Abstract
Purpose
The survival rate of a Flight crash is quite low and this makes the Calicut incident unique. Management of flight crash victims is itself a herculean task and during COVID-19 pandemic it poses another challenge to the treating team since all the patients are under quarantine and the treatment protocols are not well defined.
Methods
On 7/8/2020 at around 7.41 pm, Air India Express aircraft from Dubai to Calicut, while landing on the runway lost its control and skidded off the runway and broke into three parts. We report a detailed analysis of orthopaedic injury patterns and difficulties encountered in the management of these patients with full personal protective equipment (PPE) kit during COVID-19 pandemic.
Results
47 patients from the crash site were brought to our hospital and 38 of them were admitted under the orthopaedic department. 74 doctors and 76 trained nurses along with 58 supporting staff were involved in the management of the mass casualty during that night. Most of the patients suffered injuries to lower extremity and spine which included 11 femur, 13 tibial and 12 spine fractures. Average union time was around 3 months for fractures. Delayed union of fracture femur, avascular necrosis of talus and nonunion of 5th metatarsal base fracture were the reported complications. Surgical site infection was observed in two patients.
Conclusion
Trauma management team should be prepared to manage difficulties encountered during identification, communication, and treatment of the disaster victims during this COVID-19 era.
Keywords: Flight crash, COVID-19, Disaster management, Personal protective equipment, Orthopaedic injuries
Introduction
07/08/2020, Air India Express 1344 aircraft coming from Dubai crashed at the airport in Karipur, Calicut, Kerala, India. Aircraft while landing on the table top runway at around 7.41 pm, could not land properly due to heavy rains and skidded off the runway and broke into three parts (Fig. 1).
Fig. 1.
Air India Express 1344 after accident
184 passengers, four cabin crew and two pilots were there in the aircraft. This aircraft was part of the Vande Bharath Mission, helping Indians to return to India from different parts of the world, since most of the international air traffic was suspended all over the world due to COVID-19 pandemic. It was indeed a Black Friday in the history of Kerala. There were landslides near Munnar claiming the lives of more than 80 people, then rising COVID-19 cases, torrential rains, impending floods and to add to all this tragic aircraft accident in Calicut. On receiving the first alert call from the Sub Inspector of Police, Medical College Police Station, our hospital management started preparing to face this mass casualty in the most effective manner.
Disaster Management With Personal Protective Equipment (PPE)
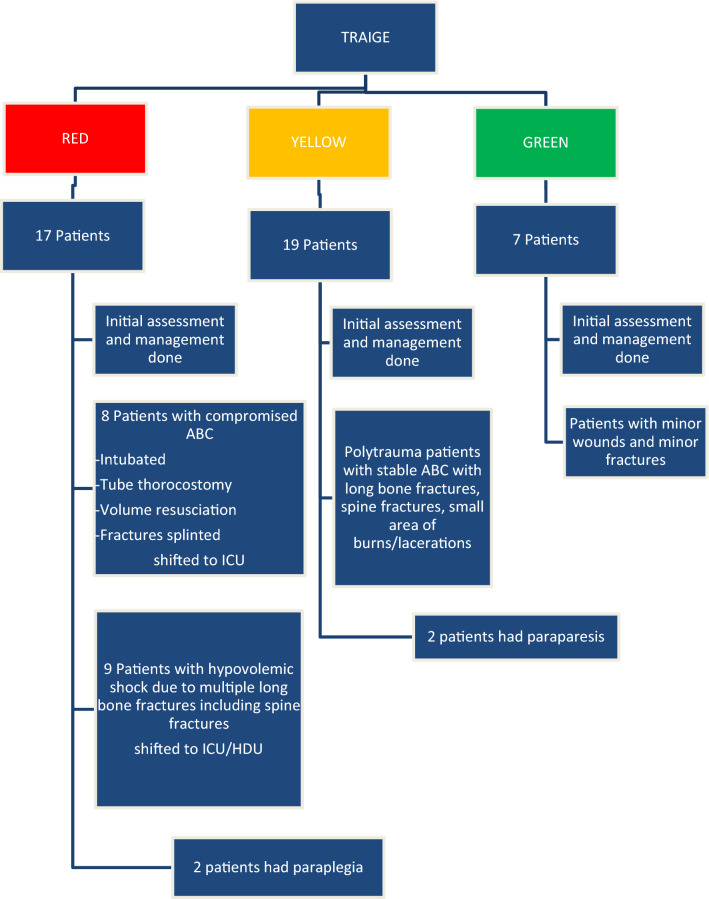
Mobile ICU and ambulances with the medical team in full PPE kit were sent to the Airport. Alerts were sent to all the staff through phone calls and messages to be prepared for receiving patients. Patients in the Emergency Department (ED) were immediately shifted to the wards and ED was ready to receive patients of mass casualty. Radiology, Pharmacy, Blood Bank, Operation Theatre and other allied functions were on alert. PPE kits were sourced from the store. Around 74 doctors from Heads (HOD) to junior residents of various departments and 76 nurses and 58 supporting staff assembled within 20 min in ED. Since patients were