 1350 (35%) | 0.1678 | b |
| Diabetes Mellitus | 4092 (12%) | 3934 (13%) | 158 (5%) | <.0001 | b |
| Hypertension | 13,401 (40%) | 12,378 (41%) | 1023 (30%) | <.0001 | b |
| Hyperlipidemia | 19,941 (59%) | 17,912 (59%) | 2029 (59%) | 0.8078 | b |
| Past Smoker | 6516 (30%) | 5912 (30%) | 604 (26%) | <.0001 | b |
| Present Smoker | 2180 (7%) | 2019 (7%) | 161 (5%) | <.0001 | b |
| CAC = 0 | 13,374 (34%) | 11,917 (34%) | 1457 (38%) | <.0001 | b |
Mean ± Standard Deviation reported for age, all else reported as counts (percentage).
a: independent t-test, b: chi square test.
Individuals from Beach Cities of LA were less likely to smoke, have diabetes, hypertension, or history of prior MI. (p < 0.001) Mean age and history of hyperlipidemia were comparable between two groups. Individuals from Beach Cities of LA were more likely to have a positive family history for premature CAD (Table 1).
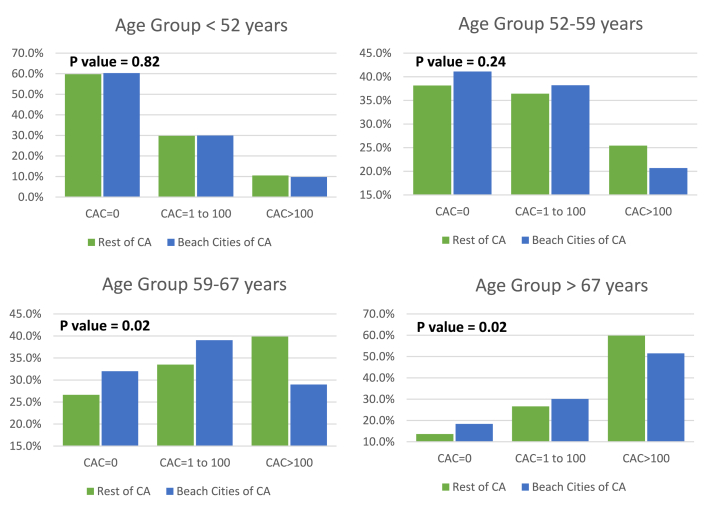
Prevalence of CAC scores across Beach Cities vs Rest of California, by age groups.
Across the study period, Beach Cities of LA have a higher prevalence of zero CAC compared to other areas in California (38% vs 34%, p < 0.001). When stratified by age, even in older age groups >67 years of age, Beach Cities of LA have a significantly higher proportion of subjects with CAC = 0 (18.4% vs 13.6%) and significantly lower proportion with CAC >100 (51.5% vs 59.8%) p value = 0.001, when compared with non-Blue Zone cities (Fig. 1).
Fig. 1.
Distribution of CAC scores in beach cities of california and Rest of california, by age Groups.
3.2. Trends in prevalence of zero CAC and cardiovascular risk factors
This is one of the first studies to examine prevalence of zero CAC as a surrogate for longevity and burden of CV risk factors, over a 20-year study period, across California (Table 2) (Fig. 3).
Table 2.
Trends observed in all subjects, the Rest of California Zone and the Beach Cities of California.
