Abstract
Epilepsy is one of the most common neurological disorders – estimated to affect at least 65 million worldwide. Most of the epilepsy research has so far focused on how to dampen neuronal discharges and to explain how changes in intrinsic neuronal activity or network function cause seizures. As a result, pharmacological therapy has largely been limited to symptomatic treatment targeted at neurons. Given the expanding spectrum of functions ascribed to the non-neuronal constituents of the brain, in both physiological brain function and in brain disorders, it is natural to closely consider the roles of astrocytes in epilepsy. It is now widely accepted that astrocytes are key controllers of the composition of the extracellular fluids, and may directly interact with neurons by releasing gliotransmitters. A central tenet is that astrocytic intracellular Ca2+ signals promote release of such signaling substances, either through synaptic or non-synaptic mechanisms. Accruing evidence suggests that astrocytic Ca2+ signals play important roles in both seizures and epilepsy, and this review aims to highlight the current knowledge of the roles of this central astrocytic signaling mechanism in ictogenesis and epileptogenesis.
Keywords: astrocyte, epilepsy, calcium signaling, IP3, epileptogenesis, ictogenesis, astrogliosis
Introduction
Epilepsy is one of the most common neurological disorders – estimated to affect around 1% of the world’s population (Hesdorffer et al., 2011; Neligan et al., 2012; Beghi, 2016). It is a chronic disorder, characterized by sudden, violent perturbations of normal brain function, causing social stigma, morbidity, and risk of premature death. In spite of a multitude of drugs for the treatment of epilepsy, about 30% of patients are not able to control their seizures with seizure suppressing medication (French, 2007; Perucca and Gilliam, 2012).
There is a striking lack of knowledge of the pathophysiological cellular mechanisms at play in epilepsy. For instance, the process transforming normal brain matter to a focus for epileptic seizures – the process of epileptogenesis – is not well understood. Also, the central question of what sets in motion an epileptic seizure – ictogenesis – remains unanswered. Most of the epilepsy research has so far focused on how to dampen neuronal discharges and to explain how changes in intrinsic neuronal activity or neuronal network function cause seizures. As a result, pharmacological therapy has been limited to symptomatic treatment aiming at neuronal targets. Given the expanding spectrum of roles ascribed to the non-neuronal constituents of the brain, it is natural to take a closer look at astrocytes as potential targets for epilepsy treatment.
Astrocytes are critical homeostatic controllers of extracellular glutamate and K+ levels (Rothstein et al., 1996; Larsen et al., 2014; Danbolt et al., 2016). Numerous studies have also demonstrated that astrocytes have important roles in supporting the neurons metabolically (Pellerin and Magistretti, 1994; Lundgaard et al., 2015) and that they have the capability of altering the vascular tone (Mulligan and MacVicar, 2004; Haydon and Carmignoto, 2006; Gordon et al., 2008). Increasing evidence suggests that astrocytes play important roles in brain state transitions and maintenance (Paukert et al., 2014; Poskanzer and Yuste, 2016; Szabó et al., 2017; Bojarskaite et al., 2020). Notably, astrocytes seem to also directly partake in brain signaling by releasing substances that affect neurons at the so-called tripartite synapse (Perea et al., 2009; Bindocci et al., 2017; Martin-Fernandez et al., 2017). A central tenet is that astroglial intracellular Ca2+ signals promote such “gliotransmitter” release, either through synaptic or non-synaptic mechanisms (Perea et al., 2014; Bazargani and Attwell, 2016). Glutamate, purines and D-serine are examples of transmitter substances that are thought to be released from astrocytes in a Ca2+ dependent manner (ibid.).
Perturbation of astrocytic Ca2+ signaling has been demonstrated in seizures and in epileptic tissue, potentially affecting both the homeostatic functions and signaling functions of astrocytes. These downstream mechanisms are largely speculative in the context of epilepsy but reflect the knowledge of roles of astrocytic Ca2+ signaling in physiology. Here, we discuss the relatively limited body of studies directly assessing astrocytic Ca2+ signaling in epilepsy, and briefly discuss potential downstream effects (Table 1). For the sake of structure and simplification, we arrange the topic into paragraphs on ictogenesis (i.e., the emergence of seizure activity), and epileptogenesis (i.e., the process by which the brain develops the predisposition of generating spontaneous seizures). These two processes are highly interconnected (Blauwblomme et al., 2014), but animal studies are often designed to study one of these two facets of epilepsy, and hence provide a framework for the further discussion.
TABLE 1.
Key publications investigating the roles of astrocytic Ca2 + signalling in ictogenesis and epileptogenesis.
| Publication | Model | Ca2+ indicator | Main findings |
|
Astrocytic Ca2+
signaling in ictogenesis | |||
| Kang et al., 2005 | Rat hippocampal slices, 4-AP | Fluo-4 AM | Adding IP3 in astrocytes causes epileptiform activity due to glutamate, and that astrocytic Ca2+ signals occur during 4-AP seizures |
| Tian et al., 2005 | Rat hippocampal slices: 4-AP, zero-Mg2+, bicuculline, penicillin Mouse cortex, in vivo, anesthetized: local injection of 4-AP | Fluo-4 AM | Increased astrocytic Ca2+ signaling in vivo during spread of 4-AP seizures, as well as showing that uncaging Ca2+ in astrocytes and extrasynaptic sources of glutamate triggered paroxysmal depolarization shifts |
| Fellin et al., 2006 | Mouse cortical-hippocampal slices: zero-Mg2+ and picrotoxin, or 0.5 mM Mg2+ and 8.5 mM K+ | Indo-1 AM or OGB-1 AM | A correlation between astrocytic Ca2+ and SICs, but activation of extrasynaptic NMDA activation by astrocytes is not necessary for either ictal or interictal epileptiform events |
| Ding et al., 2007 | Mouse, in vivo, anesthetized. Pilocarpine s.c., 350 mg/kg | Fluo-4 AM | Increase in astrocytic Ca2+ signals during SE. See also under “Epileptogenesis” |
| Gómez-Gonzalo et al., 2010 | Mouse entorhinal cortex slice: Picrotoxin/zero-Mg2+ Whole guinea pig: Bicuculline | OGB-1 AM / Rhod-2 | Astrocytic Ca2+ signals are triggered by ictal but not interictal events, and can be inhibited by blocking mGluRs and purinergic receptors. Astrocytic Ca2+ signals contribute to the excitation of neurons, and blocking of early ictal astrocytic Ca2+ signals prevent spread of ictal activity. |
