Abstract
Background
The Gulf Cooperation Council (GCC), with a predominant ‘youth bulge’ among its 54 million people, has witnessed an exponential increase in research pertinent to child and adolescent mental health (CAMH). Aside from a few narrative reviews, to date, no critical appraisal examining the magnitude of CAMH has emerged from this region.
Aims
This study aimed to report the prevalence rates of CAMH disorders in the GCC through a systematic review of the existing literature followed by a meta-analysis.
Methods
A systematic review of the literature from the six GCC countries (Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates) was conducted. The databases used included Scopus, ProQuest, Pubmed, and a final check was performed on Google Scholar to account for any remaining studies that may have still been under review. Meta analytic techniques were then used to estimate prevalence rates of each specific mental disorder, i.e. ADHD, depression, anxiety, stress, eating disorders, and tobacco use disorder.
Results
A total of 33 studies from the six countries were included. The pooled prevalence of ADHD as per the Vanderbilt ADHD Diagnostic Rating Scale (VADHDDRS), clinical judgments, Attention Deficit Disorders Evaluation Scale (ADDES), and the Strengths and Difficulties Questionnaire (SDQ) was found to be 13.125%, 13.38%, 26.135%, and 12.83%, respectively. The pooled prevalence of depressive symptoms solicited by the Patient Health Questionnaire (PHQ-9), Depression, Anxiety, and Stress Scale (DASS), and Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI Kid) was 44.684%, 45.09%, and 26.12%, respectively. The pooled prevalence of anxiety according to the DASS and the MINI Kid was 57.04% and 17.27%, respectively, while the pooled prevalence of stress as per the DASS was found to be 43.15%. The pooled prevalence of disordered eating solicited by the Eating Attitudes Test (EAT-26) was 31.55%. Lastly, the pooled prevalence of tobacco use disorder per the Global Youth Tobacco Survey was 19.39%.
Discussion
To date, this is the first systematic review and meta-analysis of its kind from the GCC. The prevalence rate of CAMH disorders appears to be in the upper range of international trends. The higher rates could be attributed to the existing studies using suboptimal methodological approaches and instruments to solicit the presence of CAMH.
Keywords: Child and adolescent mental health disorders, GCC, Systematic review, Metaanalysis, ADHD, Depression, Anxiety, Stress, Eating disorders, Tobacco use disorder
1. Introduction
Neurodevelopmental behavioral and cognitive disorders and the variant spectrums categorized under the umbrella of child and adolescent mental health (CAMH) disorders have increasingly been recognized worldwide [1]. Empirical studies have indicated that most of the social deficits and dependence in adulthood begin during the childhood and adolescent periods [2]. In this regard, the presence of CAMH disorders often impedes children and adolescents from developing meaningful existence and good quality of life. There is also an added disadvantage of living with the stigma of a culturally devalued mental condition. CAMH disorders have been reported to occur among one out of six children in the industrialized countries of Western Europe, North America, and the Pacific Rim [3]. It is unclear whether the rising tide of such disorders reflects the new approaches to screening, identification, and case ascertainment, or the ever-expanding ‘youth bulge’ whereby an increase in the pediatric population in society has invariably caused an increase in the number of those diagnosed with CAMH disorders. Both epigenetic and nongenetic factors have been implicated in the identification of these disorders [4]. As CAMH disorders seem to be increasing in prevalence, nongenetic origins are also likely to be intertwined in shaping their expression, although this is yet to be well-established [4]. The high variability of incidence found across varied populations suggests that socio-cultural or ecological factors are likely to play a substantial role in the trajectory of the aforementioned set of disorders. Globally, the rate of CAMH disorders among children and adolescents have been reported to vary from 7.2% to 13.4% [[5], [6], [7], [8]].
Despite the phenomenon of the ‘youth bulge’ and the fact that 80% of the population resides in non-industrialized countries, not much has been documented on the magnitude of CAMH disorders in such non-industrialized countries, sometimes known as emerging economies or societies in transition. The six Arabian Gulf countries forming the Gulf Cooperation Council (GCC) (the United Arab Emirates, Saudi Arabia, Qatar, Oman, Kuwait, and Bahrain) appear to exhibit a preponderance of this aforementioned ‘youth bulge’. Demographically, the GCC is characterized by the ‘second phase of demography in transition’ [9]. Accordingly, this phase is often characterized by high fertility rates and the resultant birth rate, and the preponderance of a pyramid-like population structure [10].
In this context, systematic clinical observations suggest a high concentration of differently-abled children in the GCC [11]. This may stem from the high “prevalence of consanguinity among married couples and polygamous marriages particularly among older males, in addition to the high fertility rates and frequent births” (p.10). Furthermore, most GCC countries are yet to develop policies in support of the children and youth with special needs [12,13]. However, noteworthy is the fact that the phenomenon of a ‘stolen childhood’ appears to feature less in the GCC [14]. The GCC, in general, seems to form a part of those emerging economies where environment-related and infectious diseases appear to be diminishing, whereas the emergence of noncommunicable diseases including life-limiting diseases are increasingly being recognized [15]. Therefore, the quantification of the currently prevailing magnitude of CAMH disorders in the GCC is warranted in order to lay the groundwork for informed policies and allocation of resources and possible evidence-based prevention and intervention.
Though still in its nascent stage, literature documenting the magnitude of CAMH disorders has emerged in the GCC [16,17]. However, much of this literature has been limited to certain specific CAMH problems or narrative reviews [12,[18], [19], [20], [21], [22]]. To fill this gap in the literature, this study aimed to critically review the literature on the prevalence rates of CAMH disorders in the GCC. A glimpse into the literature shows that disorders such as anxiety, depression, stress, attention deficit hyperactivity disorder (ADHD), eating disorders (ED), and substance use disorder have received substantial attention in this region. Therefore, this appraisal would lay the groundwork for further investigations aiming to improve the identification of CAMH disorders. This, in turn, would contribute to the development of mechanisms for mitigation and safeguarding the wellbeing of both children and adolescents.
2. Methods
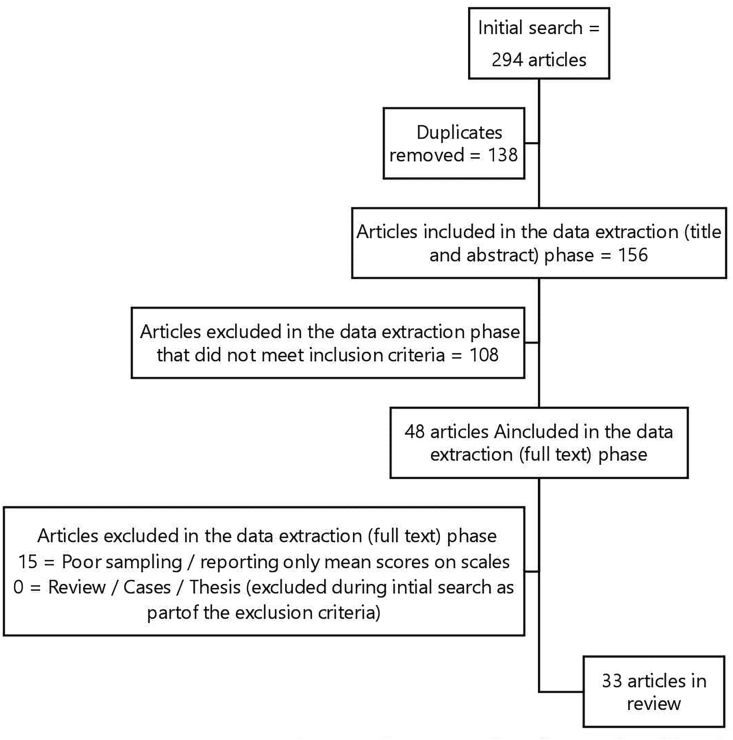
This systematic review was carried out following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Fig. 1) [23]. The study includes articles up to the year 2020, using keywords such as ‘mental disorders’, ‘prevalence’, and individual GCC country names (the United Arab Emirates, Saudi Arabia, Qatar, Oman, Kuwait, and Bahrain). The search results were screened to determine the eligibility criteria.
Fig. 1.
The PRISMA flow diagram describing the systematic review process.
2.1. Data retrieval strategies
Articles were obtained by searching various databases such as PsychINFO, Scopus, PubMed/Medline, ProQuest for English articles, and Al-Manhal for Arabic articles. The keywords used for English articles were divided into four levels as follows: Level 1 – mental disorders, psychiatric disorders, mental illnesses (other specific individual mental disorders such as ADHD, anxiety disorders, eating disorders, and PTSD); Level 2 – epidemiology, prevalence, survey; Level 3 – child, adolescent, preschool, toddler, youth, and “children with special needs”; and Level 4 – individual country name (GCC). For Arabic articles, keywords such as ‘الاضطرابات النفسية’, ‘الامراض النفسية’, and البلد were used. The following search methodology was not limited to a certain timeframe.