| 2000–2004 | 2005–2009 | 2010–2014 | 2015–2019 | |||||||
| Count | % | Count | % | Count | % | Count | % | P Trend∗ | ||
| CAC = 0 | All | 4001 | 33% | 2615 | 36% | 1928 | 33% | 4830 | 34% | 0.7805 |
| Rest of California Zone | 3608 | 33% | 2337 | 35% | 1769 | 33% | 4203 | 33% | 0.4092 | |
| Beach Cities | 393 | 36% | 278 | 40% | 159 | 34% | 627 | 39% | 0.0942 | |
| Body Mass Index>25 | All | 4985 | 63% | 2647 | 65% | 3160 | 64% | 9238 | 65% | <.0001 |
| Rest of California Zone | 4499 | 63% | 2386 | 65% | 2904 | 65% | 8336 | 67% | <.0001 | |
| Beach Cities | 486 | 63% | 261 | 59% | 256 | 60% | 902 | 56% | <.0001 | |
| Diabetes Mellitus | All | 760 | 8% | 817 | 18% | 635 | 12% | 1880 | 14% | <.0001 |
| Rest of California Zone | 731 | 8% | 796 | 20% | 617 | 13% | 1790 | 15% | <.0001 | |
| Beach Cities | 29 | 3% | 21 | 5% | 18 | 4% | 90 | 6% | 0.0098 | |
| Hypertension | All | 3134 | 32% | 2494 | 49% | 1890 | 36% | 5883 | 42% | <.0001 |
| Rest of California Zone | 2889 | 33% | 2313 | 51% | 1774 | 37% | 5402 | 44% | <.0001 | |
| Beach Cities | 245 | 27% | 181 | 39% | 116 | 26% | 481 | 31% | 0.4641 | |
| Past Smoker | All | 298 | 32% | 1060 | 50% | 920 | 20% | 4238 | 30% | <.0001 |
| Rest of California Zone | 276 | 33% | 957 | 51% | 866 | 20% | 3813 | 31% | <.0001 | |
| Beach Cities | 22 | 27% | 103 | 45% | 54 | 13% | 325 | 21% | 0.0397 | |
| Present Smoker | All | 841 | 9% | 407 | 9% | 263 | 5% | 669 | 5% | <.0001 |
| Rest of California Zone | 773 | 9% | 372 | 9% | 251 | 5% | 623 | 5% | <.0001 | |
| Beach Cities | 68 | 7% | 35 | 8% | 12 | 3% | 46 | 3% | <.0001 | |
| ∗Cochran-Armitage Trend Test for all p values | ||||||||||
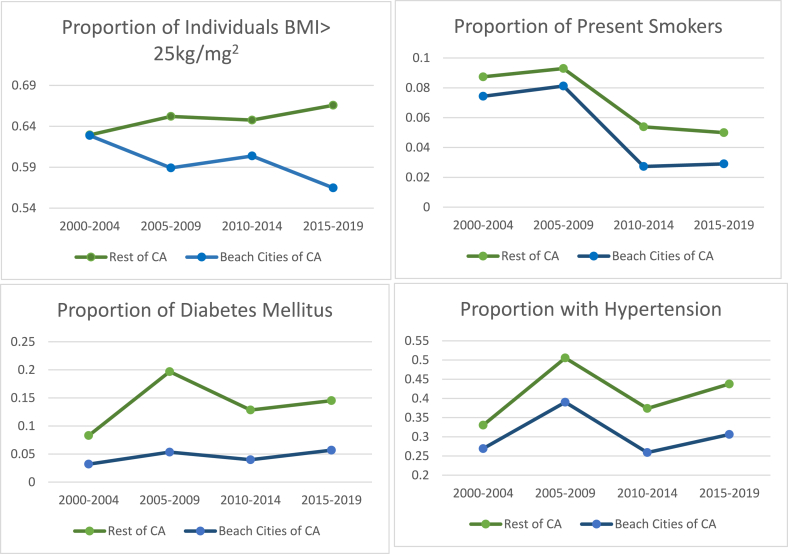
Fig. 3.
Trends of burden of CV risk factors in Beach Cities and Rest of California, across 20 year study period.
