By definition, a perforator flap is nourished by only one or more vessels passing through or piercing the underlying muscle before spreading to the corresponding cutaneous area [1] and perforators can be divided into direct cutaneous perforator, septocutaneous perforators, or musculocutaneous perforators. The average perforator caliber is between 0.5 mm and 1 mm. The concept of super microsurgery involves microneurovascular anastomosis for smaller vessels and a single nerve fascicle, as well as microvascular dissection for these small vessels less than 0.3 to 0.8 mm in diameter [2].
During harvesting, handling, or inset of a free flap vascular pedicle injury may occur potentially leading to total failure or severe complications.
The super microsurgical technique provides the ability to solve complications related to accidental injuries of the pedicle or perforator of free flaps. Arterial and venous grafts can be performed by connecting the distal perforating arteries [3], instead of harvesting another free flap, and the time of surgery can be reduced if this technique is applied as microsurgical flap salvage. Resources such as 11-0 or 12-0 sutures must be available to perform this technique to minimize injuries of the pedicle or perforator.
The study was performed with ethical committee approval and following the ethical principles of the Declaration of Helsinki. From 2010 to 2019, eight cases of free flap for different types of reconstruction had accidental disruption or transection of the perforator during flap harvesting. These included (1) free groin flaps to the hand, (2) a superficial circumflex iliac perforator (SCIP) flap to the hand, (3) 2 the lateral digital artery in the toes, (4) a single perforator of a fibula osteocutaneous flap, and (5) single perforators in anterolateral thigh (ALT) flaps (Table 1). The flaps were harvested under only loupes magnification.
Table 1.
Cases of perforator-to-perforator repair
| Flap | Inset location | Cases | Complications | Other associated procedures |
|---|---|---|---|---|
| Groin | To the hand | 2 | No | No |
| SCIP | To the hand | 1 | No | No |
| Toe (wrap- around flap and second toe flap) | To the thumb To the long finger | 2 | No | No |
| Fibula osteocutaneous | For mandible reconstruction | 1 | No | No |
| ALT | For a chronic ulcer | 2 | 1 Failure | 1 Vein graft |
SCIP, superficial circumflex iliac perforator; ALT, anterolateral thigh.
The fibula flap was harvested under a tourniquet and the injury was detected after deflating the tourniquet. The perforator was repaired under microscopy before separating it from the main pedicle and insetting it. After the injury was detected the perforator was repaired immediately with an 11-0 Ethilon suture, and blood flow was tested before division of the main pedicle to check the perfusion of the skin island. The free flap was transferred and blood perfusion was tested again after the microvascular anastomosis. In one ALT flap, the artery was cut during the intramuscular dissection (Fig. 1) and was elongated with a vein graft from the wrist site and anastomosed with 11-0 nylon (Fig. 2). In the second ALT flap, the fascia was incised to elongate the injured vessel and the anastomosis was performed with 12-0 nylon.
Fig. 1.

Intramuscular dissection of the perforator.
Fig. 2.
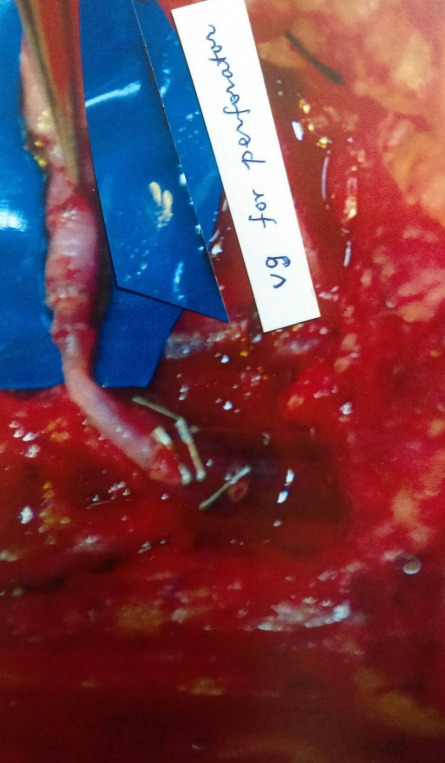
Vein graft to elongate the perforator.
The lateral digital artery of the wrap-around flap and the second toe transfer flap were injured by the monopolar electrocautery device and repaired by cutting the injured site and anastomosing the proximal and distal stump with 12-0 nylon. The groin and SCIP flaps were repaired directly.