| Baird-Daniel et al., 2017 | Rat cortex, in vivo, anesthetized. 4-AP. Blocking astrocytic Ca2+ signals and gap junctions with fluoroacetate and carbenoxolone, respectively | OGB-1 AM or Rhod-2 AM | Increased Ca2+ signals in astrocytes during seizures, but blocking of these did not affect epileptiform discharges or vascular dynamics associated with the seizures |
| Heuser et al., 2018 | Mouse hippocampus, in vivo, unanesthetized, “dual color” Ca2+ imaging of hippocampal neurons and astrocytes | GCaMP6f in astrocytes | Prominent astrocytic Ca2+ activity preceding local neuronal recruitment to seizure activity in hippocampus |
| Diaz Verdugo et al., 2019 | Zebra fish: PTZ | GCaMP6s in astrocytes | Large activations of astrocytic Ca2+ signals in the pre-ictal state and that astrocytic Ca2+ signals contribute to excitation of neurons |
| Zhang et al., 2019 | Mouse cortex, in vivo, anesthetized: local injection of 4-AP | OGB-1 AM | Absolute levels of Ca2+ in the astrocytic endfeet correlates with vascular tone during seizures |
| Astrocytic calcium signaling in epileptogenesis | |||
| Ding et al., 2007 | Mouse cortex, in vivo, anesthetized: Pilocarpine s.c. 350 mg/kg. 3D post SE | Fluo-4 AM | An increase in astrocytic Ca2+ signals at day 3 after SE due to mGluR5 signaling. Blocking this hyperactivity attenuated neuronal death |
| Szokol et al., 2015 | Mouse hippocampal slices: intracortical kainate injection. Early epileptogenesis (1, 3, and 7 days after SE) | GCaMP5E | Increased Ca2+ signaling in hippocampal astrocytes upon schaffer collateral stimulation at days 1 and 3 after SE mediated by mGluR |
| Umpierre et al., 2019 | Mouse hippocampal slices, at 1–3, 7–9, or 28–30 days after SE | GCaMP5G | mGluR5-mediated Ca2+ signaling re-emerges in epileptogenesis |
| Mentioned in Shigetomi et al. (2019): Sato et al.: unpublished report | 4 weeks after pilocarpine induced SE | Not known | Increased Ca2+ signaling in reactive astrocytes |
| Enger et al., 2015 conference proceedings, American Epilepsy Society conference | Mouse hippocampus, in vivo, unanesthetized. Chronic MTLE model of deep cortical kainate injection, imaging at 3 months after SE | GCaMP6f | Episodic spontaneous hyperactivity of reactive astrocytes within/close to the sclerotic hippocampus |
| Plata et al., 2018 | Rat, hippocampal slices, Lithium-pilocarpine | OGB-1 AM | A reduction in large size astrocytic Ca2+ events in atrophic astrocytes |
Astrocytic Ca2+ Signaling and Ictogenesis
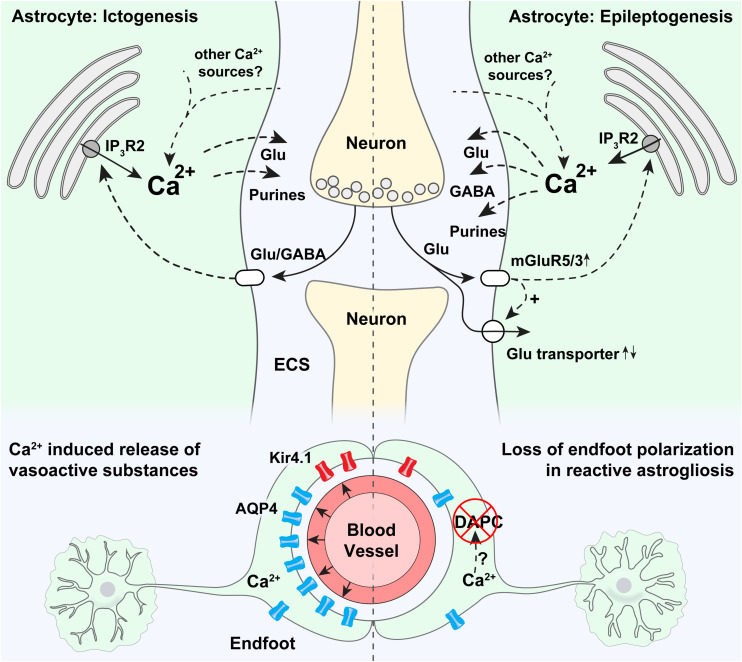
Ictogenesis describes the emergence of seizure activity (Blauwblomme et al., 2014). The interaction between astrocytes and neurons in ictogenesis has only sparsely been investigated and findings are to some extent ambiguous or contradictory, potentially due to different experimental models (Table 1; Tian et al., 2005; Fellin et al., 2006; Gómez-Gonzalo et al., 2010; Baird-Daniel et al., 2017; Heuser et al., 2018; Diaz Verdugo et al., 2019). Astrocytes express a plethora of functionally important receptors, transporters and channels, and a role of these cells in ictogenesis is highly suggestive (Agulhon et al., 2008; Patel et al., 2019; Caudal et al., 2020). Several known astrocyte-neuron interactions involving Ca2+ signaling can partake in ictogenesis or in the maintenance of hypersynchronous neuronal activity, possibly by creating excitatory feedback loops (Figure 1; Gómez-Gonzalo et al., 2010; Henneberger, 2017).
FIGURE 1.
Potential roles of astrocytic Ca2+ signaling in epilepsy. Strong astrocytic Ca2+ signals have been shown to occur in the emergency of acute seizures (in ictogenesis), that are probably triggered by neurotransmitters released by neurons. Ca2+ increases at the onset of seizures are known to be partly mediated by release through IP3R2 from the endoplasmic reticulum, even though pronounced Ca2+ signaling is present also in mice devoid of IP3R2. It is thought that intracellular Ca2+ increases may trigger proconvulsive gliotransmitter release. In astrocytic endfeet, increased Ca2+ signaling has been shown to correlate with ictal vasodilation. Epileptogenesis triggers a pronounced increase in mGluR5 expression, mGluR5-mediated Ca2+ signaling, and increased glutamate uptake. An increase in astrocytic Ca2+ signaling has been demonstrated in the days after status epilepticus, and aberrant Ca2+ signaling at later time points in the epileptogenesis has been anecdotally reported. Increased Ca2+ signaling could potentially cause both the release of glutamate (pro-convulsive), purines (pro-convulsive), and GABA (anti-convulsive, through Bestrophin-1 channels). In astrocytic endfeet in epileptic tissue a pronounced loss of aquaporin-4 (AQP4) and the K+ inwardly rectifying channel Kir4.1 can potentially be due to Ca2+ activated proteases causing a disassembly of the dystrophin associated protein complex (DAPC) tethering AQP4 and Kir4.1 to perivascular endfeet.
Building upon seminal studies demonstrating that astrocytes are able to directly interact with neurons (Nedergaard, 1994; Parpura et al., 1994; Araque et al., 1998; Parpura and Haydon, 2000; Parri et al., 2001; Angulo et al., 2004), Fellin et al. (2006), found that eliciting astrocytic Ca2+ signals by photolysis of caged Ca2 + and by application of ATP agonist and mGluR5 agonist triggered slow inward currents (SICs) in nearby neurons that were unaffected by application of the neuronal sodium channel blocker tetrodotoxin (Fellin et al., 2004). Soon thereafter, Tian et al. (2005) demonstrated that Ca2+ mediated glutamate release from astrocytes during experimentally induced seizure activity triggered slow inward currents (SICs) in neurons. These findings proposed a role for astrocytes in synchronizing neuronal activity and contributing to seizure generation (Tian et al., 2005). Further exploring which astrocytic Ca2+ signaling mechanisms were involved in this context, Kang et al. applied IP3 into astrocytes of the CA1 hippocampal region in rats, and were able to trigger epileptiform discharges in adjacent neurons (Kang et al., 2005). Later, Ding et al. (2007) were able to demonstrate increased astrocytic Ca2+ signaling in an in vivo pilocarpine epilepsy model. They proposed that this increase in Ca2+ signaling was due to activation of astrocytic metabotropic glutamate receptors, and that this activation led to the release of glutamate from astrocytes that could contribute to neuronal SICs through the activation of extrasynaptic neuronal NMDA receptors. By applying simultaneous patch-clamp recordings and Ca2+ imaging in cortical slices of the rat entorhinal cortex, Gómez-Gonzalo et al. (2010) found that Ca2+ elevations in astrocytes correlate with initiation and maintenance of focal seizure-like discharges, and postulated a recurrent excitatory loop between neurons and astrocytes in ictogenesis, where astrocytes play a role in recruiting neurons to ictal events, possibly through the release of gliotransmitters (Gómez-Gonzalo et al., 2010).