2.2. Inclusion and exclusion criteria
This article included studies that: (1) looked into mental disorders; (2) used validated questionnaires; (3) reported prevalence and sample size; and (4) were either in English or Arabic. Non-original studies such as reviews, duplicates, studies that did not report the prevalence, or studies that scored less than 90% on the Joanna Briggs Institute (JBI) evaluations were excluded. In addition, studies were excluded if they did not use a validated tool to measure the prevalence of a mental disorder or if the mental disorder was not classified by the Diagnostic and Statistical Manual of Mental Disorders or International Classification of Diseases [[24], [25], [26]].
2.3. Quality assessment
Based on the questions in the JBI guidelines [27], the three reviewers screened the title, abstract, results, discussion, and if included, other sections of each study. The scores of the JBI items ranged from 0 to 8. The inter rater reliability of the three reviewers was acceptable with an intraclass correlation coefficient (ICC) of 0.891.
The quality of the articles was assessed by answering 8 questions with answers given as Yes/No/Unclear/Not Applicable, from the JBI checklist which are: “Were the criteria for inclusion in the sample clearly defined?”, “Were the study subjects and the setting described in detail?”, “Was the exposure measured validly and reliably?”, “Were objective, standard criteria used for the measurement of the condition?”, “Were confounding factors identified?”, “Were there strategies to deal with confounding factors?”, “Were the outcomes measured validly and reliably?”, and “Was an appropriate statistical analysis used?”. The authors used a score of 7 or 8 “Yes's” as the cut-off to determine good quality articles.
2.4. Statistical analysis
The acquired data were analyzed by using the MedCalc 12 statistical Software. I² and Q statistics were used to assess heterogeneity across studies [28]. The data were considered homogeneous when I² was less than 50% and the Q statistic had a p-value greater than 10%, in which case a fixed effect model was used to produce pooled estimates; else, the random-effect model was used to interpret the results (i.e., the data were heterogenous) [29].
3. Results
The initial search yielded 294 useful studies. Three independent authors (MA, RA, and SM) excluded non-relevant and duplicate articles, which left a total of 156 articles for the full review. All 156 articles were scanned using the JBI appraisal checklist of scientific research articles [27]. The authors went through the reference list of all articles considered for the full review to properly check for any relevant studies that may have been missed out in the initial search. The other co-authors were consulted for input in case the three authors (MA, RA, and SM) were in disagreement.
3.1. Quality assessment
The following information was collected independently by the three reviewers (MA, RA, and SM): author names, date of publication, country, year of publication, year of study, sampling methods, age range, sample characteristics, sample size, the gender distribution of the sample, the measurement tool used, tool reliability, case diagnosis, the sum of diagnosed cases, and the prevalence percentages of each disorder.
Since none of the Arabic articles adhered to JBI guidelines, a total of 33 articles were included in the systematic review, of which 21 were used for the meta-analysis.
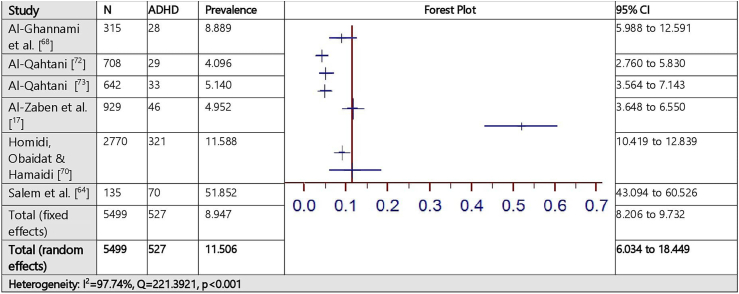
3.2. Prevalence of attention deficit hyperactivity disorder (ADHD) assessed by the Vanderbilt ADHD diagnostic rating scale (VADHDDRS)
The estimated prevalence of ADHD assessed by the VADHDDRS for 6 studies is demonstrated in Fig. 2. The pooled prevalence of ADHD in the total sample of 5499 was 11,506% (95% CI = 6.034–18.449%) based on the random effects model (I² = 97.74%, Q = 221.39, P < .001).
Fig. 2.
Prevalence estimates of attention deficit hyperactivity (ADHD) assessed by the Vanderbilt ADHD Diagnostic Scale.
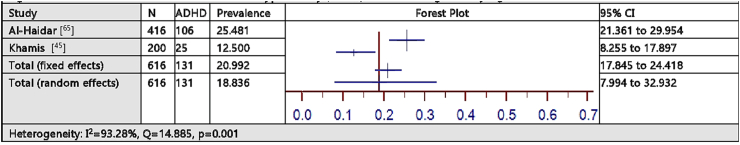
3.3. Prevalence of attention deficit hyperactivity disorder (ADHD) assessed using clinical judgment
The estimated prevalence of ADHD assessed using clinical judgment for 2 studies is demonstrated in Fig. 3. The pooled prevalence of ADHD in the total sample of 616 was 18.836% (95% CI = 7.994–32.932%) based on the random effects model (I² = 93.28%, Q = 14.885, P = .001).
Fig. 3.
Prevalence estimates of attention deficit hyperactivity (ADHD) assessed using clinical judgment.
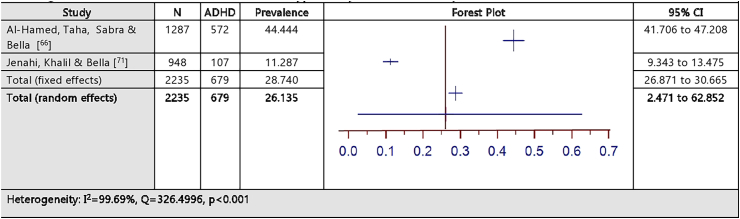
3.4. Prevalence of attention deficit hyperactivity disorder (ADHD) assessed by the Attention Deficit Disorders Evaluation Scale (ADDES)
The estimated prevalence of ADHD assessed by the ADDES for 2 studies is illustrated in Fig. 4. The pooled prevalence of ADHD in the total sample of 2235 was 26.135% (95% CI = 2.471–62.852%) based on the random effects model (I² = 99.69%, Q = 326.50, P < .001).
Fig. 4.
Prevalence estimates of attention deficit hyperactivity (ADHD) assessed by the Attention Deficit Disorders Evaluation Scale.
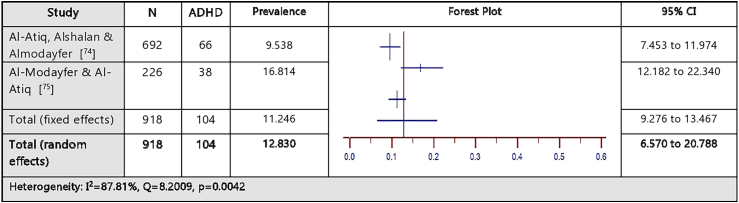
3.5. Prevalence of attention deficit hyperactivity disorder (ADHD) assessed by the Strengths and Difficulties Questionnaire (SDQ)
The estimated prevalence of ADHD assessed by the SDQ for 2 studies is illustrated in Fig. 5. The pooled prevalence of ADHD in the total sample of 918 was 12.830% (95% CI = 6.570–20.788%) based on the random effects model (I² = 87.81%, Q = 8.20, P = .0042).
Fig. 5.
Prevalence estimates of attention deficit hyperactivity (ADHD) assessed by the Strengths and Difficulties Questionnaire.
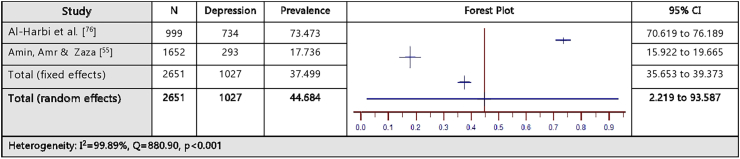
3.6. Prevalence of depression assessed by the Patient Health Questionnaire-9 (PHQ-9)
The estimated prevalence of depression assessed by the PHQ-9 for 2 studies is demonstrated in Fig. 6. The pooled prevalence of depression in the total sample of 2651 was 44.684% (95% CI = 2.219–93.567%) based on the random effects model (I² = 99.89%, Q = 880.90, P < .001).
Fig. 6.
Prevalence estimates of depression assessed by the Patient Health Questionnaire-9 (PHQ-9).
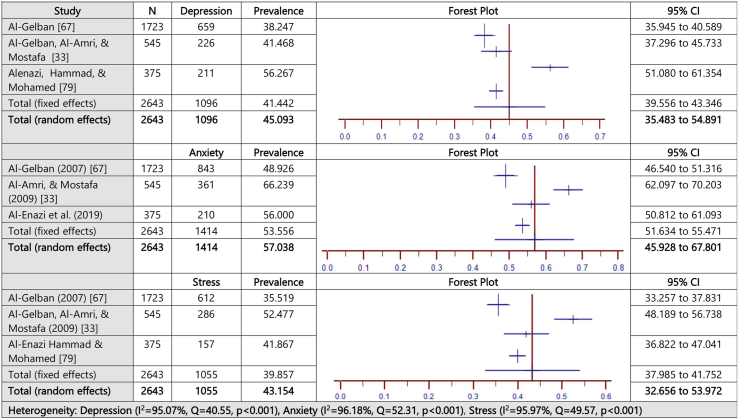
3.7. Prevalence of depression, anxiety, and stress assessed by the Depression, Anxiety, and Stress Scale (DASS)
The estimated prevalence of depression, anxiety, and stress assessed by the DASS for 3 studies is demonstrated in Fig. 7. The pooled prevalence of depression in the total sample of 2643 was 45.09% (95% CI = 35.48–54.89%) based on the random effects model (I² = 95.07%, Q = 40.55, P < .001). The pooled prevalence of anxiety was 57.04% (95% CI = 45.93–67.801%) based on the random effects model (I² = 96.18%, Q = 52.31, P < .001). The pooled prevalence of stress was 43.15% (95% CI = 32.66–53.97%) based on the random effects model (I² = 95.97%, Q = 49.57, P < .001).
