Abstract
During the nationwide state of emergency, many hospitals could not provide outpatient cardiac rehabilitation for cardiac disease patients in order to minimize coronavirus disease 2019 (COVID-19) incidence. The purpose of this study was to examine the trajectories of frailty, physical function and physical activity levels due to interruption and resumption of outpatient cardiac rehabilitation by COVID-19 in elderly heart failure patients. Fifteen patients who did not attend outpatient cardiac rehabilitation during the state of emergency but resumed it after the state of emergency were included. Frailty, physical function and physical activity levels were assessed with the Kihon checklist (KCL), various tests including short physical performance battery (SPPB), and life space assessment (LSA), respectively. Objective parameters were measured at three points; before and after the nationwide state of emergency in Japan and 3 months after resuming outpatient cardiac rehabilitation. The post-state of emergency KCL score was significantly higher than the pre-state of emergency score (P = 0.03), whereas there was no significant difference in KCL between post-state of emergency and 3 months after cardiac rehabilitation resumption. SPPB and LSA scores did not change significantly between pre- and post-state of emergency. The changes in LSA from post-state of emergency to 3 months after cardiac rehabilitation resumption tended to correlate with changes in KCL (r = −0.71, P = 0.11). We demonstrated that frailty status deteriorated significantly in elderly heart failure patients whose outpatient cardiac rehabilitation was interrupted due to COVID-19. In addition, the frailty status showed no significant improvement after 3 months of resuming cardiac rehabilitation.
Keywords: cardiac rehabilitation, coronavirus disease 2019, frailty, heart failure, physical function, physical activity
Introduction
In 2020, coronavirus disease 2019 (COVID-19) evolved into a worldwide pandemic, dramatically interrupting traditional face-to-face healthcare services. First COVID-19 case in Japan was reported on 16 January 2020, then, the incidence rate of infection gradually increased [1]. The government in Japan declared a nationwide state of emergency on 7 April 2020 and lifted it on 25 May 2020 [2]. The Japanese Association of Cardiac Rehabilitation announced a statement to consider interrupting outpatient cardiac rehabilitation in endemic areas of COVID-19 in Japan [3]. Therefore, many hospitals could not provide outpatient cardiac rehabilitation services for cardiac disease patients in order to minimize COVID-19 incidence in hospitals during the state of emergency. On the other hand, because the statement also described that outpatient cardiac rehabilitation can restart in non-epidemic area, some hospitals resumed outpatient cardiac rehabilitation after a state of emergency [3].
For elderly patients with cardiac disease who regularly participate in outpatient cardiac rehabilitation, interruption of cardiac rehabilitation due to COVID-19 impairs opportunities for regular and effective exercise therapy to improve physical function. A previous study reported that the total physical activity (physical activity) time was significantly decreased due to the COVID-19 pandemic in community-dwelling elderly Japanese adults [4]. Decreased physical function and physical activity are well known to associate with the presence of frailty [5]. The cessation of exercise is well known to bring about negative alterations of body composition and physical fitness, while retraining restores beneficial adaptations and improves them [6]. Therefore, it is important to assess how the interruption and resumption of outpatient cardiac rehabilitation affect frailty, physical function and physical activity levels. We hypothesized that interruption of outpatient cardiac rehabilitation among elderly heart failure patients would result in a higher degree of frailty and worse physical function, and the resumption of cardiac rehabilitation would result in improved status.
The aims of the study were to examine the trajectories of frailty, physical function and physical activity levels due to interruption and resumption of outpatient cardiac rehabilitation by COVID-19 in elderly heart failure patients.
Methods
This was a case series study of consecutive heart failure patients who underwent outpatient cardiac rehabilitation at the Omote-jyunkankika Cardiovascular Clinic in Shizuoka, Japan, between January 2020 and October 2020. We included 29 patients who did not attend outpatient cardiac rehabilitation during the state of emergency due to the desire or personal convenience of the patient or the patient’s family. Patients who were 64 years or younger or did not resume outpatient cardiac rehabilitation after the state of emergency were excluded. We complied with the principles of the 1975 Declaration of Helsinki regarding investigations in human subjects, and all patients were informed about the study and provided written consent.
