Figure 3.
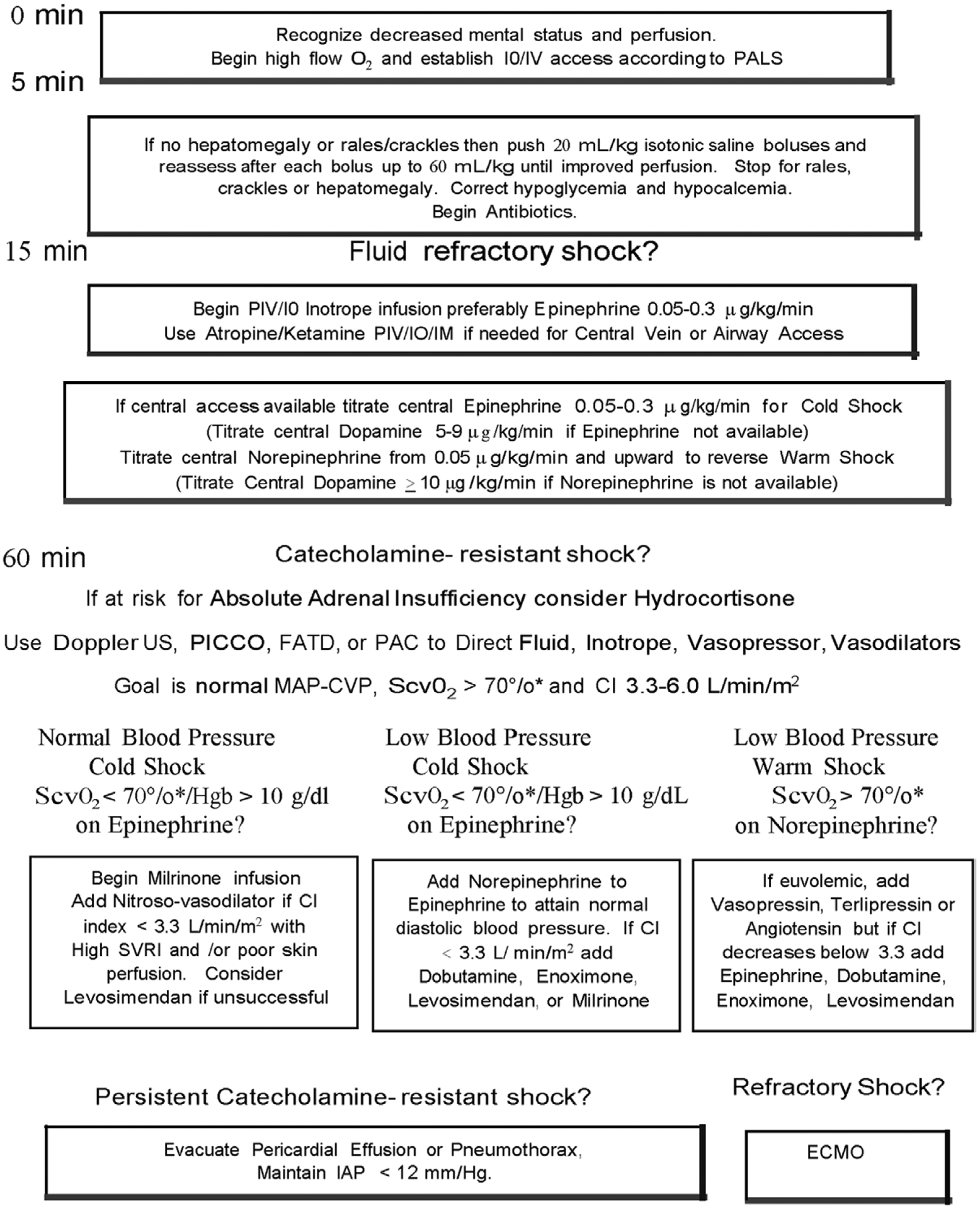
American College of Critical Care Medicine algorithm for time sensitive, goal-directed stepwise management of hemodynamic support in infants and children during resuscitation and stabilization. Proceed to next step if shock persists. 1) First-hour goals—restore and maintain heart rate thresholds, capillary refill less than or equal to 2 s, and normal blood pressure in the first hour/emergency department. 2) Subsequent ICU goals—if shock not reversed, proceed to restore and maintain normal perfusion pressure (mean arterial pressure [MAP] minus central venous pressure [CVP]) for age, central venous oxygen saturation at right atrial/vena cava junction level (Scvo2) greater than 70% (*except congenital heart patients with mixing lesions for whom this is too high), and cardiac index (CI) > 3.3 < 6.0 L/min/m2 in PICU. ECMO = extracorporeal membrane oxygenator, FATD = femoral artery thermodilution catheter, Hgb = hemoglobin, IM = intramuscular, IO = intraosseous line, PAC = pulmonary artery catheter, PALS = Pediatric Advanced Life Support, PICCO = pulse index contour cardiac output catheter, PIV = peripheral IV line, SVRI = systemic vascular resistance index, US = ultrasound.