Fig. 7.
Prevalence estimates of depression, anxiety, and stress assessed by the DASS.
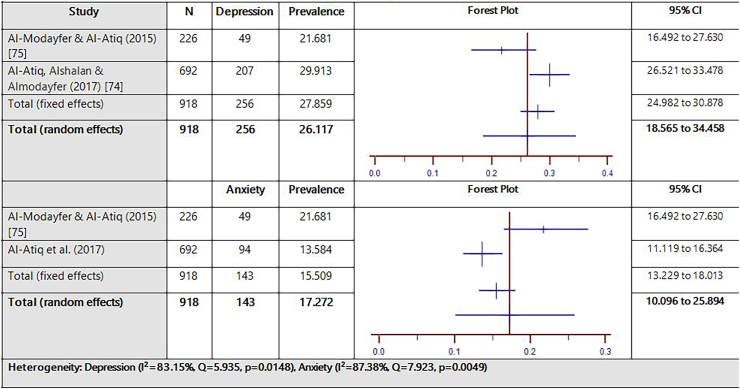
3.8. Prevalence of depression and anxiety assessed by the Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI kid)
The estimated prevalence of depression and anxiety assessed by the MINI-kid for 2 studies is illustrated in Fig. 8. The pooled prevalence of depression and anxiety in the total sample of 918 was 26.12% (95% CI = 18.57–34.46%) and 17.27% (95% CI = 10.10–25.89%), respectively, based on the random effects model (depression: I² = 83.15%, Q = 5.935, p = .0148; anxiety: I² = 87.38%, Q = 7.923, P = .0049).
Fig. 8.
Prevalence estimates of depression and anxiety assessed by the Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI Kid).
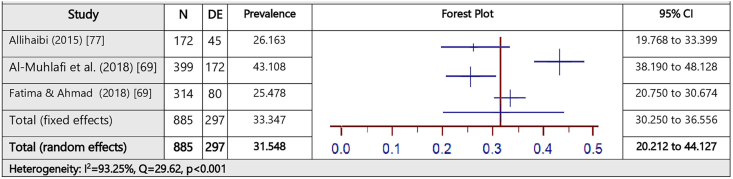
3.9. Prevalence of disordered eating assessed by the Eating Attitudes Test (EAT-26)
The estimated prevalence of disordered eating (DE) assessed by the EAT-26 for 3 studies is illustrated in Fig. 9. The pooled prevalence of disordered eating in the total sample of 885 was 31.55% (95% CI = 20.21–44.13%) based on the random effects model (I² = 93.25%, Q = 29.62, P < .001).
Fig. 9.
Prevalence estimates of disordered eating (DE) assessed by the Eating Attitudes Test (EAT-26).
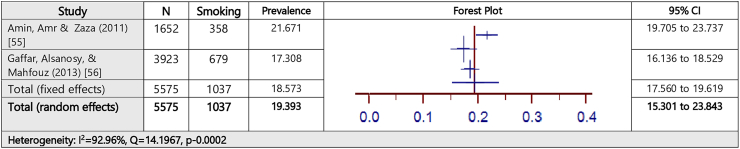
3.10. Prevalence of smoking assessed by the Global Youth Tobacco Survey (GYTS)
The estimated prevalence of smoking assessed by the GYTS for 2 studies is demonstrated in Fig. 10. The pooled prevalence of smoking in the total sample of 5575 was 19.39% (95% CI = 15.30–23.84%) based on the random effects model (I² = 92.96%, Q = 14.20, P = .0002).
Fig. 10.
Prevalence estimates of smoking assessed by the Global Youth Tobacco Survey.
3.11. Excluded studies
The current systematic review included 33 studies (Table 1) [[30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40],45,55,56,[64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74],[77], [78], [79], [80]].
Table 1.
Characteristics of studies included in Systematic Review [[30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40],45,55,56,[64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74],[77], [78], [79], [80]].
| No. | Author (year) | Country | Sample size (N) | Age range (years) | Study setting | Screening tool | Disorder screened | Positive cases (%) |
|---|---|---|---|---|---|---|---|---|
| 1 | Salem et al. (2014) [64] | Kuwait | 135 | 6–15 | Hospital | VADHDDRS-PRS (Arabic)/SSPI/WIS/MINI-KID | ADHD | ADHD = 70 (51.9%) |
| 2 | Bener et al. (2011) [30] | Qatar | 1703 | 6–18 | School | Clinical Impression | Phobias | Overall Phobias = 335 (19.7%) |
| 3 | Bradshaw & Kamal (2017) [31] | Qatar | 4489 | 6–19 | School | SNAP-IV RS | ADHD | ADHD = 373 (8.3%) |
| 4 | Alshaban et al. (2019) [32] | Qatar | 8676 | 5–12 | Schools and medical centers | SCQ/QSS-PTI/ADI-R/ADOS-2 | ASD | ASD = 1398 (0.79%) |
| 5 | Al-Gelban, Al-Amri, & Mostafa (2009) [33] | Saudi Arabia | 545 | 14–19 | School | SCL 90-R (Arabic) | Mental health symptoms | Depression = 76 (13.9%); Anxiety = 78 (14.3%) |
| 6 | Al-Haidar (2003) [65] | Saudi Arabia | 416 | 0–18 | Hospital | DSM III-R/DSM IV | ADHD | ADHD = 106 (25.5%) |
| 7 | Al Hamed, Taha, Sabra & Bella al. (2008) [66] | Saudi Arabia | 1287 | 6–13 | School | ADDES | ADHD | ADHD = 572 (45.11) |
| 8 | Al Gelban (2007) [67] | Saudi Arabia | 1723 | 15–19 | School | DASS | Depression, anxiety and stress | Depression = 659 (38.2%) Anxiety = 843 (48.9%) Stress = 612 (35.5%) |
| 9 | Al-Gelban, Al-Amri, & Mostafa (2009) [33] | Saudi Arabia | 545 | 14–20 | School | DASS | Depression, anxiety and stress | Depression = 226 (41.5%) Anxiety = 361 (66.2%) Stress = 286 (52.5%) |
| 10 | Al-Modayfer & Alatiq (2017) [75] | Saudi Arabia | 226 | 0–17 | Community | SDQ/MINI-KID | Psychiatric disorders | ADHD = 38 (17.0%) Any affective (depression) or anxiety disorder = 49 (21.7%) |
| 11 | Al-Qahtani and Al-Harbi (2017) [34] | Saudi Arabia | 347 | 17–19 | School | Taif Hospital Scales Series: Anxiety scale | Anxiety | Anxiety = 223 (64.3%) |
| 12 | Al-Sughayr and Ferwana (2012) [35] | Saudi Arabia | 354 | 17–20 | School | GHQ-28 | Psychiatric morbidity | Psychiatric morbidity = 170 (48%) |
| 13 | Alatiq, Alshalan, and Almodayfer (2010) [74] | Saudi Arabia | 692 | Mean = 16.9 SD = .02 |
School | SDQ/MINI-KID | Psychiatric disorders | ADHD = 66 (9.5%); Generalized Anxiety Disorder = 94 (13.64%) Conduct Disorder = 39 (5.66%) Dysthymia = 30 (4.37%) Anorexia Nervosa = 4 (0.58%) Bulimia Nervosa = 23 (3.34%) Substance Dependence/Abuse = 1 (0.14%) |
| 14 | Albuhairan et al. (2017) [36] | Saudi Arabia | 9073 | Mean = 15.8 SD = 1.84 |
School | Global school-based student health survey | Bullying, physical violence (PV), anxiety, and sadness | PV = 3021 (33.3%) Victims & perpetrator of PV = 1116 (12.3%) Victim (bullied) = 1923 (21.2%) Bullying & PV = 1043 (11.5%) |
| 15 | Alenazi, Hammad & Mohamed (2019) [79] | Saudi Arabia | 375 | 16–19 | School | DASS-42 | Depression/anxiety/stress | Depression = 211 (56.3%) Anxiety = 210 (56.0%) Stress = 157 (41.9%) |
| 16 | Alharbi et al. (2019) [77] | Saudi Arabia | 1245 | 13–19 | School | PHQ-9/GAD-7 | Depression/anxiety | Depression = 734 (73.5%) Anxiety = 620 (62.1%) |
| 17 | Allihaibi (2015) [78] | Saudi Arabia | 172 | 15–19 | School | EAT-26 | Disordered eating attitudes | DEA = 45 (26.2%) |
| 18 | Almuhlafi, Jamilah, Almutairi & Salam (2018) [69] | Saudi Arabia | 399 | Mean = 16.8 SD = 0.9 | School | EAT-26 | Disordered eating | Binge eating = 123 (30.8%) Purging = 28 (7.0%) Laxative usage = 21 (5.3%) |
| 19 | Almuneef (2019) [37] | Saudi Arabia | 10,156 | Mean = 34.3 SD = 11 |
Community | ACEIQ | Child sexual abuse (CSA) | Lifetime CSA (contact form) = 2112 (20.8%); Experienced Penetrating Sexual Abuse = 1016 (10%); Experienced non-penetrating sexual abuse = 1137 (11.2%) |
| 20 | Alqahtani (2012) [72] | Saudi Arabia | 708 | 7–9 | School | VADHDDRS | ADHD | ADHD = 29 (4.1%) |
| 21 | Alqahtani (2010) [73] | Saudi Arabia | 642 | 7–9 | School | DSM-IV-TR | ADHD | ADHD = 33 (5.0%) [DSM-IV-TR] |
| 22 | Alzaben et al. (2018) [17] | Saudi Arabia | 929 | 6–12 | School | VADHDDRS | ADHD | ADHD = 46 (11.6%) |
| 23 | Amin, Amr & Zaza (2011) [55] | Saudi Arabia | 1652 | 15–19 | School | GYTS/FT/PHQ-9/NCS | Tobacco use disorder | Smoking = 358 (21.7%) Cigarettes only = 165 (46.1%), Shisha = (WP or Maasel) = 134 (37.4%) Cigarettes and Shisha = 59 (16.5%) |
| 24 | Elarousy, & Al-Jadaani (2013) [38] | Saudi Arabia | 60 | 12–18 | Community | Specially designed, self-administered questionnaire | Emotional abuse | Rejecting = 54 (90.0%) Ignoring = 37 (61.7%) Terrorizing = 37 (61.7%) |
| 25 | Fatima & Ahmad (2018) [69] | Saudi Arabia | 314 | 15–19 | School | EAT-26 | Disordered Eating | Disordered Eating = 80 (25.4%) |
| 26 | Gaffar, Alsanosy & Mahfouz (2013) [56] | Saudi Arabia | 3923 | 12–21 | School | GYTSQ | Tobacco Use Disorder | Smoking = 679 (17.3%) |