Before the state of emergency, all patients were undergoing a standardized cardiac outpatient cardiac rehabilitation program according to the guidelines by the Japanese Circulation Society and the Japanese Association of Cardiac Rehabilitation [7, 8]. Patients attended a supervised outpatient cardiac rehabilitation program once or twice weekly and were also instructed to perform unsupervised moderate-intensity walking and resistance exercise more than two times per week. The supervised outpatient cardiac rehabilitation program was a combination of endurance and resistance training, including ergometer cycling or treadmill walking and machine-based strength training. Each session was 60 min, including warm-up and cool-down. For endurance training, the prescribed exercise was moderate in intensity (anaerobic threshold measured by cardiopulmonary exercise testing) and was for 30 min. For resistance training, patients used machines to perform 2–3 sets of a series of two upper-extremity and three lower-extremity exercises with an intensity of 40–60% of one-repetition maximum. As soon as the state of emergency was lifted, all patients resumed the same cardiac rehabilitation program. During all exercise programs, infection prevention measures were strictly implemented for the participants and staff, which included wearing masks, washing hands, social distancing and disinfecting equipment.
Clinical variables including age, sex, BMI, cause of heart failure, medications, comorbidities, biochemical data and echocardiographic data were obtained from medical records.
Objective variables in this study were frailty, physical function and physical activity levels. We assessed the frailty status with the Kihon checklist (KCL), which consists of 25 items that are divided into seven domains: lifestyle, motor abilities, nutrition, oral functions, seclusion, forgetfulness and depression [9]. On the basis of a previous study [10], we defined scores of 8 or higher as frail, 4–7 as pre-frail and 0–3 as robust. Physical functions were assessed with short physical performance battery (SPPB) [11], handgrip [12], 5 times sit-to-stand test (5STS) [13] and usual gait speed (UGS) [14], on the basis of previous methods. Physical activity level was measured using Life space assessment (LSA) [15,16]. LSA has been shown to correlate positively with higher step counts and physical activity time [17]. Objective parameters were assessed by physical therapists and measured at three time points; before and after the nationwide state of emergency in Japan, and 3 months after the resumption of outpatient cardiac rehabilitation (pre-state of emergency, post-state of emergency, and 3 months after cardiac rehabilitation resumption, respectively).
Data are presented as mean ± SD for continuous variables and percentages for categorical variables. Parameters of frailty, physical function, and physical activity levels were compared among the three points using Friedman’s test, and a holm post-hoc analysis was also conducted if indicated. To analyze the relationship between physical activity level and frailty status after the state of emergency, the changes in LSA and KCL from post-state of emergency to 3 months after cardiac rehabilitation resumption were calculated (Δ LSA and Δ KCL, respectively). The relationship between Δ LSA and Δ KCL was assessed using Spearman’s rank correlation coefficient. All analyses were carried out using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). In all analyses, two-tailed P values <0.05 were considered statistically significant.
Results
Of the 29 consecutive heart failure patients whose outpatient cardiac rehabilitation was interrupted, 14 were excluded because 7 were 64 years or younger and 7 did not resume cardiac rehabilitation even after the state of emergency, and a total of 15 were deemed eligible for this study. Thus, the final analysis comprised 15 patients. Table 1 shows the patient characteristics of these 15 patients.
Table 1.
