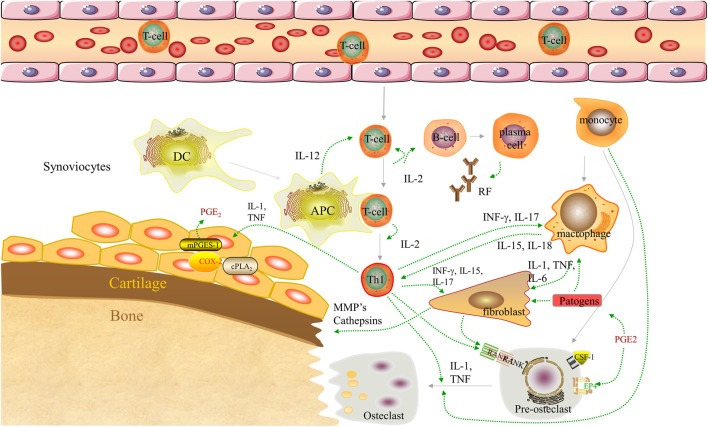
FIGURE 1.
Pathogenesis of RA. Dendritic cells complexed with autoantigen to activate naive T cells. Differentiated T cells stimulate B cells to produce autoantibodies [rheumatoid factor (RF)]. B cells present autoantigens to T cells, leading to their activation. Synovial macrophages are activated by T cells to release pro-inflammatory cytokines (TNF-α, IL-1, and IL-6), driving the activation of synovial fibroblasts and inducing osteoclast production. In addition, the monocyte subpopulations of the arthritic synovium can differentiate into macrophages and osteoclasts. Collectively, these components play an important role in the destruction of bones, cartilage, and the synovium. APC, antigen-presenting cell; COX-2, cyclooxygenase-2; cPLA2, cyosolic phospholipase A2; CSF-1, colony-stimulating factor-1; DC, dendritic cell; EP4, prostaglandin E receptor subtype 4; IFN-ɣ, interferon-gamma; IL-, interleukin; MMP, matrix metalloproteinase; mPGES-1, microsomal prostaglandin E synthase-1; PGE2, prostaglandin E2; PGF2, prostaglandin F2; RA, rheumatoid arthritis; RANK, receptor activator of nuclear factor-kB; Th1, T helper 1; TNF-α, tumor necrosis factor α.