Introduction
Liver cancer is a prominent cause of cancer death in the US.1 Rates of hepatocellular carcinoma (HCC), the most common histologic subtype,2 increased for decades,3 until recent years when rates flattened,4 and then potentially declined. Previously, we reported that US HCC rates in 2016 were 4% lower than 2015,5 however, it was unclear from those data whether that finding reflected a true downward trend. Here, we examine HCC rates through 2017.
Methods
Data on HCC were obtained from 21 cancer registries in the Surveillance, Epidemiology and End Results Program. Cases were identified using International Classification of Diseases for Oncology, 3rd edition, codes (site: C22.0; histology: 8170–8175). Incidence rates for 2000–2017 were age-standardized to the 2000 US population in five-year age groups. Using Joinpoint regression, we identified statistically significant (p<0.05) changes in rate trajectories and estimated annual percent changes (APCs) in rates.
Data on American Indian/Alaska Natives were restricted to purchased/referred care delivery areas to reduce racial misclassification. In a sensitivity analysis, delay-adjustment corrections for liver and intrahepatic bile duct cancers were applied to HCC rates to assess whether the decline was driven by reporting delays.6
Results
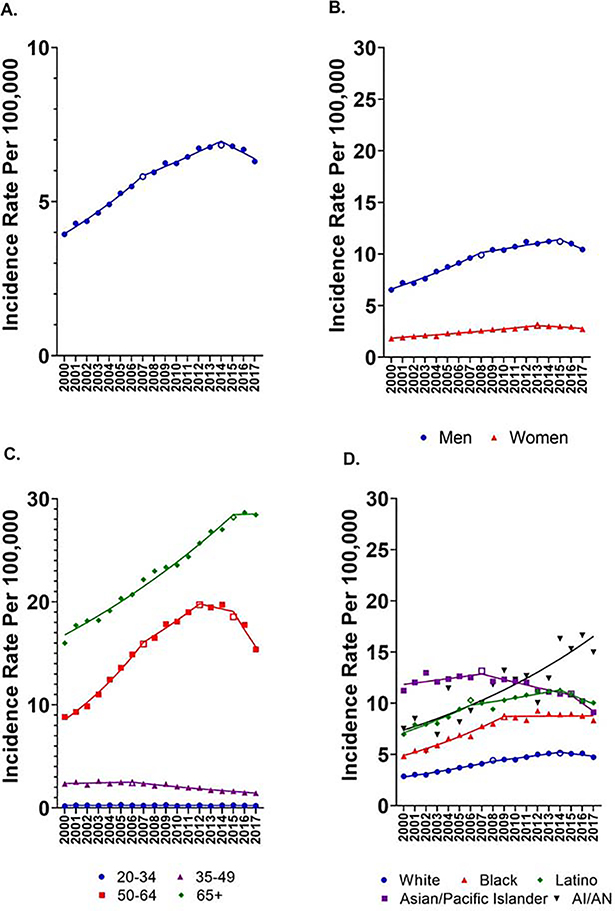
Overall HCC rates increased from 3.94/100,000 in 2000 to a peak of 6.83/100,000 in 2014 before declining to 6.30/100,000 in 2017. HCC incidence increased 5.71%/year during 2000–07 and 2.54%/year during 2007–2014, but then declined 2.79%/year during 2014–2017 (Figure 1; Supplemental Table 1). HCC rates increased among men through 2015 and among women through 2013, before declining non-significantly. HCC trends varied substantially by registry (Supplemental Figure 1). The results were attenuated, though consistent, when accounting for delayed reporting (2014–17; APC=−1.59; 95%CI −3.29, 0.13).
Figure 1:
Age-standardized hepatocellular carcinoma incidence rates, 2000–2017 A) overall, B) by sex, C) by age and D) by race/ethnicity. Symbols indicate incidence rates, lines represent trends between joinpoints, and open symbols represent joinponts. AI/AN: American Indian and Alaska Natives. Note that the scale in panel A differs from the other panels.
By age group, the highest HCC rates were observed in those aged ≥65 years (2017: 28.4/100,000), with rates increasing 3.58%/year during 2000–2015 before plateauing during 2015–2017. In 50–64-year-olds, HCC rates increased during 2000–2012 before plateauing during 2012–2015 and then declining 9.45%/year during 2015–2017. Among 35–49-year-olds, rates were stable during 2000–2006 and then declined 4.83%/year during 2006–2017. HCC rates among 20–34-year-olds remained low (2017: 0.22/100,000) and relatively stable over the entire period (APC=−0.29).