from Dubai and were considered as suspected COVID-19 patients, all teams were donned with full PPE. At around 9 pm, the patients started reaching ED. Mass casualty code was announced. Around 47 patients reached our hospital from 9 PM to 1AM. Triaging of patients was done. Patients who sustained polytrauma with airway, breathing and circulatory compromise were categorized as RED, patients who had stable airway, breathing and circulation but with long bone fractures, spine fractures, small area of burns were categorized as YELLOW, patients with minor wounds and minor fractures were categorized as GREEN. 17 patients in RED category, 19 in YELLOW category, 7 in GREEN category and 3 patients were brought dead including the Pilot and the Co-pilot of the aircraft. After Primary survey of Airway, Breathing, Circulation and Disability (ABCD) in ED, the splinting of fractures with Plaster of Paris (POP) was done. Secondary survey was carried out in step down ED area to make facilities /bed for new patients to receive. There was an incident commander assigned for safety, security, liaison, and public information. All patients were admitted under the Orthopaedic Department. Our orthopaedic team consisting of 12 doctors from HOD to junior residents were split into 3 teams, one team for ED, one team for ICU and another team for wards. By around 3 AM the secondary survey of all patients had been completed and the code for mass casualty under control was announced. We had the surge capacity and surge capability and could manage the disaster with ease. In short, the theoretical management strategies of disaster management were put into practice without any fault (Fig. 2).
Fig. 2.
Triage protocol
The biggest difficulty was managing mass casualty in full PPE. Identifying the doctor, nurse and technician posed a major challenge for they were in full PPE uniform. Another hurdle was patient assessment and smooth communication between patient and the doctor and between doctors as they were split into many teams in various places and all their mobile phones were inside PPE. First time in our life, we felt that PPE is a handicap, but there was no other way as we had to follow the guidelines of COVID-19 management. Next difficulty was in identifying the parents and bystanders of children who were admitted to our hospital, since all flight crash victims were admitted under different hospitals in and around the airport. Around five children were under the age of 6 years, getting consent for investigations, operative procedures and explaining the condition of the children became a daunting task for us that night. Our hospital beds were almost full that day including more than 20 COVID-19 patients, even then our hospital handled the situation professionally. We had enough PPE stocks in our hospital. We used nearly 1000 PPEs within the first 24 h for various needs of the management. Waste management in the doffing area was also a challenge. The mock drill that followed a replica of the scenario (flight crash) held at Calicut Airport a few years back helped us and the staff who had participated in that mock drill were still working in our hospital. It was a very good baseline for us to start off and hence we could manage the scenario well. The whole disaster was managed perfectly by adhering to pandemic rules and regulations. Our team managed without any breach in the COVID protocol and the result of this is seen in the fact that none of our personnel tested positive on follow up.