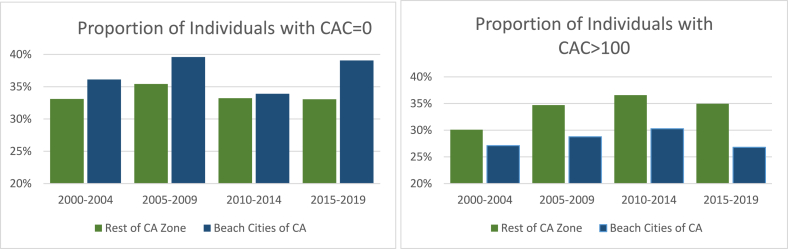
Across all time intervals, the prevalence of zero CAC was higher in Beach cities, compared to other cities in CA, respectively. Across the 20-year time period, there was a trend towards significance, with increase in proportion of individuals with zero CAC in Beach Cities of California (36%–39%, p value 0.09), while the proportion of individuals with zero CAC in rest of California remained at 33%, (p value 0.41). (Fig. 2).
Fig. 2.
Trends of prevalence of zero CAC and CAC>100 in Beach Cities and Rest of California, across 20 year study period.
There was a significant decrease in prevalence of elevated BMI > 25, classified as overweight or obese among the individuals in Beach Cities (from 63% to 56%; P ≤ 0.0001 for trend). The proportion of individuals with obese or overweight BMI significantly increased in the rest of CA, across the study period. (from 41% to 66%; P ≤ 0.0001 for trend).
The prevalence of DM was significantly lower in Beach cities across all time intervals. However, prevalence of DM significantly increased in other cities of CA (from 8% to 15%; P ≤ 0.0001 for trend).
For hypertension, across all time intervals, the prevalence was significantly lower in Beach Cities compared to other areas in CA. There was no significant difference in prevalence of hypertension, over the last 20 years in Beach Cities, but there was a significant increase in prevalence of HTN in the other areas across California from 33% to 44%; P < 0.0001 for trend).
For active smoking, across all time intervals, the prevalence was lower in Beach Cities compared to other areas in CA. Across the 20-year study period, there was a significant decline in prevalence of active smokers in Beach Cities compared to other cities, from 7% to 3%; P < 0.0001 for trend, and a decreasing trend was also observed in rest of CA, from 9% to 5%, P < 0.001). The proportion of individuals with history of past smoking remained lower in Beach cities (27%–21%, P value 0.039), compared to rest of CA (33%–31%, P value 0.001).
4. Discussion
This study, to the best of our knowledge, is the first to examine and report the last 20-year trends of prevalence of zero CAC score, a surrogate marker of excellent CV health and longevity, in Beach Cities vs other areas in California. Overall, our data reveals a higher prevalence of zero CAC in the certified blue zone communities compared to other areas of CA, across time intervals in the last 20 years, adding insights to expected longevity and excellent survival in these areas. A significant trend was observed for a decrease in the burden of cardiovascular risk factors, across time intervals in the last 20 years, in the Beach Cities compared to the other areas. Most recently from 2015 to 2019, we observe a significantly low prevalence of active smoking (3% vs 5%), past smoking (21% vs 31%), BMI > 25 (56% vs 66%), diabetes (6% vs 15%) and hypertension (31% vs 44%) in the Beach cities vs rest of CA, respectively. This is particularly relevant in the context of recent trends of significant increase in smoking, diabetes and obesity epidemic in the US, metrics identified as key risk factors impacting CVD mortality and life expectancy currently.
Prospective epidemiological studies have highlighted that persons with low CAC scores in middle age, experience lower rates of age-specific CVD events, all-cause mortality, incidence of cancer and increased life expectancy with higher self-reported quality of life standards [[18], [19], [20]]. In this context, the high prevalence of zero CAC across all age groups, including middle age and older individuals in Beach Cities of California represents a unique population with a favorable all-cause prognosis and can therefore, identify a community of “healthy ageing”. In Atherosclerosis Risk in Communities (ARIC) study, they demonstrated that 70% of adverse events related to CVD and stroke, could be eliminated through primordial prevention of risk behaviors and basic risk factors, mainly hypertension, high cholesterol, diabetes and smoking [21], [22]. Our study findings identify a similar correlation between low burden of risk factors/risk behaviors and zero CAC in the Beach Cities/certified blue zones over the last 20 years, with the ‘power of zero CAC’ offering additional prognostic information.