| 27 | Homidi, Obaidat & Hamaidi (2018) [70] | Saudi Arabia | 2770 | 6–12 | School | ADHDS | ADHD | ADHD = 321 (11.6%) |
| 28 | Jenahi, Khalil, & Bella (2013) [71] | Saudi Arabia | 1009 | 6–15 | School | ADDES | ADHD | ADHD = 107 (11.3%) |
| 29 | Raheel (2015) [80] | Saudi Arabia | 1028 | 15–19 | School | BDI | Depression | Depression = 308 (30.0%) |
| 30 | Al-Yateem et al. (2020) [39] | UAE | 968 | 13–18 | School | SCARED | Anxiety | Anxiety = 271 (28.0%) |
| 31 | Khamis (2011) [45] | UAE | 200 | 11–14 | School | DSM-IV | ADHD | ADHD = 25 (12.5%) |
| 32 | Al-Ghannami et al. (2018) [68] | Oman | 328 | 9–10 | School | VADHDDRS-TAS | ADHD | ADHD = 28 (8.8%) |
| 33 | Afifi (2006) [40] | Oman | 500 | Mean = 16.99 SD = 0.99 |
School | CDIS | Depression | Depression = 91 (18.3%) |
ADHD = Attention deficit hyperactivity disorder; VADHDDRS=Vanderbilt ADHD diagnostic rating scale; TDR = Tool developed by the researchers; SNAP – IV RS = The Swanson, Nolan and Pelham Teacher and Parent Rating Scale; SCQ=Social Communication Questionnaire; QSS-PTI = Qatar School Survey Patient Telephone Interview; ASD = Autism Spectrum Disorders; ADI-R = Autism Diagnostic Interview-Revised; ADOS-2 = Autism Diagnostic Observation Schedule, Second Edition; SCL 90-R = Symptom-revised Checklist 90; DSM – III R = Diagnostic Statistical Manual, Third Edition, Revised; DSM – IV = Diagnostic Statistical Manual, Fourth Edition; ADDES = Attention Deficit Disorders Evaluation Scale; DASS = Depression, Anxiety and Stress Scale; SDQ=Strengths and difficulties Questionnaire; MINI-KID=The Mini-International Neuropsychiatric Interview for Children and Adolescents; GHQ-28 = General Health Questionnaire; PHQ-9 = Patient Health Questionnaire-9; GAD-7 = General Anxiety Disorder-7; EAT-26 = Eating Attitude Test-26; ACEIQ = Adverse Childhood Experience International Questionnaire; ODD = Occupational Defiant Disorder; CD = Conduct Disorder; GYTS = Global Youth Tobacco Survey; ADHDS = Attention Deficit Hyperactivity Disorder Scale; ADHD IA = ADHD/inattentive type; ADHD HI = ADHD/hyperactivity type; ADHD C = ADHD/combined type; BDI=Beck depression inventory; SCARED=Screen for Child Anxiety Related Disorders Scale; VADHDDRS-PRS=Vanderbilt ADHD Diagnostic Parent Rating Scale (VADPRS); CDIS=Children's Depression Inventory scale; FT=Fagerstrom Test (nicotine dependence); NCS=National comorbidity survey; DEA = Disordered eating attitudes; VADHDDRS-TAS, National Initiative for Children's Health Quality Vanderbilt Assessment Scales-Teacher Assessment Scale; WIS=Wechsler Intelligence Scale for Children II; SSPI=Semi-structured psychiatric interview.
However, noteworthy is the fact that the final meta-analysis includes only 21 of them (Table 2) [17,33,45,55,56,[64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79]]. The reason for the exclusion of these 12 studies is that, unlike the rest, it was not possible to group them into any of the tool-based categories since each study covered a unique disorder by itself including child abuse, language disorders, and autism spectrum disorders. Additionally, studies were also excluded if they measured the five disorders included in the current meta-analysis, but used a unique tool that was not used by at least one other study. In this regard, studies covering mental health symptoms, in general, were also excluded.
Table 2.
Evaluation of the qualifying papers using the JBI guidelines [17,33,45,55,56,[64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79]].
| No. | Criteria | Qa | Qb | Qc | Qd | Qe | Qf | Qg | Qh |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Salem et al. [64] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2 | Al-Haidar [65] | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| 3 | Al Hamed, Taha, Sabra & Bella [66] | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| 4 | Al Gelban [67] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 5 | Al-Gelban, Al-Amri, & Mostafa [33] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 6 | Al-Ghannami et al. [68] | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes |
| 7 | Khamis [45] | Unclear | Yes | Yes | Yes | Yes | Yes | Unclear | Yes |
| 8 | Almuhlafi, Jamilah, Almutairi & Salam [69] | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes |
| 9 | Fatima & Ahmad [70] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 10 | Gaffar, Alsanosy, & Mahfouz [56] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 11 | Homidi, Obaidat & Hamaidi [71] | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| 12 | Jenahi, Khalil, and Bella [72] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 13 | Al Qahtani [73] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 14 | AlZaben et al. [17] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 15 | Al Qahtani [74] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 16 | Alatiq, Alshalan, and Almodayfer [75] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 17 | Almodayfer and Alatiq [76] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 18 | AlHarbi et al. [77] | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| 19 | Amin, Amr & Zaza [55] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 20 | Allihaibi [78] | No | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 21 | Alenazi, Hammad, and Mohamed [79] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
Were The Criteria For Inclusion In The Sample Clearly Defined?.
Were The Study Subjects And The Setting Described In Detail?.
Was The Exposure Measured In A Valid And Reliable Way?.
Were Objective, Standard Criteria Used For Measurement Of The Condition?.
Were Confounding Factors Identified?.
Were Strategies To Deal With Confounding Factors Stated?.
Were The Outcomes Measured In A Valid And Reliable Way?.
Was Appropriate Statistical Analysis Used?.
Bener et al. investigated 1703 school children aged between 6 and 18 years for phobias [30]. The authors found that although the overall prevalence of phobias was found to be 19.7%, social phobia, agoraphobia, specific phobia, and medical phobia were 12.7%, 8.6%, 7.5%, and 7% respectively. Bradshaw and Kamal [31] examined the prevalence of ADHD among 2195 school students (6 to 19-year-olds) to find an 8.3% prevalence rate. In investigating the prevalence of autism spectrum disorder among 5 to 12-year-olds, Alshaban et al. [32] reported a 0.79% prevalence rate. In 2009, Al-Gelban, Al-Amri, and Mostafa [33] examined the prevalence of various general mental health symptoms among 545 secondary school girls aged 14–19 years. In this study, the authors reported the prevalence of depression (13.9%), anxiety (14.3%), phobic anxiety (16.5%), psychoticism (14.7%), somatization (14.1%), interpersonal sensitivity (13.8%), paranoid ideation (13.8%), hostility (12.8%), and obsessive-compulsive behavior (12.3%).
