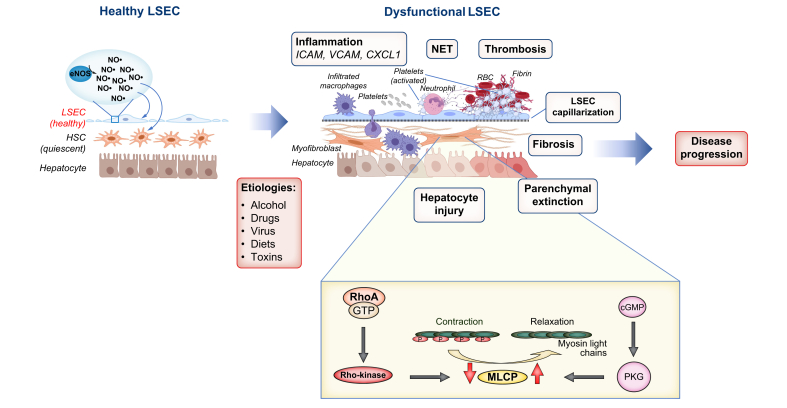
Fig. 1.
Liver sinusoidal cell dysfunction in liver pathogenesis.
Normal LSEC function is necessary for liver homeostasis. Various aetiologies can cause LSECs to become dysfunctional, leading to disease progression. Capillarisation is the loss of fenestrae and appearance of a basement membrane in LSECs. eNOS-derived NO plays a pivotal role in liver homeostasis by regulating vascular tone, maintaining fenestrae, maintaining HSCs in a quiescent state and blocking platelet attachments to endothelial cells among other functions. LSEC dysfunction often precedes pathological events, including inflammation, NET formation, microvascular thrombosis, parenchymal extinction (regions of tissue loss and fibrosis secondary to vascular obstruction and microvascular thrombosis), hepatocyte injury and fibrosis, leading to the development of portal hypertension. By contrast, in HSCs, calcium-independent contraction is mainly regulated by MLCP, which is inhibited by the RhoA/Rho-kinase pathway and activated by the NO/PKG-pathway. CXCL1, chemokine (C-X-C motif) ligand 1; HSCs, hepatic stellate cells; ICAM, intercellular adhesion molecule; LSECs, liver sinusoidal endothelial cells; MLCP, myosin light-chain phosphatase; NO, nitric oxide; NET, neutrophil extracellular trap; PKG, cGMP-dependent kinase; VCAM, vascular cell adhesion molecule.