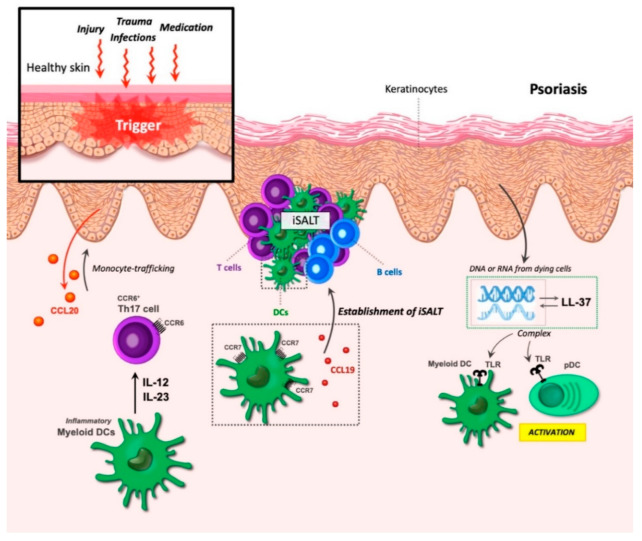
Figure 6.
Dendritic cells (DCs) in psoriasis. Psoriasis can be triggered by various factors, including trauma, infections, injury, and medication. The increased proliferation of keratinocytes leads to thickening of the epidermis, while the corneocytes fail to stack normally. During epidermal injury, keratinocytes secrete CCL20, leading to the recruitment of CCR6+ monocytes that, together with dermal DCs, are critical for psoriasis development. Inflammatory myeloid DCs produce the cytokines IL-12 and IL-23, resulting in the activation and expansion of Th17 cells and leading to an autoimmune response. The formation of inducible skin-associated lymphoid tissue (iSALT) structures occurs in psoriatic lesions. CCR7 and CCL19 partake in the establishment of these structures. iSALT primary contains CD3+ T cells, CD11c+ LAMP3/DC-LAMP+ DC, and, to a minor extent, CXCR5+ B cells. Keratinocytes produce the antimicrobial peptide LL-37, which can form complexes with DNA and RNA from dying cells. These complexes bind to toll-like receptors (TLRs) in myeloid DCs and pDCs leading to the activation of these cells.