Al-Qahtani and Al-Harbi investigated 347 female students for anxiety [34]. Overall, anxiety was found to be prevalent in 64.3% of the samples with 39% of them having high non-morbid anxiety and 25% with high morbid anxiety. In a study conducted by Al-Sughayr and Ferwana, 216 females and 138 males aged 17 years and above were examined [35]. A prevalence of 48% was found in the total sample. Furthermore, when dividing the sample into specific age groups such as “below 18 years”, a prevalence of 46.5% was reported. Albuhairan et al. studied 4300 female and 4773 male students for bullying, physical violence, anxiety, and sadness [36]. Their results demonstrate a prevalence of 33.3% and 21.2% for physical violence and bullying, respectively. Almuneef examined 4865 females and 5291 males for child sexual abuse and found that 2112 participants experienced lifetime contact forms of sexual abuse in which 1016 of them experienced penetrating sexual abuse [37].
Elarousy and Al-Jadaani examined emotional abuse in 23 females and 37 males aged between 12 and 18 years [38]. The study reported the prevalence of emotional abuse in three aspects: rejecting emotional abuse (90%), ignoring emotional abuse (61.7%), and terrorizing emotional abuse = 61.7%. Fatima and Ahmed (2018) investigated disordered eating in a sample of 314 females, aged 15–19 years old. The overall prevalence rate based on the EAT-26) was found to be 25.4%. Another study conducted by Al-Yateem et al. looked into the prevalence rate of anxiety in 331 females and 637 males, aged between 13 and 18 years old [39]. The anxiety rate was found to be 28%. Finally, Afifi examined 240 females and 260 males students for depression. A prevalence rate of 18.3% was found in the overall sample [40].
4. Discussion
The current study examined the prevalence rates of child and adolescent mental health (CAMH) disorders in the GCC, also known as the emerging economy or society in transition with the bulk of its population being under the age of 20 years [10]. Research on CAMH has significantly increased in the past decade in the GCC, and therefore, the time is ripe to critically appraise the existing literature so that informed policies could be contemplated to safeguard the wellbeing of the youth [41]. Although mental health disorders viewed from biomedical perspectives are generally highly stigmatized in traditional societies and often a pejorative of traditional healing systems, community surveys have suggested that there is a rising tide of CAMH disorders amid the lack of dedicated services and suboptimal health utilization of biomedical health services [42,43].
The findings of the present study suggest that CAMH disorders are increasingly recognized. In this study, the prevalence of attention deficit hyperactive disorder (ADHD) ranged from 12.83% to 26.14%, depressive symptoms ranged 6.12%–45.09%, anxiety ranged from 17.27% to 57.04%, disordered eating was 31.55%, while tobacco use disorder was 19.39%. In the section below, each disorder will be recapitulated within the background literature.
In the GCC, the present appraisal suggests that the prevalence rate of ADHD ranged from 12.83% to 26.14%. The present ranges appeared to be less extreme from previous studies compared with Yemen and UAE which ranged from 1.3% to 34.5%, respectively [44,45]. In comparison with international trends, ADHD appears to range from 6–7% when DSM-IV criteria are employed, whereas they plummet down to 1–2% when using the ICD-10 among children and adolescents. Polanczyk, de Lima, Horta, Biederman, and Rohde have suggested that this discrepancy stemmed from differing modes of case ascertainment, diagnosis, and catchment area [46]. In addition to clinical judgments, most of the quantification of ADHD in the GCC was conducted by using structured questionnaires (Vanderbilt ADHD Diagnostic Rating Scale, Attention Deficit Disorders Evaluation Scale, and the Strengths and Difficulties Questionnaire). This may explain the higher rate compared to the global trend.
Depression-like symptoms have been documented in various parts of the world among children and adolescents [7]. The rate of depressive symptoms appears to increase over time among children and adolescents. For example, in China, Li et al. conducted a systematic review and meta analysis and reported that the prevalence of depressive symptoms was 18.4% in 2000, but the rate increased to 26.3% after 2016 [47]. Lopez et al. have projected that depressive symptoms will be the leading cause of disability and dependency by 2030 [48]. Depression in children and adolescents not only impedes educational attainment, but it also acts as a strong risk factor for poor physical health outcomes and dented subsequent quality of life and meaningful existence [49]. Polanczyk et al. have reported a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents including depressive symptoms [7]. The study accrued 41 articles that fulfilled the study criteria from 27 countries around the world. The worldwide prevalence of any depressive disorder was 2.6%. In the present study, depressive symptoms ranged from 6.12% to 45.09% which were solicited using checklists such as the Patient Health Questionnaire, Depression, Anxiety and Stress Scale, and Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI Kid). Overall, the upper range from the GCC appears to exceed the global rate. This issue warrants further scrutiny since the previously held view was that depressive symptoms unless presented as a ‘somatic metaphor’ is likely to be rare in those societies where the individual is ushered into the collective mindset [50]. There are some suggestions that cultural patterning in traditional societies as those in the GCC tend to abhor the expression of emotion, since this is deemed to be disruptive to social equilibrium in collective societies [51]. In contrast to such sociological perspectives, children and adolescents in the GCC appear to have a high rate of depressive symptoms, and the rates seemingly exceed the global rate
In contrast to depressive illness which often appears as being cognitive, somatic or a combination of these, anxiety is mainly of somatic nature (e.g., palpitation) and is likely to be endorsed even in those societies where those with psychological symptoms are ostracized. This appraisal suggests that anxiety in children and adolescents in the GCC range from 17.27% to 57.04%. Two instruments – Depression, Anxiety and Stress Scale, and Mini-International Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI Kid)–fulfilled the study criteria. The global prevalence of any anxiety disorder has been reported to range from 0.9% to 28.3%, even if it is quantified using structured interviews compared to semi-structured interviews which often result in more conservative estimates [7,52]. Again, the rate in the GCC appears to exceed those from other parts of the world. Studies are, therefore, warranted to examine whether the observed rate represents genuine trends on the ground or are intimately tied to the socio-cultural artifact of quantifying psychological symptoms. These artifacts often lack the central features and thus are prone to ‘false-positives’ which, in turn, trigger inflation of the rate of psychological symptoms.
Disordered eating and disturbed body image, which sometimes manifest as full-fledged eating disorders, had initially been conceptualized as a ‘culture-bound’ syndrome of the industrialized countries of North America and Western Europe owing to the alleged social pressure dispensed by the media which ‘glorifies’ a body image favoring thinness in women [43]. However, more recently, eating disorders have been documented to be common in non-western countries [53]. The scrutinized studies appear to be limited to disordered eating rather than full-blown eating disorders as featured in the international psychiatric nosology such as ICD and DSM. The present pooled prevalence of disordered eating in the GCC, tapped by the Eating Attitudes Test (EAT-26), is found to be 31.55%. Globally, disordered eating was found to be 22.07%, whereas eating disorders have been reported to be 1.01% [47]. This suggests that the pooled prevalence of disordered eating in the GCC also appears to be in the upper range of the global trend.
Besides being viewed as alien in conservative or sometimes puritanical societies, evidence suggests that substance use disorders are increasingly coming to the fore in the GCC [54]. Most of the substances that have been reported to be used in other parts of the world are now being reported in the GCC as well. The GCC is steadily becoming the hub for international transshipment and tourism. With the bulk of the population below the age of 20 years, it should therefore be expected that ‘adolescent turmoil’ often observed in other societies is also likely to exist in the GCC. In the present data, two studies (n = 5575) filled the inclusion criterion which only focused on tobacco use disorder [55,56]. The pooled prevalence was 19.39%. Tobacco use disorder has been reported using various methods of quantification and the present rate is reported using data from the study using the Global Youth Tobacco Survey. Jawad, Lee, and Millett have scrutinized the prevalence of tobacco consumption using the Global Adult Tobacco Survey among South-East Asian countries [57]. The prevalence rate appeared to range from 5.9% to 56.5%. Jawad, Khader, and Millett have reported the prevalence estimates for current tobacco smoking by logistics laid out by Global Adult Tobacco Survey in the Fertile Crescent region (Jordan, Syria, Lebanon, and Palestine) [58]. The prevalence rate varied from 23.2% to 39.5%. Baška et al. have reported the prevalence rate of 22% and 18% for males and females 13–15 years old, respectively, among 25 European countries [59]. Therefore, the present pooled prevalence of 19.39% appears to be in the lower range compared with other regions of the world.
