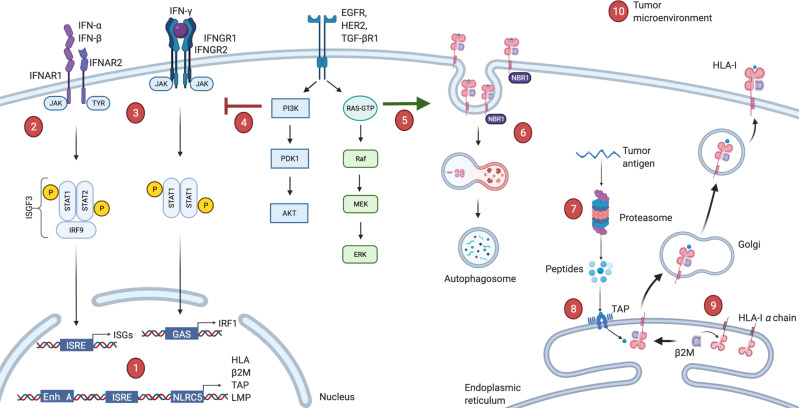
Figure 1.
Possible deficiencies in antigen presenting machinery. (1) Acquired mutations, transcriptional or post-transcriptional regulations in HLA or antigen presentation machinery (APM) genes or epigenetic modifications in their promoter regions. (2, 3) Defects in type-I or type-II interferon pathways, which are direct stimulators of HLA-I expression. (4) Aberrant activation of PI3K-Akt oncogenic pathway interferes with phosphorylation of STAT1 and hinders interferon mediated HLA-I expression. (5) Oncogenic BRAF mutation can drive internalization and endosomal degradation of surface HLA-I antigens. (6) Autophagy cargo receptor NBR1 protein can bind to HLA-I leads to autophagy-mediated degradation. (7) Defects in the proteasome components (LMP2, LMP9 or MECL-1, etc). (8) Defects in the peptide transport or ER peptide loading complex (TAP1/TAP2, ERp57, calnexin, calreticulin). (9) Downregulation of light chain β2M can lead to complete absence of HLA-I. (10) Microenvironmental conditions such as glucose deprivation, hypoxia, acidosis or excessive IL-10, TGF-β levels can also drive loss of HLA. β2M, β−2-microglobulin; ER, endoplasmic reticulum; HLA, human leucocyte antigen; IFNAR1, interferon alpha and beta receptor 1; IL-10, interleukin 10; ISRE, interferon stimulated response element; TAP1, transporter associated with antigen processing 1; TGF-β, transforming growth factor-β.