By using two-photon microscopy and simultaneous astrocyte and neuron Ca2+ imaging in the hippocampal CA1 region of awake mice, we were able to show that prominent astrocytic Ca2+ transients preceded local hypersynchronous neuronal activity in the emergence of kainate induced generalized epileptic seizures (Heuser et al., 2018). These findings were in agreement with the earlier results from the study of Tian et al. (2005), who also observed stereotypical astrocytic Ca2+ signals typically preceding local neurons in the spread of cortical seizure activity. A later work by Diaz Verdugo et al. (2019) similarly demonstrated large and synchronized astrocytic Ca2+ signals preceding ictal onset in zebrafish, and proposed that this signaling modulated neural excitation through glutamate release, by gap junction dependent mechanisms. In another in vivo study, Zhang et al. (2019), provided evidence, although correlative, that increased Ca2+ concentration in astrocytic endfeet governed precapillary arteriole dilation during epileptic events, suggesting a role for astrocytes in the metabolic support of neurons in seizures. In contrast to these previously mentioned studies, data from another model for focal neocortical seizures in anesthetized rats using bulk-loaded synthetic Ca2+ indicators found the astrocytic Ca2+ activation to lag behind neuronal activation and to be unnecessary for ictogenesis and the accompanying vascular dynamics (Baird-Daniel et al., 2017).
An extensive array of stimuli and corresponding signaling pathways have been shown to trigger intracellular Ca2+ signals in astrocytes (Zhang et al., 2019; Caudal et al., 2020). To discuss all of them would go beyond the scope of this review. One important pathway is mediated by the Inositol 1,4,5-trisphosphate (IP3) receptor in the endoplasmic reticulum, of which the isoform 2 (IP3R2) is thought to be the key functional IP3 receptor in astrocytes (Figure 1; Sharp et al., 1999; Parri and Crunelli, 2003; Volterra and Steinhäuser, 2004; Scemes and Giaume, 2006; Foskett et al., 2007). Lack of IP3R2 has been shown to abolish a large proportion of astrocytic Ca2+ signals (Petravicz et al., 2008; Guerra-Gomes et al., 2020). In spite of the importance of IP3 as a second messenger involved in astrocytic Ca2+ dynamics, mice lacking this receptor are overtly normal (Petravicz et al., 2008). Accordingly, studies have questioned the physiological importance of IP3-mediated astrocytic Ca2+ signaling, by for instance demonstrating normal synaptic transmission and plasticity in mice devoid of IP3R2 (Agulhon et al., 2010; Nizar et al., 2013; Petravicz et al., 2014). Conversely, we have demonstrated attenuated seizure activity in mice devoid of IP3R2 compared to WT mice following low dose intraperitoneal kainate, suggesting a proconvulsant role of astrocytic IP3R2 mediated Ca2+ elevations (Heuser et al., 2018). However, seizure activity in this study was only collected for 1 h after initiation of seizures, encouraging further investigation of the role of IP3R2 at later time points during epileptogenesis and in chronic epilepsy. Interestingly, even though a sizable amount of Ca2+ signals were still present in the knockout mice, we found that the early activation of astrocytic Ca2+ signals in the emergence of seizures, as discussed above, was dependent on IP3R2 (Heuser et al., 2018). These two observations underscore the potential importance of IP3R2 in ictogenesis.
Another pathway involved in astrocytic Ca2+ signaling attracting increasing attention for a role in epilepsy is glial purinergic signaling (Ding et al., 2007; Wellmann et al., 2018; Alves et al., 2019; Nikolic et al., 2020). Activation of astrocytic purinergic receptors triggers intracellular Ca2+ signals that could promote astrocytic release of gliotransmitters like glutamate or ATP, which acts on neurons and modulates excitation [reviewed in Nikolic et al. (2020)]. Importantly, Nikolic et al. (2018) provided evidence for TNFα-driven autocrine astrocyte purinergic signaling as a trigger of glutamatergic gliotransmission in a model of mesial temporal lobe epilepsy (mTLE), highlighting the complex interplay between astrocytes and microglia in epilepsy pathogenesis, discussed elsewhere (Bedner and Steinhäuser, 2019).
Most of the studies above explored the role for astrocytic Ca2+ signals in seizures in relation to gliotransmission, i.e., that astrocytes release transmitters that directly signal to neurons. A growing body of evidence suggests that astrocytic Ca2+ signals also play important roles in the control of the homeostatic functions of astrocytes. For instance they have been shown to be involved in the uptake of extracellular K+ through modulation of the Na+/K+ ATPase, and through the breakdown of glycogen (Wang et al., 2012; Müller et al., 2014). These mechanisms remain poorly explored in the context of epilepsy but could be important downstream effects of astrocytic Ca2+ signaling.
Astrocytic Ca2+ Signaling and Epileptogenesis
Epileptogenesis refers to the gradual process by which a normal brain develops a propensity for recurrent seizure activity. A range of pathophysiological changes have been shown to occur during epileptogenesis, including inflammation, neurodegeneration, aberrant neurogenesis and dendritic plasticity, impaired blood-brain-barrier, epigenetic changes and alterations of the molecular composition and function of ion channels, receptors and transporters, and more (van Vliet et al., 2007; Vezzani et al., 2011; Steinhäuser and Seifert, 2012; Dingledine et al., 2014; Jessberger and Parent, 2015; Hauser et al., 2018; Escartin et al., 2021).
A common denominator of astrocytic pathophysiology associated with epileptogenesis is the process of reactive astrogliosis (Burda and Sofroniew, 2014; Pekny and Pekna, 2016). This is a graded response to a wide array of insults, which is a hallmark of many neurological disorders (Burda and Sofroniew, 2014; Ferlazzo et al., 2016; Glushakov et al., 2016; Pekny and Pekna, 2016; Fordington and Manford, 2020; Galovic et al., 2021).
Reactive astrocytes are characterized by morphological and molecular changes (Figure 1). Specifically they proliferate, undergo hypertrophy and increase their expression of intermediary filament proteins like glial fibrillary acid protein (GFAP) and vimentin (Yang et al., 1994; Pekny and Nilsson, 2005; Sofroniew, 2009; Cregg et al., 2014; Escartin et al., 2021). In extremis, these changes may lead to the formation of a glial scar (Miller, 2005; Barres, 2008; Sofroniew, 2009; Burda and Sofroniew, 2014; Ferlazzo et al., 2016; Glushakov et al., 2016; Pekny and Pekna, 2016; Fordington and Manford, 2020; Galovic et al., 2021). Reactive astrogliosis can be observed in several acquired forms of epilepsy but has mostly been investigated in the context of mTLE (Wieser and ILAE Commission on Neurosurgery of Epilepsy., 2004; Blümcke et al., 2013; Cendes et al., 2014).
There is ample evidence that reactive astrocytes display aberrant Ca2+ signaling at least in the early phase of epileptogenesis (Table 1). Ding et al. (2007) found increased astrocytic Ca2+ activity in the days following pilocarpine-induced SE in mice. In the same study both in vitro and in vivo pharmacological approaches demonstrated that these Ca2+ signals could contribute to neuronal death, linking astrocytic hyperactivity to a key hallmark of epileptogenesis (Ding et al., 2007). We confirmed the astrocytic hyperactivity following SE by employing genetically encoded Ca2+ indicators in acute hippocampal slices from a mouse model of mTLE, and found that stimulation-evoked Ca2+ transients in astrocytic endfeet even outlasted those in cell bodies during the latent phase of epileptogenesis (Szokol et al., 2015).
Increased astrocytic Ca2+ activity has been anecdotally reported at even later time points after the initial insult (Enger et al., 2015; Shigetomi et al., 2019). These increased Ca2+ signals are likely stimuli- and stage specific and may reflect the degree of the reactive astrogliosis (Kuchibhotla et al., 2009; Fordsmann et al., 2019), as others have shown attenuated astrocytic Ca2+ activity in atrophic astrocytes in chronic epilepsy (Plata et al., 2018).