4.1. Limitations
Some of the obvious limitations that go beyond the meta-analysis and systematic review are highlighted below. Firstly, existing literature on child and adolescent mental health (CAMH) in the GCC has not been explicit in terms of the specific age group of the study population. Therefore, it was not feasible to split the sample using conventional demarcations such as preschooler, grade-schooler, and teen. Such an undertaking could have simplified and provided a clearer understanding of the developmental trends. Second, there are concerns regarding the validity and utility of the currently employed diagnostic approaches. Three studies used clinical judgments based on DSM criteria. A study has indicated that clinical judgment tends to be less reliable and may lead to biased assessment [60]. The rest of the assessments were performed through standardized psychiatric interviews. It has been well-established that structured questionnaires or symptom checklists are likely to give spurious results [61]. The advantage of the gold-standard interview is that it has the potential to identify the presence of disorders that are not otherwise specified (for example, EDNOS) which are likely to be rife in cross-cultural populations such as those in the GCC [62]. Related to this, most of the information was solicited from the accompanying caregiver and it is unclear who constitutes a caregiver. Third, though standard tools used to assess CAMH are essential for international comparison, most of them emanate from Euro-American nosographic perspectives. Little effort was taken to subject tools to cross-cultural validation so their utility could resonate with local symptoms of distress. It has been widely established that psychiatric distress tends to manifest as per the local idiom of distress [63]. Therefore, studies aiming to develop culturally sensitive diagnostic tools are needed in order to ensure that culture-specific idioms of distress are taken into account. Related to this, some studies have examined the concept of stress in the GCC. However, stress is yet to be a featured diagnostic criterion in the international nomenclature. Four, for proper epidemiological studies, community surveys are optimal compared to clinical settings. In the present review, a significant number of studies constituted a self-selective cohort where most participants were recruited from schools or clinical settings. Community surveys with a national catchment are therefore warranted. Five, outcome measures and what constitutes CAMH disorders were not completely homogeneous across accrued articles. Finally, studies in the GCC appear to be skewed towards a particular subtype of child and adolescent disorders. It remains unclear whether the GCC does indeed have a high concentration of such clinical populations, or if this rate of prevalence is simply due to a lack of diagnostic expertise wherein other common childhood disorders such as language and scholastic disorders are overlooked.
5. Conclusion
Despite the aforementioned limitations, countries in the GCC have recently witnessed an increase in research pertinent to CAMH. This indeed corroborates the existing trend of this region being in its second stage of demographic transition characterized by a high fertility rate and a predominance of the pediatric population in its pyramid-like population structure. The present appraisal indicates that the most common CAMH disorders are increasingly being reported in the GCC. The global rate of CAMH disorders varies from 12.83% to 57.04%, with ADHD at 12.83%–26.135%, depressive symptoms at 26.12%–45.09%, anxiety at 17.27%–57.04%, disordered eating at 31.55%, and tobacco use disorder at 19.39%. It should be noted that modeling the quantification of CAMH disorders using local tools is likely to limit their international comparability. Moreover, adhering purely to international screening tools has the potential to give rise to spurious figures owing to the lack of cultural adaptability of these measures. In the future, the quantification of CAMH disorders in the GCC should reflect two contesting backgrounds: the relevance of integrating global or international trends and the paramount importance of viewing CAMH through a more socio-culturally sensitive lens.
Ethics and consent approval
NA.
Consent for publication
NA.
Availability of data and materials
This is a research article and all data generated or analyzed during this study are included in this published article.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
MA, MC, RB, MF, SM, and SA had full access to all of the data in the study and take responsibility for the integrity and the accuracy of the data analysis as they were involved in the analysis and interpretation of the data. MC contributed to technical and statistical analysis. MA, MC, RB, MF, SM, and SA were involved in the drafting of the manuscript. All the authors were involved in the critical revision of different drafts of the manuscript.
Declaration of competing interest
None. The authors declare that there are no conflicts of/or competing interests.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
Contributor Information
Moon Fai Chan, Email: moonf@squ.edu.om.
Rola Al Balushi, Email: rola.iqbal@hotmail.com.
Maryam Al Falahi, Email: azz.ayo.525@gmail.com.
Sangeetha Mahadevan, Email: sm5520@nyu.edu.
Muna Al Saadoon, Email: munasa@squ.edu.om.
Samir Al-Adawi, Email: samir.al-adawi@fulbrightmail.org, samir.al-adawi@fulbrightmail.org.
References
- 1.Almandil N.B., Alkuroud D.N., AbdulAzeez S., AlSulaiman A., Elaissari A., Borgio J.F. Environmental and genetic factors in autism spectrum disorders: special emphasis on data from arabian studies. Int J Environ Res Publ Health. 2019 Feb 23;16(4):658. doi: 10.3390/ijerph16040658. PMID: 30813406; PMCID: PMC6406800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatr. 2005 Jun;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Bitsko R.H., Holbrook J.R., Robinson L.R., Kaminski J.W., Ghandour R., Smith C. Health care, family, and community factors associated with mental, behavioral, and developmental disorders in early childhood—United States, 2011–2012. MMWR Morb Mortal Wkly Rep. 2016;65:221–226. doi: 10.15585/mmwr.mm6509a1. [DOI] [PubMed] [Google Scholar]
- 4.Thygesen J.H., Presman A., Harju-Seppänen J., Irizar H., Jones R., Kuchenbaecker K., Lin K. Genetic copy number variants, cognition and psychosis: a meta-analysis and a family study. Mol Psychiatr. 2020 Jul 27 doi: 10.1038/s41380-020-0820-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas R., Sanders S., Doust J., Beller E., Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015 Apr 1;135(4):e994–e1001. doi: 10.1542/peds.2014-3482. [DOI] [PubMed] [Google Scholar]
- 6.Silva S.A., Silva S.U., Ronca D.B., Gonçalves V.S.S., Dutra E.S., Carvalho K.M.B. Common mental disorders prevalence in adolescents: a systematic review and meta-analyses. PloS One. 2020;15(4) doi: 10.1371/journal.pone.0232007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Polanczyk G.V., Salum G.A., Sugaya L.S., Caye A., Rohde L.A. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. JCPP (J Child Psychol Psychiatry) 2015 Mar;56(3):345–365. doi: 10.1111/jcpp.12381. Epub 2015 Feb 3. PMID: 25649325. [DOI] [PubMed] [Google Scholar]
- 8.Malhotra S., Patra B.N. Prevalence of child and adolescent psychiatric disorders in India: a systematic review and meta-analysis. Child Adolesc Psychiatr Ment Health. 2014 Jul 21;8:22. doi: 10.1186/1753-2000-8-22. Erratum in: Child Adolesc Psychiatry Ment Health. 2017 Jul 12;11:39. PMID: 25071865; PMCID: PMC4113132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Omran A.R. The epidemiologic transition: a theory of the epidemiology of population change. Milbank Q. 2005. 1971;83(4):731–757. doi: 10.1111/j.1468-0009.2005.00398.x. PMID: 16279965; PMCID: PMC2690264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zaiceva A., Zimmermann K.F. Chapter 3 - migration and the demographic shift. In: Piggott John, Woodland Alan., editors. Handbook of the economics of population aging, 2016. vol. 1. 2016. pp. 119–177. [DOI] [Google Scholar]
- 11.Al Qudsi S.S. 2006. Unemployment evolution in the GCC economies: its nature and relationship to output gaps, labor market study No. 22, Abu Dhabi: center for market research & information (CLMRI)http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.494.5816&rep=rep1&type=pdf [Google Scholar]
- 12.Qoronfleh M.W., Essa M.M., Alharahsheh S.T., Al-Farsi Y.M., Al-Adawi S. Autism in the Gulf states: a regional overview. Front Biosci. 2019;24:334–346. doi: 10.2741/4721. [DOI] [PubMed] [Google Scholar]
- 13.Al-Adawi S. Emergence of diseases of affluence in Oman: where do they feature in the health research agenda? Sultan Qaboos University Medical Journal. 2006;6(2):3–9. [PMC free article] [PubMed] [Google Scholar]