The Danish Twin study established that longevity is predominantly (approximately 80%), determined by our lifestyle choices, environmental influence on healthy habits and minimally influenced by genetic heritability [23]. Building on this concept, Blue Zones Project (BZP) adopts specific lifestyle habits shared among longevity hotspots around the world, and aims to transform communities through implementation of policy and environmental changes that can positively impact life expectancy [24]. In collaboration with preventive health agencies in Southern California such as Beach cities Health district and other key stakeholders, the BZP was introduced in the Beach Cities of Southern California in 2012 [15]. This included implementation of innovative, evidence-based policies and environmental engineering that aimed at improving daily physical movement, dietary patterns and building purposeful communities. For eg, BZP worked with city planners to institute community-wide smoking bans including ban on retail tobacco, engineered streets to make them walking and bike friendly, increased access to plant based menus in restaurants vs fast food, curating grocery stores to educate customers on healthy food options and encouraged mindful and purpose-based social support groups in the community. BZP has previously demonstrated population level benefits such as a 30% increase in physical activity in city of Albert Lea, MN and a 14% reduction in rates of obesity along with 30% reduction in smoking in the Beach Cities of LA, California [25], [26]. Our results suggest a similar trend with reduction in key population metrics since the implementation of BZP, where we observed a significant reduction in prevalence of smoking, obesity and diabetes in Beach Cities, compared to other areas of California. Previously, in a report from the Chicago Healthy Aging Study, the authors concluded that decade-long protective effects of low risk status in early to middle adulthood is likely mediated through a lower burden of subclinical atherosclerosis [20]. In a recent prospective study from UCC-SMART study group, they showed that healthy lifestyle improvements including smoking cessation, physical activity increase and weight loss, can contribute to CV risk reduction through lowering CRP concentrations in participants with established CVD [27]. Similarly, healthy dietary behaviors including low meat consumption, and high fruit and vegetable consumption have shown to attenuate the relationship between CAC and short telomere length, a marker of biological ageing and increased CV risk [28].
Our study therefore, supports the current consensus that CAC scores can serve as a phenotypic expression of overall health status, reflective of pathophysiological pathways such as chronic inflammation, that are usually accelerated by interaction of risk factors, lifestyle patterns, genetic and environmental factors over time [29].
4.1. Strengths and potential implications
The strengths of our study is inherent in its large sample size and the first time examination of trends of zero CAC prevalence and burden of CV risk factors to identify a community of healthy ageing in Beach Cities of California. Our study has a number of implications for the development of cardiovascular health/healthy longevity surveillance systems and population-based preventive strategies. The study results lend it support to the mission of AHA’s 2030 Impact Goals to live longer, healthier lives and highlights the need to understand the impact of community based initiatives designed to make healthy choices easier through institution of changes in environment and public policy that influence healthy behaviors. Our study adds further evidence supporting the use of CAC as key risk stratification tool and a potential metric for surveillance of healthy longevity and cardiovascular disease burden.
4.2. Limitations
There are a few limitations. Causal inference between effect of environmental factors and policy implementation on risk factor prevalence or CAC scores cannot be drawn due to cross sectional nature of analysis. In our study, Zero CAC may serve as a valuable potential surrogate to longevity but true longevity with chronological age/census data and survival has not been evaluated
Given the retrospective study design, the likelihood that people with a healthier lifestyle and behavior may have moved to beach cities of Southern California from neighboring cities and how that may influence results, needs to be explored in future studies. We do not have information on income levels or socio-economic status, key metrics that are known to affect outcomes and life-expectancy. However, a few differential influences in these metrics may be mitigated since they are all presenting to our CT lab for diagnostic evaluation and this can indirectly confirm access to basic healthcare/primary care physician and health insurance. Lack of use of race-specific cut points may influence the accuracy of estimates. We did not have information on behavioral patterns related to physical activity, dietary habits, consumption of fish and plant based food, all of which have been demonstrated to significantly influence cardiovascular health [30].