About 12 patients required early surgical intervention and were posted in emergency OT. All open fractures like tibial fractures, malleoli fractures, open/closed talus fractures, calcaneum fractures and unstable spine fractures were treated as emergency surgeries and they were operated within the first two days. Out of the 12 patients 4 were children. All elective surgeries were postponed for a week for the safety of the patients. For all patients, COVID-19 (TrueNat) test was done and only two of the patients admitted were found to be positive. But as the patients were in quarantine period for 14 days, they had to be considered as potentially positive patients, so the protocol for surgeries in Operation Theatre (OT) were followed. We had to do surgery in full PPE in negative pressure OT. It was the most difficult situation for all the doctors and staff of OT who had their worst experience in their lifetime. Firstly, we had to wear OT apron, followed by full PPE (consisting of complete body and head covering gown, plastic cover for OT slippers, N 95 masks, gloves, goggles/eye shield masks), lead aprons due to C arm exposure and finally sterile OT apron and gloves (Fig. 3).
Fig. 3.

Surgical team with full PPE kit and sterile gown
Doing orthopaedic surgery with three layers of apron, one layer of lead apron in addition to fogging of goggles/eye shield masks during surgery with traction and retraction intermittently and sweating due to negative pressure OT was the worst experience we had during these days. We were allotted two operation theatres for doing surgeries for these flight crash accident victims, simultaneously other department’s elective and emergency surgeries were running in other operation theatres. We had to run our outpatient department simultaneously, so it took 7 days to complete the surgeries of these flight crash victims. The patients with closed fractures were considered as elective surgical cases and they were performed after initial 2 days. The operative techniques and methods which were performed for these patients were the same as during non-COVID times and there was no difference in management like conservative or operative/regional or general anaesthesia.
Injury Patterns
Around 38 patients were admitted in the orthopaedic department of our hospital (Table 1). Among them 16 patients were under the age of 14 years. There were 19 male and 21 female patients. 9 patients had no bony injuries and 8 patients had open fractures. Out of 12 patients who sustained spine fractures, surgical stabilization was done in 6. Among the 12 spine fractures, 4 people had neurological complications like paraparesis/paraplegia. Among the paediatric age group, two patients with bilateral femur fractures, three patients with tibia fractures, one patient with humerus fracture, one patient with metacarpal fracture and one patient with type 1 open calcaneum fracture were treated conservatively. Among the adult age group, one clavicle fracture, one metatarsal fracture and two patients with type 3 open calcaneum fractures were treated conservatively. For type 3 open calcaneum fractures, initial surgical debridement followed by flap cover was done. Surgical fixation was performed for all other fractures. Out of seven patients who sustained femur fractures, four had bilateral involvement. Out of six patients who had both bone leg fractures, three were open. There were three intra-articular proximal tibial and four intra-articular distal tibial fractures and all four distal tibia fractures were open fractures. Out of the five patients presented with talar fractures, four were Hawkins type 4 talus fracture dislocations. Two patients had bimalleolar ankle fracture dislocations. All three patients who presented with calcaneus fractures were open. Ten patients had upper extremity fractures, four humerus shaft, three distal humerus and one proximal humerus fractures. Three patients had clavicle fractures and two of them had scapula fracture also. Of all the patients only three were presented with rib fractures (Table 2).
Table 1.