- 14.GBD 2017 Child and Adolescent Health Collaborators. Reiner R.C., Jr., Olsen H.E., Ikeda C.T. Diseases, injuries, and risk factors in child and adolescent health, 1990 to 2017: findings from the global burden of diseases, injuries, and risk factors 2017 study. JAMA Pediatr. 2019 Jun 1;173(6) doi: 10.1001/jamapediatrics.2019.0337. Epub 2019 Jun 3. PMID: 31034019; PMCID: PMC6547084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Adawi S.S.H., Al Lamki Z., Moustafa A.A., Alkindi S., Al-Adawi S. Springer International Publishing; 2020. Palliative care in a society in transition: how to Address the unmet biopsychosocial needs in Oman. Handbook of healthcare in the Arab world; pp. 1–20. [DOI] [Google Scholar]
- 16.Bener A., Qahtani R.A., Abdelaal I. The prevalence of ADHD among primary school children in an Arabian society. J Atten Disord. 2006 Aug;10(1):77–82. doi: 10.1177/1087054705284500. PMID: 16840595. [DOI] [PubMed] [Google Scholar]
- 17.AlZaben F.N., Sehlo M.G., Alghamdi W.A., Tayeb H.O., Khalifa D.A., Mira A.T., Alshuaibi A.M., Alguthmi M.A., Derham A.A., Koenig H.G. Prevalence of attention deficit hyperactivity disorder and comorbid psychiatric and behavioral problems among primary school students in western Saudi Arabia. Saudi Med J. 2018 Jan;39(1):52–58. doi: 10.15537/smj.2018.1.21288. PMID: 29332109; PMCID: PMC5885121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salhia H.O., Al-Nasser L.A., Taher L.S., Al-Khathaami A.M., El-Metwally A.A. Systemic review of the epidemiology of autism in Arab Gulf countries. Neurosciences. 2014;19(4):291. [PMC free article] [PubMed] [Google Scholar]
- 19.Farah L.G., Fayyad J.A., Eapen V., Cassir Y., Salamoun M.M., Tabet C.C., Mneimneh Z.N., Karam E.G. ADHD in the Arab world: a review of epidemiologic studies. J Atten Disord. 2009;(3):211–222. doi: 10.1177/1087054708325976. [DOI] [PubMed] [Google Scholar]
- 20.Al-Saadoon M., Al-Adawi M., Al-Adawi S. Socio-cultural constraints in protecting child rights in a society in transition: a review and synthesis from Oman. Child Indic Res. 2020 Aug 7:1–29. doi: 10.1007/s12187-020-09759-z. Epub ahead of print. PMID: 32837628; PMCID: PMC7412292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lansford J.E., Ben Brik A., Al Fara H. A framework for child well-being in the Gulf countries. Child Ind Res. 2019;12:1971–1987. doi: 10.1007/s12187-019-9620-5. [DOI] [Google Scholar]
- 22.Kelly M.P., Alireza I., Busch H.E. An overview of autism and applied behavior analysis in the Gulf cooperation Council in the Middle East. Rev J Autism Dev Disord. 2016;3:154–164. doi: 10.1007/s40489-016-0073-1. [DOI] [Google Scholar]
- 23.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009 Oct;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. Epub 2009 Jul 23. PMID: 19631508. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association . American Psychiatric Publishing, Inc; 2000. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. [Google Scholar]
- 25.American Psychiatric Association . fifth ed. American Psychiatric Press; Washington, DC: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 26.World Health Organization . World Health Organization; Geneva: 1992. The ICD-10 classification of mental and behavioral disorders: clinical descriptions and diagnostic guidelines. [Google Scholar]
- 27.Joanna Briggs Institute (JBI) Systematic Review . 2020. JBI reviewer's manual.https://wiki.joannabriggs.org/display/MANUAL/3.2.6+Selection+of+studies [Google Scholar]
- 28.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003 Sep 6;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. PMID: 12958120; PMCID: PMC192859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DerSimonian R., Laird N. Meta-analysis in clinical trials. Contr Clin Trials. 1986 Sep;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. PMID: 3802833. [DOI] [PubMed] [Google Scholar]
- 30.Bener A., Ghuloum S., Dafeeah E.E. Prevalence of common phobias and their socio-demographic correlates in children and adolescents in a traditional developing society. Afr J Psychiatr. 2011 May;14(2):140–145. doi: 10.4314/ajpsy.v14i2.6. PMID: 21687913. [DOI] [PubMed] [Google Scholar]
- 31.Bradshaw L.G., Kamal M. Prevalence of ADHD in Qatari school-age children. J Atten Disord. 2017 Mar;21(5):442–449. doi: 10.1177/1087054713517545. Epub 2016 Jul 27. PMID: 24412969. [DOI] [PubMed] [Google Scholar]
- 32.Alshaban F., Aldosari M., Al-Shammari H., El-Hag S., Ghazal I., Tolefat M., Ali M., Kamal M., Abdel Aati N., Abeidah M., Saad A.H., Dekair L., Al Khasawneh M., Ramsay K., Fombonne E. Prevalence and correlates of autism spectrum disorder in Qatar: a national study. JCPP (J Child Psychol Psychiatry) 2019 Dec;60(12):1254–1268. doi: 10.1111/jcpp.13066. Epub 2019 May 8. PMID: 31069792; PMCID: PMC6899566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Gelban K.S., Al-Amri H.S., Mostafa O.A. Prevalence of depression, anxiety and stress as measured by the depression, anxiety, and stress scale (DASS-42) among secondary school girls in abha, Saudi Arabia. Sultan Qaboos Univ Med J. 2009 Aug;9(2):140–147. Epub 2009 Jun 30. PMID: 21509290; PMCID: PMC3074779. [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Qahtani A.M., Al-Harbi M.B. Prevalence and risk factors of anxiety among female governmental secondary schools students in Al-madinah, Saudi Arabia. Indian Journal of Pharmaceutical Education and Research. 2017;51(1):137–143. [Google Scholar]
- 35.Al-Sughayr A.M., Ferwana M.S. Prevalence of mental disorders among high school students in National Guard Housing, Riyadh, Saudi Arabia. J Family Community Med. 2012 Jan;19(1):47–51. doi: 10.4103/2230-8229.94015. PMID: 22518359; PMCID: PMC3326771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.AlBuhairan F., Abou Abbas O., El Sayed D., Badri M., Alshahri S., de Vries N. The relationship of bullying and physical violence to mental health and academic performance: a cross-sectional study among adolescents in Kingdom of Saudi Arabia. Int J Pediatr Adolesc Med. 2017 Jun;4(2):61–65. doi: 10.1016/j.ijpam.2016.12.005. Epub 2017 Feb 9. PMID: 30805503; PMCID: PMC6372492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Almuneef M. Long term consequences of child sexual abuse in Saudi Arabia: a report from national study. Child Abuse Negl. 2019 Mar 11 doi: 10.1016/j.chiabu.2019.03.003. Epub ahead of print. PMID: 30871806. [DOI] [PubMed] [Google Scholar]
- 38.Elarousy W., Al-Jadaani M. Emotional abuse among children: a study in Jeddah, Saudi Arabia. East Mediterr Health J. 2013 Oct;19(10):869–875. PMID: 24313151. [PubMed] [Google Scholar]
- 39.Al-Yateem N., Rossiter R.C., Al-Shujairi A., Radwan H., Awad M., Fakhry R., Mahmoud I. Anxiety related disorders in adolescents in the United Arab Emirates: a population based cross-sectional study. BMC Pediatr. 2020;20(1):1–8. doi: 10.1186/s12887-020-02155-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Afifi M. Depression in adolescents: gender differences in Oman and Egypt. East Mediterr Health J. 2006 Jan-Mar;12(1–2):61–71. PMID: 17037222. [PubMed] [Google Scholar]
- 41.James S.L., Castle C.D., Dingels Z.V. Global injury morbidity and mortality from 1990 to 2017: results from the global burden of disease study 2017 [published correction appears in inj prev. 2020 sep 28. Inj Prev. 2020;26(Supp 1):i96–i114. doi: 10.1136/injuryprev-2019-043494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maalouf F.T., Alamiri B., Atweh S., Becker A.E., Cheour M., Darwish H., Ghandour L.A., Ghuloum S., Hamze M., Karam E., Khoury B., Khoury S.J., Mokdad A., Meho L.I., Okasha T., Reed G.M., Sbaity E., Zeinoun P., Akl E.A. Mental health research in the Arab region: challenges and call for action. Lancet Psychiatry. 2019 Nov;6(11):961–966. doi: 10.1016/S2215-0366(19)30124-5. Epub 2019 Jul 18. PMID: 31327707. [DOI] [PubMed] [Google Scholar]
- 43.Jaju S., Al-Adawi S., Al-Kharusi H., Morsi M., Al-Riyami A. Prevalence and age-of-onset distributions of DSM IV mental disorders and their severity among school going Omani adolescents and youths: WMH-CIDI findings. Child Adolesc Psychiatr Ment Health. 2009 Sep 26;3(1):29. doi: 10.1186/1753-2000-3-29. PMID: 19781098; PMCID: PMC2761855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alyahri A., Goodman R. The prevalence of DSM-IV psychiatric disorders among 7-10 year old Yemeni schoolchildren. Soc Psychiatr Psychiatr Epidemiol. 2008 Mar;43(3):224–230. doi: 10.1007/s00127-007-0293-x. Epub 2007 Nov 26. PMID: 18040589. [DOI] [PubMed] [Google Scholar]
- 45.Khamis V. Attention-deficit and hyperactivity among school-age United Arab Emirates children. Int J Spec Educ. 2011;26(3):28–35. [Google Scholar]
- 46.Polanczyk G., de Lima M.S., Horta B.L., Biederman J., Rohde L.A. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatr. 2007 Jun;164(6):942–948. doi: 10.1176/ajp.2007.164.6.942. PMID: 17541055. [DOI] [PubMed] [Google Scholar]