The degree, development and underlying mechanisms involved in aberrant Ca2+ signaling in epileptogenesis are still unknown, but it is plausible that several of the physiological signaling pathways involved in astrocytic Ca2+ dynamics (Caudal et al., 2020), could be perturbed. A major pathway for eliciting astrocytic Ca2+ signals is the activation of the Gq G-protein coupled receptors (GqPCRs) and subsequent release of Ca2+ from the endoplasmic reticulum via IP3R2 as discussed in “Astrocyte Ca2 + signaling and Ictogenesis” (Figure 1; Foskett et al., 2007). Astrocytes express several GqPCRs, of which mGluR5 has attracted most attention due to an upregulation in epileptic tissue and potential involvement in an excitatory loop comprising glutamate induced Ca2+ dependent glutamate release from astrocytes (Umpierre et al., 2019). While astrocytes in the adult brain are almost depleted of mGluR5 (Sun et al., 2013), the receptor is consistently expressed in chronic epilepsy models and resected tissue from patients with epilepsy (Aronica et al., 2000, 2003), and a recent study has shown that mGluR5 expression and mGluR5-dependent Ca2+ transients reemerge during epileptogenesis along with an increase in glutamate uptake (Umpierre et al., 2019). This reemergence of astrocytic mGluR5 could potentially be a compensatory anti-epileptic mechanism to handle the elevated glutamate levels in epileptic tissue but could possibly also represent a pro-epileptic feature triggering downstream Ca2+ mediated gliotransmission.
Apart from these perturbations in glutamate dynamics, it has been shown that reactive astrocytes exhibit a tonic release of GABA, presumably through Bestrophin-1 channels (Pandit et al., 2020). Bestrophin-1 channels are Ca2+ activated anion channels, and increased GABA release could hence be a downstream effect of increased Ca2+ signaling in reactive astrocytes (Lee et al., 2010). In support of this conjecture is the finding of an accumulation of GABA in reactive astrocytes in a model of mTLE (Müller et al., 2020). Potentially, this is a protective aspect of reactive astrocytes to curb epileptiform activity in this pathological tissue.
Moreover, as mentioned in “Ictogenesis” astrocytic Ca2+ signaling has been suggested to be involved in homeostatic mechanisms of astrocytes. These mechanisms could be important downstream effects of astrocytic Ca2+ dyshomeostasis in epileptic tissue, but these effects are so far rudimentarily investigated in epilepsy.
Loss of astrocytic gap junction coupling has been shown to occur during early epileptogenesis in experimental models of mTLE and in specimens of resected hippocampi from patients with mTLE (Bedner et al., 2015; Deshpande et al., 2017, 2020; Henning et al., 2021). It is believed that this loss of astrocytic coupling in epilepsy may perturb the ability of astrocytes to remove K+ from the extracellular space through the process of K+ spatial buffering (Nwaobi et al., 2016). Notably, astrocytic gap junctions may also allow Ca2+ signals to propagate from cell to cell, at least during pathological conditions like seizure activity (Scemes and Giaume, 2006). It is tempting to hypothesize that such propagating Ca2+ waves could play a role in neuronal synchronization and seizure generation. Potentially a loss of astrocytic gap junctions as seen in epileptic tissue, may be a compensatory mechanism to prevent intercellular spread of astrocytic Ca2+ waves. Even so, to the best of our knowledge, no direct study of astrocytic Ca2+ signaling in gap junction deficient mice has been performed.
Loss of the highly concentrated expression of key membrane channels in astrocytic endfoot processes, i.e., loss of astrocyte polarization, is another pathological hallmark, which could be a consequence of perturbed glial Ca2+ dynamics (Figure 1). For instance AQP4 and Kir4.1 are normally densely expressed in astrocytic endfeet, kept in place by the so-called dystrophin associated protein complex (DAPC) (Nagelhus et al., 1998; Enger et al., 2012), and in tissue resectates from patients with mTLE, a striking loss of this polarized expression of both AQP4 and Kir4.1 have been shown (Eid et al., 2005; Heuser et al., 2012). It is possible that prolonged epileptic activity and increased Ca2+ signaling in astrocytic endfeet, as we demonstrated in Szokol et al. (2015), activate Ca2+ dependent proteases like calpain (Nagelhus and Ottersen, 2013), that shows affinity to dystrophin and could cleave the DAPC (Figure 1; Shields et al., 2000).
Even though the evidence is indirect, it has been suggested that this loss of astrocyte endfoot polarization could contribute to epileptogenesis and hyperexcitation (Binder et al., 2012; Binder and Carson, 2013; Crunelli et al., 2015). Notably, the loss of the astrocyte endfoot Kir4.1 channels in tissue from mTLE patients (Heuser et al., 2012) is expected to cause impaired K+ handling and resultant neuronal hyperexcitation due to the role of Kir4.1 in K+ homeostasis (Bordey and Sontheimer, 1998; Hinterkeuser et al., 2000; Kivi et al., 2000; Neusch et al., 2001; Djukic et al., 2007; Bockenhauer et al., 2009; Scholl et al., 2009; Steinhäuser et al., 2012).
Conclusion and Future Perspectives
Here we have discussed the role of astrocyte Ca2+ signaling in ictogenesis and epileptogenesis. These terms are used to describe two different features of epilepsy, but do not necessarily imply two separate processes, as mechanisms crucial in ictogenesis could also be an integral part of epileptogenesis, or vice versa. While we often associate astrocytic dysfunction in epileptogenesis with the appearance of reactive astrogliosis (Escartin et al., 2021), the term ictogenesis seems typically to be used when studying the interplay between neurons and astrocytes independent of pre-existing tissue pathology. Therefore, we may overlook the fact that ictogenesis most often would occur in tissue that has undergone pathological transformation typical for epileptogenesis, i.e., not normal, healthy tissue. On the other hand, epileptogenesis comprises many pathological changes beyond reactive astrogliosis, like alterations in transcriptional regulation, morphological, biochemical, metabolic and physiological remodeling ultimately resulting in gain or loss of function (Escartin et al., 2021).
Astrocytic Ca2+ signals are today considered a main readout of astrocytic activity and there are reasons to believe that they play important roles in epilepsy. Evidence suggests that such signals are neither necessary nor sufficient to maintain epileptiform activity, but rather should be seen as modulators of the pathophysiological process. The literature directly investigating the role of astrocytic Ca2+ signaling in epilepsy is still sparse and at some points contradictory, and for most proposed mechanisms only a small subset of the signaling pathways involved are identified. A major challenge will be to disentangle the potentially beneficial from detrimental consequences of the different modes of astrocyte Ca2+ signaling in reactive astrogliosis. It is even probable that astrocyte Ca2+ signaling may carry different roles in the large variety of epileptic entities. To decipher the roles of astrocyte Ca2+ signaling in epilepsy, next steps should include a rigorous study of the mechanisms mentioned above in vivo in adult mice, leveraging new developments in both imaging and genetics, with the aim of identifying promising targets for future pharmacological therapy of epilepsy.
Author Contributions
KH and RE reviewed the literature, conceptualized the manuscript, and wrote the manuscript. Both authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank the Department of Neurology, Oslo University Hospital, and especially Erik Taubøll, leader of the Epilepsy Research Group, Oslo, https://www.ous-research.no/ergo/, for constant support. We would also like to thank all members of the EU Glia Ph.D. Consortium, http://www.eu-gliaphd.eu for long-lasting friendship and discussions on glial pathology in epilepsy, and the Letten Foundation.
Footnotes
Funding. KH has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement no. 722053.