Patient characteristics
| n | 15 |
|---|---|
| Age, years | 79.7 ± 6.0 |
| Women, n (%) | 11 (73.3) |
| BMI, kg/m2 | 23.7 ± 3.5 |
| NYHA | I:2/II:9/III:4/IV:0 |
| Cause of heart failure | |
| ICM, n (%) | 3 (20.0) |
| Valve, n (%) | 3 (20.0) |
| DCM, n (%) | 2 (13.3) |
| etc, n (%) | 8 (53.3) |
| Medications | |
| β blocker, n (%) | 11 (73.3) |
| ACEI or ARB, n (%) | 7 (46.7) |
| Diuretic, n (%) | 9 (60.0) |
| Comorbidities | |
| Hypertension, n (%) | 11 (73.3) |
| Diabetes mellitus, n (%) | 4 (26.6) |
| Dyslipidemia, n (%) | 6 (40.0) |
| CKD, n (%) | 7 (46.6) |
| Atrial fibrillation, n (%) | 8 (53.3) |
| Cognitive impairment, n (%) | 0 (0) |
| Biochemical data | |
| BNP, pg/dL | 195 ± 116 |
| eGFR, mL/min/1.73 m2 | 51.9 ± 19.1 |
| Echocardiography | |
| E/e’ | 14.9 ± 7.0 |
| LVEF, % | 53.2 ± 7.8 |
| Exercise capacity | |
| Peak VO2, mL/kg/min | 15.3 ± 5.0 |
Average ± SD.
ACEI, angiotensin-converting enzyme inhibitor; ARB, Angiotensin ll Receptor Blocker; BNP, brain natriuretic peptide; CKD, chronic kidney disease; DCM, dilated cardiomyopathy; E/e’, early mitral inflow velocity to mitral annular early diastolic velocity; eGFR, estimated glomerular filtration rate; ICM, ischemic cardiomyopathy; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association functional classification; peak VO2, peak oxygen uptake.
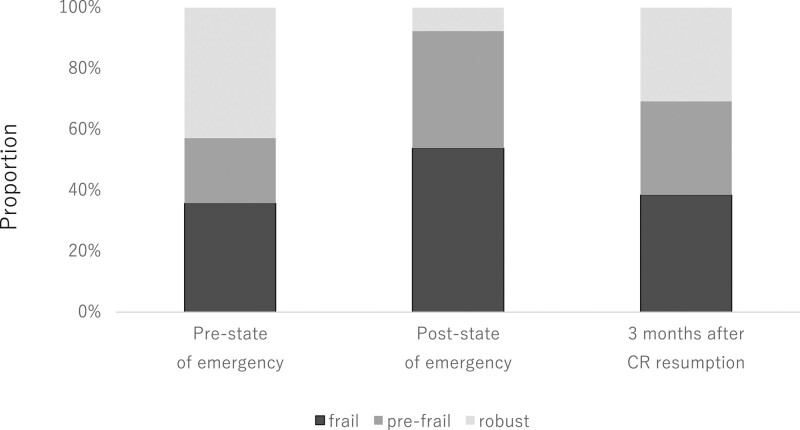
Trajectories of frailty, physical function, and physical activity levels are shown in Table 2. With the COVID-19 pandemic, outpatient cardiac rehabilitation was suddenly interrupted, and there was a shortage of medical staff to take objective measurements. Therefore, some patients were missing data on frailty, physical function or physical activity levels at one or more of the three time points: pre- and post-state of emergency and 3 months after cardiac rehabilitation resumption. Table 2 only includes patients who had data for all three time points, and the numbers of patients with available data are shown in parenthesis for each measurement. The post-state of emergency KCL score was significantly higher compared with the pre-state of the emergency score (P = 0.03). On the other hand, there was no significant difference in KCL between post-state of emergency and 3-months after cardiac rehabilitation resumption. SPPB tended to deteriorate gradually from the pre-state of emergency to 3 months after cardiac rehabilitation resumption, but the changes were NS. LSA tended to decrease from pre-state of emergency to post-state of emergency, but this change was also NS. Figure 1 shows the proportion of patients classified as frail, pre-frail and robust at three time points. Proportions of frail and prefrail patients were highest at post-state of emergency among the three time points.
Table 2.