List of injuries and their management
| S. no | Age/sex | Diagnosis | Treatment | No of days after crash operation done |
|---|---|---|---|---|
| 1 | 13/M | Closed comminuted shaft of femur fracture right, closed shaft of femur fracture left and closed shaft of tibia fracture left | ORIF plating right femur, IM nailing left femur | 3rd day |
| 2 | 9/M | Type 1 open fracture calcaneum left, closed fracture neck of talus right | ORIF talus right | 1st day |
| 3 | 11/M | Type 2 open fracture both bone left leg | TENS nailing left tibia, VAC dressing back | 2nd day |
| 4 | 6/F | Closed supracondylar fracture right elbow, closed shaft of femur fracture right, closed both bone fracture left leg | ORIF K wire right elbow, ORIF with TENS nail left tibia, ORIF plating right femur | 3rd day |
| 5 | 10/M | Closed supracondylar fracture right elbow, type 3B open ankle posterolateral dislocation with medial malleolus fracture right, type 3A open both bone fracture left leg | CMR K wire right elbow, ORIF K wire medial malleolus right ankle, K wire tibia left leg | 1st day |
| 6 | 11/F | Closed both bone fracture left leg | POP | |
| 7 | 5/M | Closed fracture shaft of humerus right | POP | |
| 8 | 5/M | Type 3B open fracture both bone right leg | K wire fixation right tibia | 1st day |
| 9 | 15/M | Chip fracture distal tibia left ankle | POP | |
| 10 | 4/F | Closed shaft of femur fracture bilateral, mild SAH | Hip spica | 2nd day |
| 11 | 34/M | L2 chance fracture with paraparesis | L1-L3 instrumentation, decompression | 1st day |
| 12 | 30/F | Zone 2 sacral fracture b/l with spinopelvic dissociation, scapula and clavicle fracture right, fracture 2nd, 3rd, 4th ribs, spinous process fracture D1, D2, D3 | spinopelvic fixation L4-S2 screws and decompression | 3rd day |
| 13 | 63/M | Spinous process fracture D2 | conservative | |
| 14 | 24/F | Compression fracture D3, D4,D5,D6,D7, Spinous process fracture C7, D1-D6 | conservative | |
| 15 | 31/F | D3 chance fracture | Not willing for surgery | |
| 16 | 46/F | 5th metatarsal base fracture right foot | ORIF 5th metatarsal right | 1 month |
| 17 | 29/M | L5 transverse process fracture | conservative | |
| 18 | 21/F | Right clavicle fracture, D5 and D6 fracture, left hip dislocation | CMR left hip | Same day |
| 19 | 36/M | Fracture right orbitozygomatic complex, maxilla, open fracture dislocation left ankle with talus bone loss, fracture proximal tibia right, type 3 open fracture both bone distal third right, type 2 open fracture right distal humerus, L3 burst fracture, multiple rib fractures | ORIF right orbitozygomatic complex, L2-L4 instrumentation and decompression, ORIF right humerus, ORIF right proximal tibia and right distal tibia | 1st day |
| 20 | 23/F | Closed proximal tibia fracture right, open fracture distal tibia + calcaneum with heel pad avulsion right, closed humerus fracture left, closed distal femur comminuted fracture left, closed intra-articular distal humerus fracture with proximal ulna fracture right, L3 burst fracture with paraparesis | ORIF right distal humerus + olecranon, ORIF left humerus + distal femur, L2-L4 instrumentation and decompression, ORIF right proximal tibia | 1st day |
| 21 | 14/F | Epiphyseal injury right 1st metacarpal | POP | |
| 22 | 29/M | D12 compression fracture | conservative | |
| 23 | 32/F | Closed b/l femur fracture, type 2 open fracture distal both bone right leg, type 3 open comminuted calcaneum left | B/L IM nailing femur, ORIF distal tibial and medial malleolus right | 1st day |
| 24 | 30/F | Closed humerus shaft fracture left, medial malleolus and talus fracture left ankle | ORIF left humerus, ORIF left talus and medial malleolus | 2nd day |
| 25 | 51/M | Comminuted fracture proximal humerus right, clavicle and scapula fracture right, bimalleolar fracture right ankle, L3 burst fracture with paraplegia | ORIF right clavicle and proximal humerus, ORIF right ankle, L2-L4 spine instrumentation and decompression | 2nd day |
| 26 | 50/M | Type 3B open comminuted distal tibia fracture right + closed talus fracture left and lateral malleolus fracture, L2 chance fracture with paraplegia | ORIF tibia, D12-L3 instrumentation and decompression, ORIF talus and lateral malleolus left | 2nd day |
| 27 | 27/M | closed humerus fracture left, closed femur fracture and both bone forearm fracture right, closed fracture dislocation talus and medial malleolus fracture left, closed metatarsal fractures right foot | ORIF humerus left, both bone forearm right, talus and medial malleolus left, IM nailing right | 2nd day |
| 28 | 53/M | Closed comminuted fracture proximal tibia and fibula right, multiple rib fractures | ORIF proximal tibia right | 14 days |
| 29 | 4/F | Closed bilateral distal femur fracture | Hip spica | 2nd day |
Table 2.