References
- Agulhon C., Fiacco T. A., McCarthy K. D. (2010). Hippocampal short- and long-term plasticity are not modulated by astrocyte Ca2 signaling. Science 327 1250–1254. 10.1126/science.1184821 [DOI] [PubMed] [Google Scholar]
- Agulhon C., Petravicz J., McMullen A. B., Sweger E. J., Minton S. K., Taves S. R., et al. (2008). What is the role of astrocyte calcium in neurophysiology? Neuron 59 932–946. 10.1016/j.neuron.2008.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves M., De Diego Garcia L., Conte G., Jimenez-Mateos E. M., D’Orsi B., Sanz-Rodriguez A., et al. (2019). Context-specific switch from anti- to pro-epileptogenic function of the P2Y receptor in experimental epilepsy. J. Neurosci. 39 5377–5392. 10.1523/jneurosci.0089-19.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angulo M. C., Kozlov A. S., Charpak S., Audinat E. (2004). Glutamate released from glial cells synchronizes neuronal activity in the hippocampus. J. Neurosci. 24 6920–6927. 10.1523/jneurosci.0473-04.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araque A., Sanzgiri R. P., Parpura V., Haydon P. G. (1998). Calcium elevation in astrocytes causes an NMDA receptor-dependent increase in the frequency of miniature synaptic currents in cultured hippocampal neurons. J. Neurosci. 18 6822–6829. 10.1523/jneurosci.18-17-06822.1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronica E., Gorter J. A., Jansen G. H., van Veelen C. W. M., van Rijen P. C., Ramkema M., et al. (2003). Expression and cell distribution of group I and group II metabotropic glutamate receptor subtypes in taylor-type focal cortical dysplasia. Epilepsia 44 785–795. 10.1046/j.1528-1157.2003.54802.x [DOI] [PubMed] [Google Scholar]
- Aronica E., van Vliet E. A., Mayboroda O. A., Troost D., da Silva F. H., Gorter J. A. (2000). Upregulation of metabotropic glutamate receptor subtype mGluR3 and mGluR5 in reactive astrocytes in a rat model of mesial temporal lobe epilepsy. Eur. J. Neurosci. 12 2333–2344. 10.1046/j.1460-9568.2000.00131.x [DOI] [PubMed] [Google Scholar]
- Baird-Daniel E., Daniel A. G. S., Wenzel M., Li D., Liou J.-Y., Laffont P., et al. (2017). Glial calcium waves are triggered by seizure activity and not essential for initiating ictal onset or neurovascular coupling. Cereb. Cortex 27 3318–3330. 10.1093/cercor/bhx072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barres B. A. (2008). The mystery and magic of glia: a perspective on their roles in health and disease. Neuron 60 430–440. 10.1016/j.neuron.2008.10.013 [DOI] [PubMed] [Google Scholar]
- Bazargani N., Attwell D. (2016). Astrocyte calcium signaling: the third wave. Nat. Neurosci. 19 182–189. 10.1038/nn.4201 [DOI] [PubMed] [Google Scholar]
- Bedner P., Dupper A., Hüttmann K., Müller J., Herde M. K., Dublin P., et al. (2015). Astrocyte uncoupling as a cause of human temporal lobe epilepsy. Brain 138 1208–1222. 10.1093/brain/awv067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedner P., Steinhäuser C. (2019). TNFα-driven astrocyte purinergic signaling during epileptogenesis. Trends Mol. Med. 25 70–72. 10.1016/j.molmed.2018.12.001 [DOI] [PubMed] [Google Scholar]
- Beghi E. (2016). Addressing the burden of epilepsy: many unmet needs. Pharmacol. Res. 107 79–84. 10.1016/j.phrs.2016.03.003 [DOI] [PubMed] [Google Scholar]
- Binder D. K., Carson M. J. (2013). Glial cells as primary therapeutic targets for epilepsy. Neurochem. Int. 63 635–637. 10.1016/j.neuint.2013.09.004 [DOI] [PubMed] [Google Scholar]
- Binder D. K., Nagelhus E. A., Ottersen O. P. (2012). Aquaporin-4 and epilepsy. Glia 60 1203–1214. 10.1002/glia.22317 [DOI] [PubMed] [Google Scholar]
- Bindocci E., Savtchouk I., Liaudet N., Becker D., Carriero G., Volterra A. (2017). Three-dimensional Ca imaging advances understanding of astrocyte biology. Science 356:eaai8185. 10.1126/science.aai8185 [DOI] [PubMed] [Google Scholar]
- Blauwblomme T., Jiruska P., Huberfeld G. (2014). Mechanisms of ictogenesis. Int. Rev. Neurobiol. 114 155–185. 10.1016/b978-0-12-418693-4.00007-8 [DOI] [PubMed] [Google Scholar]
- Blümcke I., Thom M., Aronica E., Armstrong D. D., Bartolomei F., Bernasconi A., et al. (2013). International consensus classification of hippocampal sclerosis in temporal lobe epilepsy: a Task Force report from the ILAE commission on diagnostic methods. Epilepsia 54 1315–1329. 10.1111/epi.12220 [DOI] [PubMed] [Google Scholar]
- Bockenhauer D., Feather S., Stanescu H. C., Bandulik S., Zdebik A. A., Reichold M., et al. (2009). Epilepsy, ataxia, sensorineural deafness, tubulopathy, and KCNJ10 mutations. N. Engl. J. Med. 360 1960–1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojarskaite L., Bjørnstad D. M., Pettersen K. H., Cunen C., Hermansen G. H., Åbjørsbråten K. S., et al. (2020). Astrocytic Ca signaling is reduced during sleep and is involved in the regulation of slow wave sleep. Nat. Commun. 11:3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bordey A., Sontheimer H. (1998). Properties of human glial cells associated with epileptic seizure foci. Epilepsy Res. 32 286–303. 10.1016/s0920-1211(98)00059-x [DOI] [PubMed] [Google Scholar]
- Burda J. E., Sofroniew M. V. (2014). Reactive gliosis and the multicellular response to CNS damage and disease. Neuron 81 229–248. 10.1016/j.neuron.2013.12.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caudal L. C., Gobbo D., Scheller A., Kirchhoff F. (2020). The paradox of astroglial Ca2+ signals at the interface of excitation and inhibition. Front. Cell. Neurosci. 14:609947. 10.3389/fncel.2020.609947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cendes F., Sakamoto A. C., Spreafico R., Bingaman W., Becker A. J. (2014). Epilepsies associated with hippocampal sclerosis. Acta Neuropathol. 128 21–37. 10.1007/s00401-014-1292-0 [DOI] [PubMed] [Google Scholar]
- Cregg J. M., DePaul M. A., Filous A. R., Lang B. T., Tran A., Silver J. (2014). Functional regeneration beyond the glial scar. Exp. Neurol. 253 197–207. 10.1016/j.expneurol.2013.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crunelli V., Carmignoto G., Steinhäuser C. (2015). Novel astrocyte targets: new avenues for the therapeutic treatment of epilepsy. Neuroscientist 21 62–83. 10.1177/1073858414523320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danbolt N. C., Furness D. N., Zhou Y. (2016). Neuronal vs glial glutamate uptake: resolving the conundrum. Neurochem. Int. 98 29–45. 10.1016/j.neuint.2016.05.009 [DOI] [PubMed] [Google Scholar]
- Deshpande T., Li T., Henning L., Wu Z., Müller J., Seifert G., et al. (2020). Constitutive deletion of astrocytic connexins aggravates kainate−induced epilepsy. Glia 68 2136–2147. 10.1002/glia.23832 [DOI] [PubMed] [Google Scholar]
- Deshpande T., Li T., Herde M. K., Becker A., Vatter H., Schwarz M. K., et al. (2017). Subcellular reorganization and altered phosphorylation of the astrocytic gap junction protein connexin43 in human and experimental temporal lobe epilepsy. Glia 65 1809–1820. 10.1002/glia.23196 [DOI] [PubMed] [Google Scholar]