Trajectories of frailty, physical function and physical activity levels
| Pre-state of emergency, A |
Post-state of emergency, B |
3-months after cardiac rehabilitation resumption, C |
ANOVA | Post hoc | |||
|---|---|---|---|---|---|---|---|
| A vs. B | B vs. C | C vs. A | |||||
| KCL, point (n = 13) | 4.8 ± 3.0 | 8.4 ± 4.6 | 6.1 ± 4.1 | 0.01 | 0.03 | — | 0.07 |
| SPPB, point (n = 12) | 11.4 ± 1.2 | 11.1 ± 1.6 | 10.9 ± 1.7 | 0.07 | — | — | — |
| Hand grip, kg (n = 15) | 20.8 ± 6.2 | 20.6 ± 5.6 | 19.9 ± 5.1 | 0.14 | — | — | — |
| 5STS, s (n = 12) | 8.1 ± 4.1 | 10.0 ± 4.1 | 8.9 ± 4.1 | 0.24 | — | — | — |
| UGS, m/s (n = 12) | 1.16 ± 0.30 | 1.12 ± 0.27 | 1.09 ± 0.27 | 0.67 | — | — | — |
| LSA, point (n = 9) | 84.1 ± 25.6 | 73.5 ± 32.3 | 75.7 ± 26.1 | 0.31 | — | — | — |
LSA, life space assessment; KCL, Kihon checklist; SPPB, short physical performance battery; 5STS, the 5 times sit-to-stand test; UGS, usual gait speed.
Fig. 1.
Proportion of frail, pre-frail, and robust patients at three time points (n = 13). CR, cardiac rehabilitation.
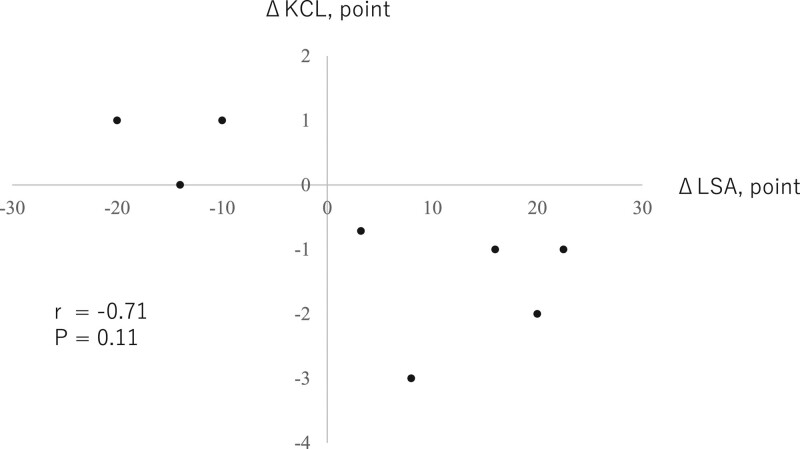
The relationship between ΔLSA and ΔKCL is shown in Fig. 2. The Δ LSA tended to correlate with Δ KCL negatively (r = −0.71, P = 0.11), showing a tendency for better frailty status with increased physical activity level.
Fig. 2.
Relationship between ΔLSA and ΔKCL from post-state of emergency to 3 months after cardiac rehabilitation resumption (n = 9). CR, cardiac rehabilitation; KCL, Kihon checklist; LSA, Life space assessment.
Discussions
The present study showed that KCL score as a parameter of frailty status deteriorated significantly in elderly heart failure patients whose outpatient cardiac rehabilitation was interrupted due to COVID-19. Although the frailty status showed no significant improvement after 3 months of resuming cardiac rehabilitation, there was a tendency for better frailty status among patients whose physical activity level increased.
In the present study, elderly heart failure patients whose cardiac rehabilitation was interrupted during the nationwide state of emergency tended to have lower post-state of emergency LSA scores, indicating lower physical activity. In addition, patients’ KCL scores, especially the seclusion domain scores, deteriorated significantly from pre- to post-state of emergency. These findings suggest that patients not only discontinued outpatient cardiac rehabilitation but also refrained from going outside due to COVID-19. Yamada et al. reported that total physical activity time per week significantly decreased by −26.5% due to the COVID-19 pandemic in community-dwelling older adults in Japan [4]. Decreased physical activity is a serious problem for elderly heart failure patients because low physical activity is associated with a higher risk of heart failure hospitalization and mortality [18]. Moreover, decreased physical activity is strongly associated with the presence of frailty [5]. Performing alternative exercise in their house is necessary to prevent decreasing physical activity and developing frailty in these patients in the COVID-19 pandemic.