All flaps except one survived well without partial loss of tissue. The ALT and fibula flaps were elevated in the subfascial plane, and the groin flap and SCIP flap were elevated in the suprafascial plane. The postoperative care for the flaps consisted of 5,000 units of heparin diluted in 500 mL of 5% glucose, administered at 20 mL/hr for 3 to 5 days, and dextran 40 administered 100 mL as the loading dose, followed by continual infusion at 20 mL/hr for 3 days. The failed flap was a large ALT flap in a chronic ulcer patient with a (methicillin resistant Staphylococcus aureus infection). Although repeated debridement was done before flap surgery, the wound might have still been contaminated with bacteria, and even though we administered the patient antibiotics the tiny perforator repaired with a vein graft might not have been able to withstand invasion by the remaining toxic bacteria. After the ALT flap failed and was removed and the infection was controlled, we performed a latissimus dorsi flap to close the wound.
In this report the injuries resulted from sharp dissection of the perforator, cauterization by a monopolar electrocautery device, and mishandling of the perforator flaps during harvesting. We also used a vein graft to elongate the perforator when abrupt avulsion or coagulation occurred with the electrocautery device due to removal of the damaged segment. Even though the wrap-around flap and second toe flap are not considered to be perforator flaps, they were included in this study because the lateral digital artery size is comparable to that of any perforator. On average, the perforator caliber was 0.5 mm to 0.8 mm. Anastomosis of an injured perforator is a practically applicable salvage procedure that has been described elsewhere [4]. In that study, more injuries occurred due to mishandling than due to accidents in harvesting. Refinement of the dissection technique improves every day for our staff, and our rate of injuries caused by mishandling is low; however, we urge all surgeons to be careful when handling the perforator vessels to prevent injury.
Furthermore, it is not necessarily the case that complete skeletonization of the perforator vessels increases the risk of injury [4].
Although anastomosis of the injured perforator vessel is recommended as a salvage procedure, anastomosis requires supermicrosurgical skills and involves risk of thrombosis.
Failure of injured vessels after repair was associated with infection after anastomosis, and vein grafts have been shown to be associated with free flap failure or complications in salvage procedures [5]. In secondary free flaps, a vein graft is more often needed when the reconstruction is required due to initial free flap failure.
If a free flap is determined to be unsalvageable, the treatment strategy should be chosen based on many factors. The perforator-to-perforator technique is well known as a salvage procedure although it has been associated with a high risk of thrombosis some studies have not confirmed that same finding.
In summary supermicrosurgical skills help to perform salvage procedure when perforator injuries occur during free flaps harvesting as a result of sharp dissection, cauterization or avulsion of the pedicle or perforator. When the perforator is divided during harvesting surgery, it still can be repaired for flap transfer. However, in the presence of potential infection management strategy is to elevate a new flap for anastomosis of large vessels, which are more resistant to infection.
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of China Medical University Hospital (IRB No. CMUH108-REC3-185) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.
Author contribution
Conceptualization: J Velazquez-Mujica, HC Chen. Data curation: J Velazquez-Mujica, D Aksoyler. Formal analysis: J Velazquez-Mujica, L Losco, HC Chen. Methodology: J Velazquez-Mujica, L Losco, D Aksoyler. Project administration: D Aksoyler. Visualization: L Losco. Writing - original draft: J Velazquez-Mujica. Writing - review & editing: HC Chen.
REFERENCES
- 1.Faga A, Nicoletti G, Carminati M. Perforator flaps: current concept and definition. Rivista Italiana di Chirurgia Plastica. 2001;33:27–32. [Google Scholar]
- 2.Koshima I, Yamamoto T, Narushima M, et al. Perforator flaps and supermicrosurgery. Clin Plast Surg. 2010;37:683–9. doi: 10.1016/j.cps.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Hong JP, Koshima I. Using perforators as recipient vessels (supermicrosurgery) for free flap reconstruction of the knee region. Ann Plast Surg. 2010;64:291–3. doi: 10.1097/SAP.0b013e3181ac4263. [DOI] [PubMed] [Google Scholar]
- 4.Miyamoto S, Sakuraba M, Nagamatsu S. Inadvertent injury of critical perforator vessels during perforator flap surgery. J Reconstr Microsurg. 2012;28:95–8. doi: 10.1055/s-0031-1287673. [DOI] [PubMed] [Google Scholar]
- 5.Bozikov K, Arnez ZM. Factors predicting free flap complications in head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2006;59:737–42. doi: 10.1016/j.bjps.2005.11.013. [DOI] [PubMed] [Google Scholar]