- Diaz Verdugo C., Myren-Svelstad S., Aydin E., Van Hoeymissen E., Deneubourg C., Vanderhaeghe S., et al. (2019). Glia-neuron interactions underlie state transitions to generalized seizures. Nat. Commun. 10: 3830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding S., Fellin T., Zhu Y., Lee S.-Y., Auberson Y. P., Meaney D. F., et al. (2007). Enhanced astrocytic Ca2+ signals contribute to neuronal excitotoxicity after status epilepticus. J. Neurosci. 27 10674–10684. 10.1523/jneurosci.2001-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingledine R., Varvel N. H., Dudek F. E. (2014). When and how do seizures kill neurons, and is cell death relevant to epileptogenesis? Adv. Exp. Med. Biol. 813 109–122. 10.1007/978-94-017-8914-1_9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djukic B., Casper K. B., Philpot B. D., Chin L.-S., McCarthy K. D. (2007). Conditional knock-out of Kir4.1 leads to glial membrane depolarization, inhibition of potassium and glutamate uptake, and enhanced short-term synaptic potentiation. J. Neurosci. 27 11354–11365. 10.1523/jneurosci.0723-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eid T., Lee T.-S. W., Thomas M. J., Amiry-Moghaddam M., Bjornsen L. P., Spencer D. D., et al. (2005). Loss of perivascular aquaporin 4 may underlie deficient water and K homeostasis in the human epileptogenic hippocampus. Proc. Natl. Acad. Sci. U.S.A. 102 1193–1198. 10.1073/pnas.0409308102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enger R., Gundersen G. A., Haj-Yasein N. N., Eilert-Olsen M., Thoren A. E., Vindedal G. F., et al. (2012). Molecular scaffolds underpinning macroglial polarization: an analysis of retinal Müller cells and brain astrocytes in mouse. Glia 60 2018–2026. 10.1002/glia.22416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enger R., Heuser K., Nome C., Tang W., Jensen V., Helm P. J., et al. (2015). “Abnormal astrocytic Ca2+ signaling in the sclerotic hippocampus of awake mice: a two-photon imaging study using the unilateral intracortical kainate injection model of mesial temporal lobe epilepsy,” in Proceedings of the AES 2015 Annual Meeting Abstract Database, (Chicago: American epilepsy society; ). [Google Scholar]
- Escartin C., Galea E., Lakatos A., O’Callaghan J. P., Petzold G. C., Serrano-Pozo A., et al. (2021). Reactive astrocyte nomenclature, definitions, and future directions. Nat. Neurosci. 24 312–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellin T., Gomez-Gonzalo M., Gobbo S., Carmignoto G., Haydon P. G. (2006). Astrocytic glutamate is not necessary for the generation of epileptiform neuronal activity in hippocampal slices. J. Neurosci. 26 9312–9322. 10.1523/jneurosci.2836-06.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellin T., Pascual O., Gobbo S., Pozzan T., Haydon P. G., Carmignoto G. (2004). Neuronal synchrony mediated by astrocytic glutamate through activation of extrasynaptic NMDA receptors. Neuron 43 729–743. 10.1016/j.neuron.2004.08.011 [DOI] [PubMed] [Google Scholar]
- Ferlazzo E., Gasparini S., Beghi E., Sueri C., Russo E., Leo A., et al. (2016). Epilepsy in cerebrovascular diseases: review of experimental and clinical data with meta-analysis of risk factors. Epilepsia 57 1205–1214. 10.1111/epi.13448 [DOI] [PubMed] [Google Scholar]
- Fordington S., Manford M. (2020). A review of seizures and epilepsy following traumatic brain injury. J. Neurol. 267 3105–3111. 10.1007/s00415-020-09926-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fordsmann J. C., Murmu R. P., Cai C., Brazhe A., Thomsen K. J., Zambach S. A., et al. (2019). Spontaneous astrocytic Ca activity abounds in electrically suppressed ischemic penumbra of aged mice. Glia 67 37–52. 10.1002/glia.23506 [DOI] [PubMed] [Google Scholar]
- Foskett J. K., White C., Cheung K.-H., Mak D.-O. D. (2007). Inositol trisphosphate receptor Ca2+ release channels. Physiol. Rev. 87 593–658. 10.1152/physrev.00035.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- French J. A. (2007). Refractory epilepsy: clinical overview. Epilepsia 48(Suppl. 1), 3–7. 10.1111/j.1528-1167.2007.00992.x [DOI] [PubMed] [Google Scholar]
- Galovic M., Ferreira-Atuesta C., Abraira L., Döhler N., Sinka L., Brigo F., et al. (2021). Seizures and epilepsy after stroke: epidemiology, biomarkers and management. Drugs Aging. 38 285–299. 10.1007/s40266-021-00837-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glushakov A. V., Glushakova O. Y., Doré S., Carney P. R., Hayes R. L. (2016). Animal Models of Posttraumatic Seizures and Epilepsy. Methods Mol. Biol. 1462 481–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Gonzalo M., Losi G., Chiavegato A., Zonta M., Cammarota M., Brondi M., et al. (2010). An excitatory loop with astrocytes contributes to drive neurons to seizure threshold. PLoS Biol. 8:e1000352. 10.1371/journal.pbio.1000352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon G. R. J., Choi H. B., Rungta R. L., Ellis-Davies G. C. R., MacVicar B. A. (2008). Brain metabolism dictates the polarity of astrocyte control over arterioles. Nature 456 745–749. 10.1038/nature07525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra-Gomes S., Cunha-Garcia D., Marques Nascimento D. S., Duarte-Silva S., Loureiro-Campos E., Morais Sardinha V., et al. (2020). IP R2 null mice display a normal acquisition of somatic and neurological development milestones. Eur. J. Neurosci. 10.1111/ejn.14724 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Hauser R. M., Henshall D. C., Lubin F. D. (2018). The Epigenetics of Epilepsy and Its Progression. Neuroscientist 24 186–200. 10.1177/1073858417705840 [DOI] [PubMed] [Google Scholar]
- Haydon P. G., Carmignoto G. (2006). Astrocyte control of synaptic transmission and neurovascular coupling. Physiol. Rev. 86 1009–1031. 10.1152/physrev.00049.2005 [DOI] [PubMed] [Google Scholar]
- Henneberger C. (2017). Does rapid and physiological astrocyte-neuron signalling amplify epileptic activity? J. Physiol. 595 1917–1927. 10.1113/jp271958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henning L., Steinhäuser C., Bedner P. (2021). Initiation of experimental temporal lobe epilepsy by early astrocyte uncoupling is independent of TGFβR1/ALK5 signaling. Front. Neurol. 12:660591. 10.3389/fneur.2021.660591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesdorffer D. C., Logroscino G., Benn E. K. T., Katri N., Cascino G., Hauser W. A. (2011). Estimating risk for developing epilepsy: a population-based study in Rochester, Minnesota. Neurology 76 23–27. 10.1212/wnl.0b013e318204a36a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuser K., Eid T., Lauritzen F., Thoren A. E., Vindedal G. F., Taubøll E., et al. (2012). Loss of perivascular Kir4.1 potassium channels in the sclerotic hippocampus of patients with mesial temporal lobe epilepsy. J. Neuropathol. Exp. Neurol. 71 814–825. 10.1097/nen.0b013e318267b5af [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuser K., Nome C. G., Pettersen K. H., Åbjørsbråten K. S., Jensen V., Tang W., et al. (2018). Ca2+ Signals in astrocytes facilitate spread of epileptiform activity. Cereb. Cortex 28 4036–4048. 10.1093/cercor/bhy196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinterkeuser S., Schröder W., Hager G., Seifert G., Blümcke I., Elger C. E., et al. (2000). Astrocytes in the hippocampus of patients with temporal lobe epilepsy display changes in potassium conductances. Eur. J. Neurosci. 12 2087–2096. 10.1046/j.1460-9568.2000.00104.x [DOI] [PubMed] [Google Scholar]