There were no significant changes in physical function measured by SPPB, handgrip, 5STS and UGS between the pre- and post-state of emergency. In this study, the average period of outpatient cardiac rehabilitation interruption was about 2 months. This interruption period may have been short enough to not significantly affect physical function. A recent study with a longer interruption of outpatient cardiac rehabilitation due to the COVID-19 pandemic (median 77 days) affected the hemodynamic response and rating of perceived exertion during exercise in patients, especially those ≥75 years old [19]. When there is a long interruption of cardiac rehabilitation, whether it is due to COVID-19 or not, healthcare staff should pay close attention to patients’ physical function and abilities to perform activities of daily living.
All patients included in this study resumed outpatient cardiac rehabilitation after the nationwide state of emergency. However, 3-month cardiac rehabilitation did not significantly improve parameters of frailty and physical function. A previous study reported that exercise plus nutrition interventions for 6 months can help pre-frail or frail older adults to improve their frailty scores and physical performance [20]. Therefore, 3-months may have been too short to observe the effect of cardiac rehabilitation resumption on frailty status and physical function. On the other hand, the Δ LSA as a parameter of physical activity tended to correlate negatively with Δ KCL as a parameter of frailty. This suggests that increasing physical activity might be associated with improving frailty after a nationwide state of emergency. A recent study found that total time devoted to physical activity after the nationwide state of emergency did not recover to the baseline level in elderly who remained social inactive [21]. We should resolicit elderly heart failure patients for outpatient cardiac rehabilitation and promote physical activity at home if they continue to strictly follow the stay-at-home policy because staying at home may reduce the risk of COVID-19 infection, but decreased physical activity could increase the risk of heart failure hospitalization and mortality in the future.
The present study has several limitations. First, this study investigated patients at a single cardiology clinic; thus the generalizability of the results may be limited. Second, there were some missing data due to difficulty in obtaining all measurements in a pandemic. Thus, the final sample size was very small, and the probability of type II error may be high in this study. Third, as this study was a case series study, there was no control group, which makes it difficult to make clear conclusions. Finally, long-term effects of resuming outpatient cardiac rehabilitation after a nationwide state of emergency were unclear. Further studies need to clarify the long-term effects of the COVID-19 pandemic on the frailty status in these patients.
Conclusion
The present study demonstrated that frailty status might have worsened in elderly heart failure patients whose outpatient cardiac rehabilitation was interrupted during the COVID-19 pandemic. Resumption of cardiac rehabilitation and increasing physical activity might improve their frailty status after a nationwide state of emergency due to COVID-19, although 3 months was not sufficient to observe the effects of cardiac rehabilitation resumption.
Acknowledgements
We thank all staff of the Omote-jyunkankika Cardiovascular Clinic for facilitating this study. We also thank Fumi Nihei Green for editing the draft of this manuscript.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ministry of Health, Labour and Welfare of Japan. https://www.mhlw.go.jp/english/. [Accessed on 24 January 2021].
- 2.Office for Novel Coronavirus Disease Control, Cabinet Secretariat, Government of Japan. https://corona.go.jp/en/ [Accessed on 24 January 2021].
- 3.The Japanese Association of Cardiac Rehabilitation. Current status of cardiac rehabilitation for COVID-19. 2021. https://www.jacr.jp/web/wp-content/uploads/2020/07/jacr_covid19_2.pdf. [Accessed on 24 January 2021].