- 47.Li J.Y., Li J., Liang J.H., Qian S., Jia R.X., Wang Y.Q., Xu Y. Depressive symptoms among children and adolescents in China: a systematic review and meta-analysis. Med Sci Mon Int Med J Exp Clin Res. 2019 Oct 5;25:7459–7470. doi: 10.12659/MSM.916774. PMID: 31586039; PMCID: PMC6792515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lopez A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C.J. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006 May 27;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 49.McCrone P., Knapp M., Fombonne E. The Maudsley long-term follow-up of child and adolescent depression. Predicting costs in adulthood. Eur Child Adolesc Psychiatr. 2005 Oct;14(7):407–413. doi: 10.1007/s00787-005-0491-6. [DOI] [PubMed] [Google Scholar]
- 50.Al-Adawi S. Adolescence in Oman. In: Jensen Arnett Jeffrey., editor. International encyclopedia of adolescence: a historical and cultural survey of young people around the world (2 volume set) Routledge; New York: 2006. pp. 713–728. [Google Scholar]
- 51.Eloul L., Ambusaidi A., Al-Adawi S. Silent epidemic of depression in women in the Middle East and North africa region: emerging tribulation or fallacy? Sultan Qaboos Univ Med J. 2009 Apr;9(1):5–15. Epub 2009 Mar 16. PMID: 21509269; PMCID: PMC3074757. [PMC free article] [PubMed] [Google Scholar]
- 52.Baxter A.J., Scott K.M., Vos T., Whiteford H.A. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med. 2013 May;43(5):897–910. doi: 10.1017/S003329171200147X. Epub 2012 Jul 10. PMID: 22781489. [DOI] [PubMed] [Google Scholar]
- 53.Melisse B., de Beurs E., van Furth E.F. Eating disorders in the Arab world: a literature review. J Eat Disord. 2020 Nov 6;8(1):59. doi: 10.1186/s40337-020-00336-x. PMID: 33292520; PMCID: PMC7646071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Al-Adawi S. Substance abuse in the Gulf cooperation Council states. In: Mamtani Ravinder, Albert B., Lowenfels M.D., editors. Critical issues in healthcare policy and politics in the Gulf cooperation Council states. Georgetown University Press; Washington: 2017. pp. 113–136. [Google Scholar]
- 55.Amin T.T., Amr M.A., Zaza B.O. Psychosocial predictors of smoking among secondary school students in Al-Hassa, Saudi Arabia. J Behav Med. 2011 Oct;34(5):339–350. doi: 10.1007/s10865-011-9319-7. Epub 2011 Feb 1. PMID: 21286799. [DOI] [PubMed] [Google Scholar]
- 56.Gaffar A.M., Alsanosy R.M., Mahfouz M.S. Sociodemographic factors associated with tobacco smoking among intermediate and secondary school students in Jazan Region of Saudi Arabia. Subst Abuse. 2013;34(4):381–388. doi: 10.1080/08897077.2013.779361. PMID: 24159909; PMCID: PMC3827661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jawad M., Lee J.T., Millett C. Waterpipe tobacco smoking prevalence and correlates in 25 eastern mediterranean and eastern European countries: cross-sectional analysis of the global youth tobacco survey. Nicotine Tob Res. 2016 Apr;18(4):395–402. doi: 10.1093/ntr/ntv101. Epub 2015 May 9. PMID: 25957438. [DOI] [PubMed] [Google Scholar]
- 58.Jawad M., Khader A., Millett C. Differences in tobacco smoking prevalence and frequency between adolescent Palestine refugee and non-refugee populations in Jordan, Lebanon, Syria, and the West Bank: cross-sectional analysis of the Global Youth Tobacco Survey. Conflict Health. 2016 Oct 5;10:20. doi: 10.1186/s13031-016-0087-4. PMID: 27708696; PMCID: PMC5050676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baška T., Warren C.W., Basková M., Jones N.R. Prevalence of youth cigarette smoking and selected social factors in 25 European countries: findings from the Global Youth Tobacco Survey. Int J Publ Health. 2009;54(6):439–445. doi: 10.1007/s00038-009-0051-9. PMID: 19680601. [DOI] [PubMed] [Google Scholar]
- 60.Lewis G., Williams P. Clinical judgement and the standardized interview in psychiatry. Psychol Med. 1989 Nov;19(4):971–979. doi: 10.1017/s0033291700005699. PMID: 2594892. [DOI] [PubMed] [Google Scholar]
- 61.van Hoeken D., Burns J.K., Hoek H.W. Epidemiology of eating disorders in Africa. Curr Opin Psychiatr. 2016 Nov;29(6):372–377. doi: 10.1097/YCO.0000000000000274. PMID: 27532943. [DOI] [PubMed] [Google Scholar]
- 62.Essien E.A., Okafor C.J., Okegbe J., Udofia O. Pattern and predictors of Brain Fag syndrome among senior secondary school students in Calabar, Nigeria. Niger Postgrad Med J. 2017 Jul-Sep;24(3):137–142. doi: 10.4103/npmj.npmj_49_17. PMID: 29082901. [DOI] [PubMed] [Google Scholar]
- 63.Thulin E.J., McLean K.E., Sevalie S., Akinsulure-Smith A.M., Betancourt T.S. Mental health problems among children in Sierra Leone: assessing cultural concepts of distress. Transcult Psychiatr. 2020 Apr 21 doi: 10.1177/1363461520916695. [DOI] [PubMed] [Google Scholar]
- 64.Salem H.A., Fahmy M.T., Youssef I.M., Haggag W.E., Muhamed A.G., Radwan D.N., Alkhadhari S. Attention deficit hyperactivity disorder in a referred sample of school-aged children in Kuwait: sociodemographics, frequency, clinical presentations and impairments. Egypt J Psychiatr. 2014;35(3):115. [Google Scholar]
- 65.Al-Haidar F.A. Co-morbidity and treatment of attention deficit hyperactivity disorder in Saudi Arabia. East Mediterr Health J. 2003 Sep-Nov;9(5–6):988–995. PMID: 16450529. [PubMed] [Google Scholar]
- 66.Al Hamed J.H., Taha A.Z., Sabra A.A., Bella H. Attention deficit hyperactivity disorder (ADHD) among male primary school children in Dammam, Saudi Arabia: prevalence and associated factors. J Egypt Publ Health Assoc. 2008;83(3–4):165–182. [PubMed] [Google Scholar]
- 67.Al-Gelban K.S. Depression, anxiety and stress among Saudi adolescent school boys. J R Soc Promot Health. 2007 Jan;127(1):33–37. doi: 10.1177/1466424007070492. PMID: 17319315. [DOI] [PubMed] [Google Scholar]
- 68.Al-Ghannami S.S., Al-Adawi S., Ghebremeskel K., Cramer M.T., Hussein I.S., Min Y., Jeyaseelan L., Al-Sibani N., Al-Shammakhi S.M., Al-Mamari F., Dorvlo A.S.S. Attention deficit hyperactivity disorder and parental factors in school children aged nine to ten years in Muscat, Oman. Oman Med J. 2018 May;33(3):193–199. doi: 10.5001/omj.2018.37. PMID: 29896326; PMCID: PMC5971059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Almuhlafi M., Jamilah K.A., Almutairi A.F., Salam M. Relationship between early menarche, obesity, and disordered eating behaviors: a school-based cross-sectional survey in Northern Saudi Arabia. Diabetes, Metab Syndrome Obes Targets Ther. 2018;11:743. doi: 10.2147/DMSO.S180697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fatima W., Ahmad L.M. Prevalence of disordered eating attitudes among adolescent girls in Arar City, Kingdom of Saudi Arabia. Health Psychol Res. 2018 Nov 29;6(1):7444. doi: 10.4081/hpr.2018.7444. PMID: 30596155; PMCID: PMC6280072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Homidi M., Obaidat Y., Hamaidi D. Prevalence of attention deficit and hyperactivity disorder among primary school students in Jeddah city, KSA. Life Sci J. 2013;10(3):280–285. [Google Scholar]
- 72.Jenahi E., Khalil M.S., Bella H. Prevalence of attention deficit hyperactivity symptoms in female schoolchildren in Saudi Arabia. Ann Saudi Med. 2012 Sep-Oct;32(5):462–468. doi: 10.5144/0256-4947.2012.462. PMID: 22871613; PMCID: PMC6080992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Alqahtani M.M. Attention-deficit hyperactive disorder in school-aged children in Saudi Arabia. Eur J Pediatr. 2010 Sep;169(9):1113–1117. doi: 10.1007/s00431-010-1190-y. Epub 2010 Mar 27. PMID: 20339867. [DOI] [PubMed] [Google Scholar]
- 74.Alqahtani M.M. The comorbidity of ADHD in the general population of Saudi Arabian school-age children. J Atten Disord. 2010 Jul;14(1):25–30. doi: 10.1177/1087054709347195. Epub 2009 Oct 22. PMID: 19850953. [DOI] [PubMed] [Google Scholar]
- 75.Alatiq Y., Alshalan M., Almodayfer O. Prevalence of psychiatric disorders among Saudi adolescent girls in a riyadh city high school. Arab J Psychiatr. 2017;44(5487):1–10. [Google Scholar]
- 76.Al-Modayfer O., Alatiq Y. A pilot study on the prevalence of psychiatric disorders among Saudi children and adolescents: a sample from a selected community in Riyadh city. Arab J Psychiatr. 2015;26(2):184–192. [Google Scholar]
- 77.Alharbi R., Alsuhaibani K., Almarshad A., Alyahya A. Depression and anxiety among high school student at Qassim Region. J Fam Med Prim Care. 2019 Feb;8(2):504–510. doi: 10.4103/jfmpc.jfmpc_383_18. PMID: 30984663; PMCID: PMC6436297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Allihaibi M.M. Disordered eating attitudes among secondary schoolgirls in Al-Iskan sector, Makkah Al-Mukarramah, Saudi Arabia. Int J Med Sci Publ Health. 2015 Jul 1;4(7):939–946. [Google Scholar]
- 79.Alenazi S.F., Hammad S.M., Mohamed A.E. Prevalence of depression, anxiety and stress among male secondary school students in Arar city, Saudi Arabia, during the school year 2018. Electron Physician. 2019;11(2):7522–7528. doi: 10.19082/752. [DOI] [Google Scholar]
- 80.Raheel H. Depression and associated factors among adolescent females in riyadh, kingdom of Saudi Arabia, A cross-sectional study. Int J Prev Med. 2015 Sep 9;6:90. doi: 10.4103/2008-7802.165156. PMID: 26445637; PMCID: PMC4593237. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This is a research article and all data generated or analyzed during this study are included in this published article.