- Jessberger S., Parent J. M. (2015). Epilepsy and adult neurogenesis. Cold Spring Harb. Perspect. Biol. 7:a020677. 10.1101/cshperspect.a020677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang N., Xu J., Xu Q., Nedergaard M., Kang J. (2005). Astrocytic glutamate release-induced transient depolarization and epileptiform discharges in hippocampal CA1 pyramidal neurons. J. Neurophysiol. 94 4121–4130. 10.1152/jn.00448.2005 [DOI] [PubMed] [Google Scholar]
- Kivi A., Lehmann T.-N., Kovács R., Eilers A., Jauch R., Meencke H. J., et al. (2000). Effects of barium on stimulus-induced rises of [K]oin human epileptic non-sclerotic and sclerotic hippocampal area CA1. Eur. J. Neurosci. 12 2039–2048. 10.1046/j.1460-9568.2000.00103.x [DOI] [PubMed] [Google Scholar]
- Kuchibhotla K. V., Lattarulo C. R., Hyman B. T., Bacskai B. J. (2009). Synchronous hyperactivity and intercellular calcium waves in astrocytes in Alzheimer mice. Science 323 1211–1215. 10.1126/science.1169096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen B. R., Assentoft M., Cotrina M. L., Hua S. Z., Nedergaard M., Kaila K., et al. (2014). Contributions of the Na+/K+-ATPase, NKCC1, and Kir4.1 to hippocampal K+ clearance and volume responses. Glia 62 608–622. 10.1002/glia.22629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Yoon B.-E., Berglund K., Oh S.-J., Park H., Shin H.-S., et al. (2010). Channel-mediated tonic GABA release from glia. Science 330 790–796. 10.1126/science.1184334 [DOI] [PubMed] [Google Scholar]
- Lundgaard I., Li B., Xie L., Kang H., Sanggaard S., Haswell J. D. R., et al. (2015). Direct neuronal glucose uptake heralds activity-dependent increases in cerebral metabolism. Nat. Commun. 6:6807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin-Fernandez M., Jamison S., Robin L. M., Zhao Z., Martin E. D., Aguilar J., et al. (2017). Synapse-specific astrocyte gating of amygdala-related behavior. Nat. Neurosci. 20 1540–1548. 10.1038/nn.4649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller G. (2005). Neuroscience. The dark side of glia. Science 308 778–781. 10.1126/science.308.5723.778 [DOI] [PubMed] [Google Scholar]
- Müller J., Timmermann A., Henning L., Müller H., Steinhäuser C., Bedner P. (2020). Astrocytic GABA accumulation in experimental temporal lobe epilepsy. Front. Neurol. 11:614923. 10.3389/fneur.2020.614923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller M. S., Fox R., Schousboe A., Waagepetersen H. S., Bak L. K. (2014). Astrocyte glycogenolysis is triggered by store-operated calcium entry and provides metabolic energy for cellular calcium homeostasis. Glia 62 526–534. 10.1002/glia.22623 [DOI] [PubMed] [Google Scholar]
- Mulligan S. J., MacVicar B. A. (2004). Calcium transients in astrocyte endfeet cause cerebrovascular constrictions. Nature 431 195–199. 10.1038/nature02827 [DOI] [PubMed] [Google Scholar]
- Nagelhus E. A., Ottersen O. P. (2013). Physiological roles of aquaporin-4 in brain. Physiol. Rev. 93 1543–1562. 10.1152/physrev.00011.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagelhus E. A., Veruki M. L., Torp R., Haug F. M., Laake J. H., Nielsen S., et al. (1998). Aquaporin-4 water channel protein in the rat retina and optic nerve: polarized expression in Müller cells and fibrous astrocytes. J. Neurosci. 18 2506–2519. 10.1523/jneurosci.18-07-02506.1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nedergaard M. (1994). Direct signaling from astrocytes to neurons in cultures of mammalian brain cells. Science 263 1768–1771. 10.1126/science.8134839 [DOI] [PubMed] [Google Scholar]
- Neligan A., Hauser W. A., Sander J. W. (2012). The epidemiology of the epilepsies. Handb. Clin. Neurol. 107 113–133. 10.1016/b978-0-444-52898-8.00006-9 [DOI] [PubMed] [Google Scholar]
- Neusch C., Rozengurt N., Jacobs R. E., Lester H. A., Kofuji P. (2001). Kir4.1 potassium channel subunit is crucial for oligodendrocyte development and in vivo myelination. J. Neurosci. 21 5429–5438. 10.1523/jneurosci.21-15-05429.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolic L., Nobili P., Shen W., Audinat E. (2020). Role of astrocyte purinergic signaling in epilepsy. Glia 68 1677–1691. 10.1002/glia.23747 [DOI] [PubMed] [Google Scholar]
- Nikolic L., Shen W., Nobili P., Virenque A., Ulmann L., Audinat E. (2018). Blocking TNFα-driven astrocyte purinergic signaling restores normal synaptic activity during epileptogenesis. Glia 66 2673–2683. 10.1002/glia.23519 [DOI] [PubMed] [Google Scholar]
- Nizar K., Uhlirova H., Tian P., Saisan P. A., Cheng Q., Reznichenko L., et al. (2013). In vivo stimulus-induced vasodilation occurs without IP3 receptor activation and may precede astrocytic calcium increase. J. Neurosci. 33 8411–8422. 10.1523/jneurosci.3285-12.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwaobi S. E., Cuddapah V. A., Patterson K. C., Randolph A. C., Olsen M. L. (2016). The role of glial-specific Kir4.1 in normal and pathological states of the CNS. Acta Neuropathol. 132 1–21. 10.1007/s00401-016-1553-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandit S., Neupane C., Woo J., Sharma R., Nam M.-H., Lee G.-S., et al. (2020). Bestrophin1-mediated tonic GABA release from reactive astrocytes prevents the development of seizure-prone network in kainate-injected hippocampi. Glia 68 1065–1080. 10.1002/glia.23762 [DOI] [PubMed] [Google Scholar]
- Parpura V., Basarsky T. A., Liu F., Jeftinija K., Jeftinija S., Haydon P. G. (1994). Glutamate-mediated astrocyte-neuron signalling. Nature 369 744–747. 10.1038/369744a0 [DOI] [PubMed] [Google Scholar]
- Parpura V., Haydon P. G. (2000). Physiological astrocytic calcium levels stimulate glutamate release to modulate adjacent neurons. Proc. Natl. Acad. Sci. U.S.A. 97 8629–8634. 10.1073/pnas.97.15.8629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parri H. R., Crunelli V. (2003). The role of Ca2+ in the generation of spontaneous astrocytic Ca2+ oscillations. Neuroscience 120 979–992. 10.1016/s0306-4522(03)00379-8 [DOI] [PubMed] [Google Scholar]
- Parri H. R., Gould T. M., Crunelli V. (2001). Spontaneous astrocytic Ca2+ oscillations in situ drive NMDAR-mediated neuronal excitation. Nat. Neurosci. 4 803–812. 10.1038/90507 [DOI] [PubMed] [Google Scholar]
- Patel D. C., Tewari B. P., Chaunsali L., Sontheimer H. (2019). Neuron-glia interactions in the pathophysiology of epilepsy. Nat. Rev. Neurosci. 20 282–297. 10.1038/s41583-019-0126-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paukert M., Agarwal A., Cha J., Doze V. A., Kang J. U., Bergles D. E. (2014). Norepinephrine controls astroglial responsiveness to local circuit activity. Neuron 82 1263–1270. 10.1016/j.neuron.2014.04.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekny M., Nilsson M. (2005). Astrocyte activation and reactive gliosis. Glia 50 427–434. 10.1002/glia.20207 [DOI] [PubMed] [Google Scholar]
- Pekny M., Pekna M. (2016). Reactive gliosis in the pathogenesis of CNS diseases. Biochim. Biophys. Acta 1862 483–491. 10.1016/j.bbadis.2015.11.014 [DOI] [PubMed] [Google Scholar]