- 4.Yamada M, Kimura Y, Ishiyama D, Otobe Y, Suzuki M, Koyama S, et al. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: a cross-sectional online survey. J Nutr Health Aging. 2020; 24:948–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madan SA, Fida N, Barman P, Sims D, Shin J, Verghese J, et al. Frailty assessment in advanced heart failure. J Card Fail. 2016; 22:840–844. [DOI] [PubMed] [Google Scholar]
- 6.Tokmakidis SP, Touvra AM, Douda HT, Smilios I, Kotsa K, Volaklis KA. Training, detraining, and retraining effects on glycemic control and physical fitness in women with type 2 diabetes. Horm Metab Res. 2014; 46:974–979. [DOI] [PubMed] [Google Scholar]
- 7.Izawa H, Yoshida T, Ikegame T, Izawa KP, Ito Y, Okamura H, et al. ; Japanese Association of Cardiac Rehabilitation Standard Cardiac Rehabilitation Program Planning Committee. Standard Cardiac Rehabilitation Program for Heart Failure. Circ J. 2019; 83:2394–2398. [DOI] [PubMed] [Google Scholar]
- 8.JCS Joint Working Group. Guidelines for rehabilitation in patients with cardiovascular disease (JCS 2012). Circ J. 2014;78:2022–2093. [DOI] [PubMed] [Google Scholar]
- 9.Arai H, Satake S. English translation of the Kihon Checklist. Geriatr Gerontol Int. 2015; 15:518–519. [DOI] [PubMed] [Google Scholar]
- 10.Satake S, Senda K, Hong YJ, Miura H, Endo H, Sakurai T, et al. Validity of the Kihon Checklist for assessing frailty status. Geriatr Gerontol Int. 2016; 16:709–715. [DOI] [PubMed] [Google Scholar]
- 11.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995; 332:556–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kato M, Saitoh M, Kawamura T, Iwata K, Sakurada K, Okamura D, et al. Postoperative atrial fibrillation is associated with delayed early rehabilitation after heart valve surgery: a multicenter study. Phys Ther Res. 2019; 22:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baggetta R, D’Arrigo G, Torino C, ElHafeez SA, Manfredini F, Mallamaci F, et al. ; EXCITE Working group. Effect of a home based, low intensity, physical exercise program in older adults dialysis patients: a secondary analysis of the EXCITE trial. BMC Geriatr. 2018; 18:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pulignano G, Del Sindaco D, Di Lenarda A, Alunni G, Senni M, Tarantini L, et al. ; IMAGE-HF Study Investigators. Incremental value of gait speed in predicting prognosis of older adults with heart failure: insights from the IMAGE-HF study. JACC Heart Fail. 2016; 4:289–298. [DOI] [PubMed] [Google Scholar]
- 15.Shimada H, Sawyer P, Harada K, Kaneya S, Nihei K, Asakawa Y, et al. Predictive validity of the classification schema for functional mobility tests in instrumental activities of daily living decline among older adults. Arch Phys Med Rehabil. 2010; 91:241–246. [DOI] [PubMed] [Google Scholar]
- 16.Lo AX, Flood KL, Kennedy RE, Bittner V, Sawyer P, Allman RM, Brown CJ. The association between life-space and health care utilization in older adults with heart failure. J Gerontol A Biol Sci Med Sci. 2015; 70:1442–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai LT, Boyle E, Brønd JC, Kock G, Skjødt M, Hvid LG, Caserotti P. Associations between objectively measured physical activity, sedentary behaviour and time in bed among 75+ community-dwelling Danish older adults. BMC Geriatr. 2021; 21:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hegde SM, Claggett B, Shah AM, Lewis EF, Anand I, Shah SJ, et al. Physical activity and prognosis in the TOPCAT trial (treatment of preserved cardiac function heart failure with an aldosterone antagonist). Circulation. 2017; 136:982–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogura A, Izawa KP, Tawa H, Kureha F, Wada M, Harada N, et al. Impact of the COVID-19 pandemic on phase 2 cardiac rehabilitation patients in Japan. Heart Vessels. 2021; 29:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hsieh TJ, Su SC, Chen CW, Kang YW, Hu MH, Hsu LL, et al. Individualized home-based exercise and nutrition interventions improve frailty in older adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2019; 16:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamada M, Kimura Y, Ishiyama D, Otobe Y, Suzuki M, Koyama S, et al. Letter to the Editor: recovery of physical activity among older Japanese adults since the first wave of the COVID-19 pandemic. J Nutr Health Aging. 2020; 24:1036–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]