Fracture distribution
| Bone affected | Number of fractures |
|---|---|
| Femur | 11 |
| Tibia | 13 |
| Malleoli | 2 |
| Talus | 5 |
| Calcaneum | 3 |
| Spine | 12 |
| Humerus | 8 |
| Clavicle | 3 |
| Scapula | 2 |
Results
All the patients were followed up regularly. The average union time for the fractures is around 3 months post operatively. Five patients had complications which included delayed union of femur fracture, avascular necrosis of talus, nonunion of 5th metatarsal base fracture which was initially treated in the conservative method. Two patients had surgical site infection due to open fractures. Four patients who had spine fractures with initial neurological complications are recovering neurologically (Table 3).
Table 3.
Neurological status of spine patients
| Age/sex | Diagnosis | Neurology at admission | Neurology at follow up |
|---|---|---|---|
| 34/M | L2 Chance fracture | ASIA B | ASIA E |
| 23/F | L3 Burst fracture | ASIA B | ASIA D |
| 51/M | L3 Burst fracture | ASIA A | ASIA D |
| 50/M | L2 chance fracture | ASIA A | ASIA D |
Discussion
Multiple casualty incidents like earthquakes, landslides, train accidents, etc. are possible in any community. Disaster management planning and execution is very important and the role of the disaster team should be well defined. Medical personnel with adequate knowledge of the plan should take in-charge during disaster and direct other personnel. Adequate number of medical and paramedical personnel with well-organized and defined roles are necessary to manage a disaster [1]. Flight crash accidents in airports are a very rare incidence and the management of these casualties during COVID-19 pandemic is really a tough task. In 2012, mock disaster exercise was performed at Calicut airport, the crash site. Medical personnel from our hospital with the specified role of disaster management performed at the mock exercise. Since some of the medical personnel are still working in our hospital, we could handle the disaster very well.
The guidelines for evidence-based disaster planning like sending emergency response units to the scene, trained medical personnel carrying out triage and providing first aid services, transportation of victims to different hospitals in and around the disaster scene so that no hospital receives disproportionate number, evacuating ED beds to open for incoming most serious patients should be followed for adequate management of disaster [2]. Most of the seriously injured patients reached our hospital in ambulances, but some patients who were less injured reached our hospital by private vehicles. The transportation of these flight crash patients with spine boards is very important since there may be chances of undiagnosed spinal injuries in less injured patients as reported by Postma et al. [3].
Turkish airline crash in 2009 [4, 5] reported that most of their injuries were to head and face followed by the spinal and extremity injuries. But our cohort shows a different pattern with a high percentage of extremity injuries followed by spinal injuries, but injuries to head and face is nearly negligible. This orthopaedic injury pattern, flight crash incident and the number of survivors of the plane crash is similar to the study of Iran airplane crash [6]. This may be attributed to the fact that the airplane nearly cleared the runway while landing and skidded off the runway at very low speed in the end and the impact caused is mostly extremity injuries and spinal injuries. Nearly all the passengers were on seat belts which might be a cause for less injury to head and face. Lower limb fracture is the most common aviation related injury reported by Baker et al. [7] and Chalmers et al. [8] which is similar to our cohort. The high number of survivors is because of relatively low speed of the airplane during landing and it was not complicated by fire or explosion of the plane [9].
During this multiple casualty incident, a large casualty caseload seriously affects the quality of trauma care given to individual patients. Hence the goal of hospital emergency plans is to provide severely injured patients with a level of care given similar to the patients under normal conditions. Triaging at ED door and adequate hospital capacity to receive mass casualty are key to successful management of disaster. There are 2 stages in the management of non-critical casualties in a disaster. First stage is while the casualties are arriving at the hospital, the minimal acceptable care should be given, like splinting of long bone fractures, placement of chest tubes for penetrating chest injuries and adequate analgesia. Second stage is providing definite care to all casualties in a graded and priority-oriented fashion. This stage happens once the casualties are no longer arriving and the patient load is well defined. Hence the main responsibility of trauma care providers during a disaster is to conserve the resources and facilities that will enable the hospital to provide optimal care to the patients [10].