Disclosures
Dr. Matthew Budoff has received grant support from General Electric/GE and National Institute of Health/NIH. Other authors have no conflicts of interest to disclose.
Funding
This study received no funding.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Dr. Suvasini Lakshmanan, Dr. Sion K Roy and Dr. Matthew Budoff were responsible for drafting the article, and conceiving the study. April Kinninger was responsible for statistical analysis and data interpretation. Dr. Suraj Dahal, Dr. Vahid Rezvanizadeh, Dr. Divya Birudaraju, Dr. Khadije Ahmad, Dr. Ahmad K. Ghanem, Ilana Golub and Christopher Dailing were responsible for participant enrollment and acquisition of clinical data.
All authors granted final approval of the version to be published.
References
- 1.Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England) 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin E.J., Muntner P., Alonso A. Heart disease and stroke statistics-2019 update: a report from the American heart association. Circulation. 2019;139(10):e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 3.Woolf S.H., Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. Jama. 2019;322(20):1996–2016. doi: 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta N.K., Abrams L.R., Myrskyla M. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proc. Natl. Acad. Sci. U.S.A. 2020;117(13):6998–7000. doi: 10.1073/pnas.1920391117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho J.Y., Hendi A.S. Recent trends in life expectancy across high income countries: retrospective observational study. BMJ (Clin. Res. ed) 2018;362 doi: 10.1136/bmj.k2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roger V.L., Sidney S., Fairchild A.L. Recommendations for cardiovascular health and disease surveillance for 2030 and beyond: a policy statement from the American heart association. Circulation. 2020;141(9):e104–e119. doi: 10.1161/CIR.0000000000000756. [DOI] [PubMed] [Google Scholar]
- 7.Blaha M.J., Whelton S.P., Al Rifai M. 2020. Comparing risk scores in the prediction of coronary and cardiovascular deaths: coronary artery calcium consortium. JACC Cardiovascular imaging. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McClelland R.L., Chung H., Detrano R., Post W., Kronmal R.A. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2006;113(1):30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 9.Whelton S.P., Rifai M.A., Marshall C.H. Coronary artery calcium and the age-specific competing risk of cardiovascular versus cancer mortality: the coronary artery calcium consortium. Am J Med. 2020;133:e575–e583. doi: 10.1016/j.amjmed.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaikh K., Li D., Nakanishi R. Low short-term and long-term cardiovascular and all-cause mortality in absence of coronary artery calcium: a 22-year follow-up observational study from large cohort. J Diabetes Complicat. 2019;33(9):616–622. doi: 10.1016/j.jdiacomp.2019.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Xia C., Vonder M., Sidorenkov G. The relationship of coronary artery calcium and clinical coronary artery disease with cognitive function: a systematic review and meta-analysis. J Atherosclerosis Thromb. 2020;27:934–958. doi: 10.5551/jat.52928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manton K.G., Gu X., Lamb V.L. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proc. Natl. Acad. Sci. U.S.A. 2006;103(48):18374–18379. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Engberg H., Christensen K., Andersen-Ranberg K., Vaupel J.W., Jeune B. Improving activities of daily living in Danish centenarians--but only in women: a comparative study of two birth cohorts born in 1895 and 1905. J. Gerontol. Series A, Biol. Sci. Med. Sci. 2008;63(11):1186–1192. doi: 10.1093/gerona/63.11.1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blaha M.J., Cainzos-Achirica M., Dardari Z. All-cause and cause-specific mortality in individuals with zero and minimal coronary artery calcium: a long-term, competing risk analysis in the Coronary Artery Calcium Consortium. Atherosclerosis. 