Among Asian/Pacific Islanders, HCC rates declined 2.17%/year during 2007–2015 and then decreased 7.52%/year during 2015–2017. Beginning in 2014, HCC rates declined 4.18%/year among Latinos and 2.56%/year among Whites, although this trend was not statistically significant among Whites. HCC rates have remained steady in Blacks since 2009. In contrast, among American Indians/Alaska Natives, HCC rates increased 4.87%/year during the entire period.
Discussion
After years of increasing rates, a drop in overall US HCC incidence started in 2014. This decrease began among 35–49-year-olds in 2006 and among 50–64-year-olds in 2015. HCC incidence has not yet declined in ≥65-year-olds. In recent years, HCC incidence fell among Asian/Pacific Islanders, Latinos and Whites, while remaining stable in Blacks and continuing to increase among American Indians/Alaska Natives. Though our work overlaps with other recent research that utilizes SEER data, 5, 7, 8 this study uniquely emphasizes the significant downward trend in HCC during 2014–2017.
The main causes of HCC in the United States are chronic infection with hepatitis B virus (HBV) or hepatitis C virus (HCV), alcohol consumption and obesity.9 SEER does not collect information on etiologic risk factors, therefore, we can only speculate about reasons for the temporal trends and demographic differences we observed. It is unlikely that recent declines reflect changes in alcohol use or obesity, as the prevalence of these risk factors has not decreased. Baby boomers are the birth cohort with the highest HCV prevalence.10 Upward and then downward trends among 50–64-year-olds roughly correspond with movement of the cohort born in 1945–1964 through that age range. Increasing mortality in baby boomers, as well as the availability of more effective treatments for HBV and HCV, may explain recent HCC declines. Observed racial/ethnic differences in HCC rates likely reflect differences in underlying risk factors. Regional variation may reflect geographic differences in HCC etiology. Recently published studies have also shown variation in HCC rates by rural/urban status and household income.7, 8
Cancer registry data are limited by potential delays in reporting, which can result in the appearance of lower rates in the most recent years; however, after applying delay adjustment, the trends remained consistent.
In recent decades U.S. rates decreased for a number of cancer sites,1 however, HCC was a notable exception. Now, after many years of increasing incidence, HCC appears to be in decline. Future studies using databases that incorporate etiologic information, such as SEER-Medicare or managed health plans, are needed to understand trends in HCC incidence overall and differences across racial/ethnic groups.
Supplementary Material
Acknowledgments
The funder reviewed and approved the final version of the manuscript, but was not involved in the study design, analysis or drafting of the manuscript.
This work was funded by the Intramural Research Program of the National Cancer Institute.
Both authors were responsible for the study design and drafting of the manuscript. MS was responsible for data analysis.
Footnotes
The authors have no conflicts of interest to declare.
Dr. O’Brien presented an abstract based on these data at the American Association for the Study of Liver Diseases annual meeting.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Henley SJ, Ward EM, Scott S, et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer. 2020;126(10):2225–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ha J, Yan M, Aguilar M, et al. Race/ethnicity-specific disparities in cancer incidence, burden of disease, and overall survival among patients with hepatocellular carcinoma in the United States. Cancer. 2016;122(16):2512–23. [DOI] [PubMed] [Google Scholar]
- 3.Islami F, Miller KD, Siegel RL, et al. Disparities in liver cancer occurrence in the United States by race/ethnicity and state. CA Cancer J Clin 2017;67(4):273–89. [DOI] [PubMed] [Google Scholar]
- 4.Rich NE, Yopp AC, Singal AG, et al. Hepatocellular Carcinoma Incidence Is Decreasing Among Younger Adults in the United States. Clin Gastroenterol Hepatol 2020;18(1):242–8 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shiels MS, O’Brien TR. Recent Decline in Hepatocellular Carcinoma Rates in the United States. Gastroenterology. 2020;158(5):1503–5 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Midthune DN, Fay MP, Limin XC, et al. Modeling Reporting Delays and Reporting Corrections in Cancer Registry Data. Journal of the American Statistical Association. 2005;100(469):61–70. [Google Scholar]
- 7.Wong RJ, Kim D, Ahmed A, et al. Patients with hepatocellular carcinoma from more rural and lower-income households have more advanced tumor stage at diagnosis and significantly higher mortality. Cancer. 2021;127(1):45–55. [DOI] [PubMed] [Google Scholar]
- 8.Wong RJ, Saab S, Konyn P, et al. Rural-Urban Geographical Disparities in Hepatocellular Carcinoma Incidence Among US Adults, 2004–2017. Am J Gastroenterol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hales CM, Carroll MD, Fryar CD, et al. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. NCHS Data Brief. 2020(360):1–8. [PubMed] [Google Scholar]
- 10.Armstrong GL, Wasley A, Simard EP, et al. The Prevalence of Hepatitis C Virus Infection in the United States, 1999 through 2002. Annals of Internal Medicine. 2006;144(10):705–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.