The most difficult problem we encountered in this plane crash was the case of a pregnant lady with bilateral femur fracture. The problem in this case was to suggest radiological investigations to know the type of fracture and to rule out other injuries. Due to the severe trauma and stress in this patient, the signs of life of foetus started deteriorating. We finally had to take a call to save the life of mother which was of utmost importance and did medical termination of pregnancy. Intra medullary nailing of bilateral femur was done subsequently.
Flight crash accidents with mass casualty management in this COVID-19 pandemic period is an eye opener for every medical personnel, especially orthopaedic surgeons in the world. Everyone should be aware of the difficulties in identification, communication, and management of these flight crash victims with a full PPE kit since they are under quarantine. Organizing mock disaster drills regularly and execution of such a plan will ensure the best possible use of the healthcare system in the event of a disaster. A further research of this air crash incident collecting all patients’ reports from different hospitals where patients had been admitted will give a deep insight to the injury patterns of the victims.
Funding
No funding was received in support of this work.
Declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This study was reviewed and approved by IRB.
Informed consent
For this type of study formal consent is not required.
References
- 1.Gerace RV. Role of medical teams in a community disaster plan. Canadian Medical Association Journal. 1979;120(8):923–928. [PMC free article] [PubMed] [Google Scholar]
- 2.Auf der Heide E. The importance of evidence-based disaster planning. Annals of Emergency Medicine. 2006;47(1):34–49. doi: 10.1016/j.annemergmed.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 3.Postma ILE, Weel H, Heetveld MJ, van der Zande I, Bijlsma TS, Bloemers FW, et al. Mass casualty triage after an airplane crash near Amsterdam. Injury. 2013;44(8):1061–1067. doi: 10.1016/j.injury.2013.03.038. [DOI] [PubMed] [Google Scholar]
- 4.Winkelhagen J, Bijlsma TS, Bloemers FW, Heetveld MJ, Goslings JC. Airplane crash near Schiphol Airport 25 February 2009: Injuries and casualty distribution. Nederlands Tijdschrift Voor Geneeskunde. 2010;154:A1064. [PubMed] [Google Scholar]
- 5.Postma ILE, Winkelhagen J, Bloemers FW, Heetveld MJ, Bijlsma TS, Goslings JC, et al. February 2009 airplane crash at Amsterdam Schiphol Airport: An overview of injuries and patient distribution. Prehospital and Disaster Medicine. 2011;26(4):299–304. doi: 10.1017/S1049023X11006467. [DOI] [PubMed] [Google Scholar]
- 6.Mirzatolooei F, Bazzazi A. Analysis of orthopedic injuries in an airplane landing disaster and a suggested mechanism of trauma. European Journal of Orthopaedic Surgery & Traumatology. 2013;23(3):257–262. doi: 10.1007/s00590-012-0973-4. [DOI] [PubMed] [Google Scholar]
- 7.Baker SP, Brady JE, Shanahan DF, Li G. Aviation-Related Injury Morbidity and Mortality: Data from U.S. Health Information Systems. Aviation, Space, and Environmental Medicine. 2009;80(12):1001–1005. doi: 10.3357/ASEM.2575.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chalmers DJ, O’Hare DP, McBride DI. The incidence, nature, and severity of injuries in New Zealand civil aviation. Aviation, Space, and Environmental Medicine. 2000;71(4):388–395. [PubMed] [Google Scholar]
- 9.Friedman A, Floman Y, Sabatto S, Safran O, Mosheiff R. Light Aircraft Crash±A Case Analysis of Injuries. Injury. 2002;12:L1. [PubMed] [Google Scholar]
- 10.Hirshberg A, Holcomb JB, Mattox KL. Hospital trauma care in multiple-casualty incidents: A critical view. Annals of Emergency Medicine. 2001;37(6):647–652. doi: 10.1067/mem.2001.115650. [DOI] [PubMed] [Google Scholar]