Figure 1.
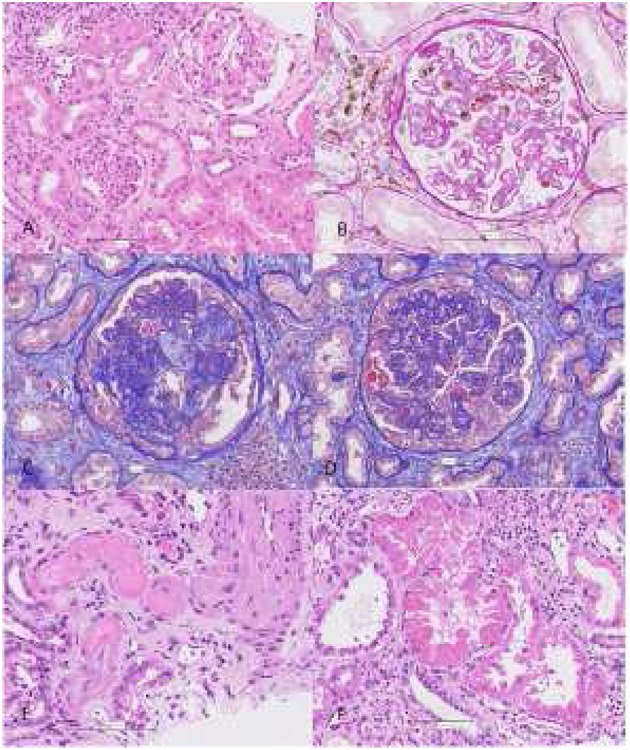
Before application of MSCs (March 2019): chronic active C4d negative antibody-mediated rejection with preserved tubules (A), focal glomerulitis and peritubular capillaritis (B). According to Banff 2017 criteria, transplant kidney biopsy was consistent with chronic active C4d negative antibody mediated rejection: 12% glomerulitis with double contour formation (g1, cg3) in glomeruli, diffuse severe peritubular capillaritis (ptc3), chronic active vascular rejection (v1, cv3) in interlobular arteries without signs of thrombotic microangiopathy, diffuse more than 50% interstitial fibrosis and tubular atrophy with mild mononuclear cell inflammation consisting of lymphocytes, macrophages, and rare plasma cells (i-IFTA 3, ci3, ct3). There was no associated tubulitis. Peritubular capillary basement membrane multilamellation (ptcbm3) was seen by electron microscopy. There were no deposits in tubular basement membrane. Immunofluorescence revealed IgA deposits indicating IgA nephropathy recurrence. 60% of glomeruli were globally sclerotic. 1 of 25 glomeruli showed pseudocrescent formation without PAS positive droplets in podocytes. After application of MSCs (July 2019): glomerular TMA with mesangiolysis (C), diffuse pseudocrescent formation in glomeruli with marked podocytes injury (D), vascular TMA (E) and huge tubular injury with resorptive droplets consisted with mottled lysosomes on EM (F). Glomeruli showed advanced double contour formation and segmental sclerosis without apparent glomerulitis, but mesangiolysis was seen in some glomeruli. 20% of glomeruli showed pseudocrescent formation with PAS positive droplets “in podocytes indicating huge podocytes injury”. Peritubular capillaritis was mild and focal. Tubulitis was absent. Tubules show signs of severe tubular injury (attenuation of tubular epithelium with coarse vacuolization, loss of brush border, loss of nuclei) and were filled with large PAS-positive droplets in line mottled lysosomes on electron microscopy. Electron optic dense deposits in tubular basement membrane were detected by EM. Amount of interstitial fibrosis, tubular atrophy, and interstitial inflammation was similar as in previous biopsy. In fibrotic areas, there was mild mononuclear cell inflammation consisting of lymphocytes 75%, macrophages 15%, and plasma cells 10%. No CD105+, CD73+ nor CD90+ cells were found. In small arteries and arterioles, thrombotic microangiopathy with obliteration of vascular lumens, fragmentation of erythrocytes, and fibrinoid necrosis was present. Peritubular capillary basement membrane multilamellation (ptcbm3) was similar as in previous biopsy.