- Pellerin L., Magistretti P. J. (1994). Glutamate uptake into astrocytes stimulates aerobic glycolysis: a mechanism coupling neuronal activity to glucose utilization. Proc. Natl. Acad. Sci. U.S.A. 91 10625–10629. 10.1073/pnas.91.22.10625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perea G., Navarrete M., Araque A. (2009). Tripartite synapses: astrocytes process and control synaptic information. Trends Neurosci. 32 421–431. 10.1016/j.tins.2009.05.001 [DOI] [PubMed] [Google Scholar]
- Perea G., Sur M., Araque A. (2014). Neuron-glia networks: integral gear of brain function. Front. Cell. Neurosci. 8:378. 10.3389/fncel.2014.00378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perucca P., Gilliam F. G. (2012). Adverse effects of antiepileptic drugs. Lancet Neurol. 11 792–802. 10.1016/s1474-4422(12)70153-9 [DOI] [PubMed] [Google Scholar]
- Petravicz J., Boyt K. M., McCarthy K. D. (2014). Astrocyte IP3R2-dependent Ca2+ signaling is not a major modulator of neuronal pathways governing behavior. Front. Behav. Neurosci. 8:384. 10.3389/fnbeh.2014.00384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petravicz J., Fiacco T. A., McCarthy K. D. (2008). Loss of IP3 receptor-dependent Ca2+ increases in hippocampal astrocytes does not affect baseline CA1 pyramidal neuron synaptic activity. J. Neurosci. 28 4967–4973. 10.1523/jneurosci.5572-07.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plata A., Lebedeva A., Denisov P., Nosova O., Postnikova T. Y., Pimashkin A., et al. (2018). Astrocytic atrophy following parallels reduced Ca2+ activity and impaired synaptic plasticity in the rat hippocampus. Front. Mol. Neurosci. 11:215. 10.3389/fnmol.2018.00215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poskanzer K. E., Yuste R. (2016). Astrocytes regulate cortical state switching in vivo. Proc. Natl. Acad. Sci. U.S.A. 113 E2675–E2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein J. D., Dykes-Hoberg M., Pardo C. A., Bristol L. A., Jin L., Kuncl R. W., et al. (1996). Knockout of glutamate transporters reveals a major role for astroglial transport in excitotoxicity and clearance of glutamate. Neuron 16 675–686. 10.1016/s0896-6273(00)80086-0 [DOI] [PubMed] [Google Scholar]
- Scemes E., Giaume C. (2006). Astrocyte calcium waves: what they are and what they do. Glia 54 716–725. 10.1002/glia.20374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl U. I., Choi M., Liu T., Ramaekers V. T., Häusler M. G., Grimmer J., et al. (2009). Seizures, sensorineural deafness, ataxia, mental retardation, and electrolyte imbalance (SeSAME syndrome) caused by mutations in KCNJ10. Proc. Natl. Acad. Sci. U. S. A. 106 5842–5847. 10.1073/pnas.0901749106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp A. H., Nucifora F. C., Jr., Blondel O., Sheppard C. A., Zhang C., Snyder S. H., et al. (1999). Differential cellular expression of isoforms of inositol 1,4,5-triphosphate receptors in neurons and glia in brain. J. Comp. Neurol. 406 207–220. [DOI] [PubMed] [Google Scholar]
- Shields D. C., Schaecher K. E., Hogan E. L., Banik N. L. (2000). Calpain activity and expression increased in activated glial and inflammatory cells in penumbra of spinal cord injury lesion. J. Neurosci. Res. 61 146–150. [DOI] [PubMed] [Google Scholar]
- Shigetomi E., Saito K., Sano F., Koizumi S. (2019). Aberrant calcium signals in reactive astrocytes: a key process in neurological disorders. Int. J. Mol. Sci. 20 996. 10.3390/ijms20040996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofroniew M. V. (2009). Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci. 32 638–647. 10.1016/j.tins.2009.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhäuser C., Seifert G. (2012). “Astrocyte dysfunction in epilepsy,” in Jasper’s Basic Mechanisms of the Epilepsies, eds Noebels J. L., Avoli M., Rogawski M. A., Olsen R. W., Delgado-Escueta A. V. (Bethesda, MD: National Center for Biotechnology Information; ). [PubMed] [Google Scholar]
- Steinhäuser C., Seifert G., Bedner P. (2012). Astrocyte dysfunction in temporal lobe epilepsy: K+ channels and gap junction coupling. Glia 60 1192–1202. 10.1002/glia.22313 [DOI] [PubMed] [Google Scholar]
- Sun W., McConnell E., Pare J.-F., Xu Q., Chen M., Peng W., et al. (2013). Glutamate-dependent neuroglial calcium signaling differs between young and adult brain. Science 339 197–200. 10.1126/science.1226740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabó Z., Héja L., Szalay G., Kékesi O., Füredi A., Szebényi K., et al. (2017). Extensive astrocyte synchronization advances neuronal coupling in slow wave activity in vivo. Sci. Rep. 7:6018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szokol K., Heuser K., Tang W., Jensen V., Enger R., Bedner P., et al. (2015). Augmentation of Ca2+ signaling in astrocytic endfeet in the latent phase of temporal lobe epilepsy. Front. Cell. Neurosci. 9:49. 10.3389/fncel.2015.00049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian G.-F., Azmi H., Takano T., Xu Q., Peng W., Lin J., et al. (2005). An astrocytic basis of epilepsy. Nat. Med. 11 973–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umpierre A. D., West P. J., White J. A., Wilcox K. S. (2019). Conditional knock-out of mGluR5 from astrocytes during epilepsy development impairs high-frequency glutamate uptake. J. Neurosci. 39 727–742. 10.1523/jneurosci.1148-18.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Vliet E. A., da Costa Araújo S., Redeker S., van Schaik R., Aronica E., Gorter J. A. (2007). Blood-brain barrier leakage may lead to progression of temporal lobe epilepsy. Brain 130 521–534. 10.1093/brain/awl318 [DOI] [PubMed] [Google Scholar]
- Vezzani A., French J., Bartfai T., Baram T. Z. (2011). The role of inflammation in epilepsy. Nat. Rev. Neurol. 7 31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volterra A., Steinhäuser C. (2004). Glial modulation of synaptic transmission in the hippocampus. Glia 47 249–257. 10.1002/glia.20080 [DOI] [PubMed] [Google Scholar]
- Wang F., Smith N. A., Xu Q., Fujita T., Baba A., Matsuda T., et al. (2012). Astrocytes modulate neural network activity by Ca2 -dependent uptake of extracellular K+. Sci. Signal. 5:ra26. 10.1126/scisignal.2002334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellmann M., Álvarez-Ferradas C., Maturana C. J., Sáez J. C., Bonansco C. (2018). Astroglial Ca-dependent hyperexcitability requires P2Y purinergic receptors and pannexin-1 channel activation in a chronic model of epilepsy. Front. Cell. Neurosci. 12:446. 10.3389/fncel.2018.00446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieser H.-G. ILAE Commission on Neurosurgery of Epilepsy. (2004). ILAE Commission Report. Mesial temporal lobe epilepsy with hippocampal sclerosis. Epilepsia 45 695–714. 10.1111/j.0013-9580.2004.09004.x [DOI] [PubMed] [Google Scholar]
- Yang H. Y., Lieska N., Shao D., Kriho V., Pappas G. D. (1994). Proteins of the intermediate filament cytoskeleton as markers for astrocytes and human astrocytomas. Mol. Chem. Neuropathol. 21 155–176. 10.1007/bf02815349 [DOI] [PubMed] [Google Scholar]
- Zhang C., Tabatabaei M., Bélanger S., Girouard H., Moeini M., Lu X., et al. (2019). Astrocytic endfoot Ca correlates with parenchymal vessel responses during 4-AP induced epilepsy: an in vivo two-photon lifetime microscopy study. J. Cereb. Blood Flow Metab. 39 260–271. 10.1177/0271678x17725417 [DOI] [PMC free article] [PubMed] [Google Scholar]