Figure 2.
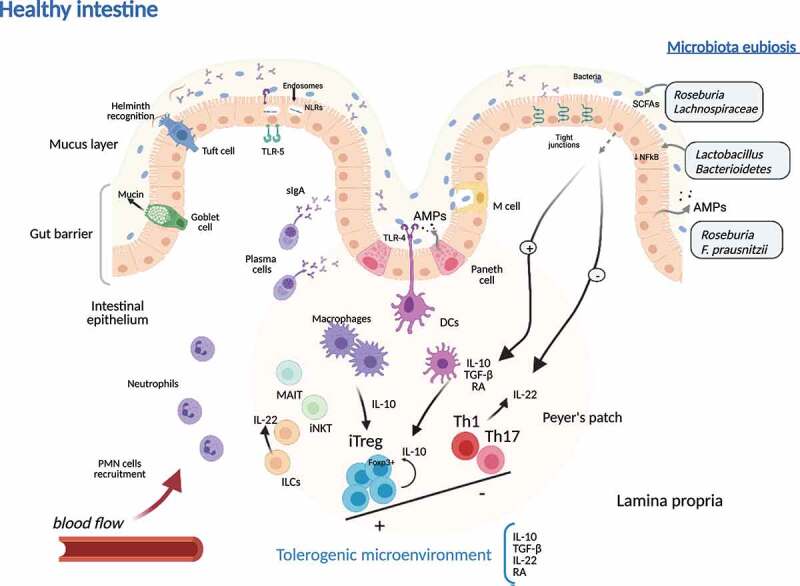
Tolerogenic microenvironment during microbiota eubiosis in healthy intestinal tissue in Crohn’s disease. In healthy colonic tissue, the gut barrier is made up of a thick mucus layer containing mucin produced by Goblet cells, sIgA produced by plasma cells, AMPs secreted by epithelial cell, and the cellular immune system (ILCs, MAIT cells, NKTs, macrophages, dendritic cells and T cells), mainly organized in Peyer’s patches. DCs and macrophages produce anti-inflammatory mediators that promote iTreg Foxp3+ expansion. Moreover, the eubiotic microbiota contributes to reduction of proinflammatory substrates induction (reduced activation of NFkB in epithelial cells) and produces SCFAs and subsequent inhibition of proinflammatory (Th1 and Th17) cell lineage activation. iTregs together with eubiotic microbiota are responsible of the predominant immunotolerance in intestinal tissue microenvironment, while ILC-derived IL-22 contributes to keep gut barrier integrity. sIgA, soluble IgA; AMPs, antimicrobial peptides; ILC, innate lymphoid cells; MAIT, mucosal associated invariant T cell; iNKT, invariant Natural Killer T cell; DC, dendritic cell; iTreg, induced regulatory T cells; NFkB, nuclear factor kappa-B; Th, T helper cell; SCFAs, short chain fatty acids, PMN, polymorphonuclear cells; TLRs, Toll-like receptors; NLRs, Nod-like receptors; IL, interleukin; RA, retinoic acid; TGF-β, transforming growth factor-β