2020;294:72–79. doi: 10.1016/j.atherosclerosis.2019.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buettner D., Skemp S. Blue zones: lessons from the world’s longest lived. Am J Lifestyle Med. 2016;10(5):318–321. doi: 10.1177/1559827616637066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poulain M., Pes G.M., Grasland C. Identification of a geographic area characterized by extreme longevity in the Sardinia island: the AKEA study. Exp Gerontol. 2004;39(9):1423–1429. doi: 10.1016/j.exger.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 17.Agatston A.S., Janowitz W.R., Hildner F.J., Zusmer N.R., Viamonte M., Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 18.Budoff M.J.Y.R., Lopez V.A. Progression of coronary calcium and incident coronary heart disease events: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2013;61(12):1231–1239. doi: 10.1016/j.jacc.2012.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Min J.K.L.F., Gidseg D.S. Determinants of coronary calcium conversion among patients with a normal coronary calcium scan: what is the "warranty period" for remaining normal? J Am Coll Cardiol. 2010;55(11):1110–1117. doi: 10.1016/j.jacc.2009.08.088. [DOI] [PubMed] [Google Scholar]
- 20.Berry J.D., Mehta A., Lin K. Association of long-term risk factor levels with carotid atherosclerosis: the Chicago healthy aging magnetic resonance imaging plaque study (CHAMPS) Circul. Cardiovascular Imag. 2019;12(9) doi: 10.1161/CIRCIMAGING.119.009226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hozawa A., Folsom A.R., Sharrett A.R., Chambless L.E. Absolute and attributable risks of cardiovascular disease incidence in relation to optimal and borderline risk factors: comparison of African American with white subjects--Atherosclerosis Risk in Communities Study. Arch Intern Med. 2007;167(6):573–579. doi: 10.1001/archinte.167.6.573. [DOI] [PubMed] [Google Scholar]
- 22.Folsom A.R., Yamagishi K., Hozawa A., Chambless L.E. Absolute and attributable risks of heart failure incidence in relation to optimal risk factors. Circulation Heart Failure. 2009;2(1):11–17. doi: 10.1161/CIRCHEARTFAILURE.108.794933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herskind A.M., McGue M., Holm N.V., Sørensen T.I., Harvald B., Vaupel J.W. The heritability of human longevity: a population-based study of 2872 Danish twin pairs born 1870-1900. Hum Genet. 1996;97(3):319–323. doi: 10.1007/BF02185763. [DOI] [PubMed] [Google Scholar]
- 24.Vegi A.S.F., Fernandes Filho E.I., Pessoa M.C., Ramos K.L., Ribeiro A.Q. [Walkability and healthy aging: an analytical proposal for small and medium-sized Brazilian cities] Cad Saúde Pública. 2020;36(3) doi: 10.1590/0102-311x00215218. [DOI] [PubMed] [Google Scholar]
- 25.Buettner D. The blue zones: 9 lessons for living longer from the people who’ve lived the longest. Washington DNGS.
- 26.Buettner D. The blue zones solution: eating and living like the world’s healthiest people. Washington DNGS.
- 27.van ’t Klooster C.C., van der Graaf Y., Ridker P.M. The relation between healthy lifestyle changes and decrease in systemic inflammation in patients with stable cardiovascular disease. Atherosclerosis. 2020;301:37–43. doi: 10.1016/j.atherosclerosis.2020.03.022. [DOI] [PubMed] [Google Scholar]
- 28.Diaz V.A., Mainous A.G., 3rd, Everett C.J., Schoepf U.J., Codd V., Samani N.J. Effect of healthy lifestyle behaviors on the association between leukocyte telomere length and coronary artery calcium. Am J Cardiol. 2010;106(5):659–663. doi: 10.1016/j.amjcard.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen H.L., Liu J., Del Castillo M., Shah T. Role of coronary calcium score to identify candidates for ASCVD prevention. Curr Atherosclerosis Rep. 2019;21(12):53. doi: 10.1007/s11883-019-0812-8. [DOI] [PubMed] [Google Scholar]
- 30.Han L., You D., Ma W. National trends in American heart association revised life’s simple 7 metrics associated with risk of mortality among US adults. JAMA Network Open. 2019;2(10) doi: 10.1001/jamanetworkopen.2019.13131. [DOI] [PMC free article] [PubMed] [Google Scholar]