Abstract
Background
The primary indication for using long-acting anesthetics in dentistry is extensive dental procedures that require pulpal anesthesia beyond 90 min and management of postoperative pain. Ropivacaine is an amide local anesthetic that is available at various concentrations with inherent vasoconstrictive properties at low concentrations. Ropivacaine has a 75% greater margin of safety than bupivacaine. Ropivacaine can be a good alternative to bupivacaine as a local anesthetic in dental implant surgery as it provides a longer duration of both pulpal and soft tissue anesthesia after mandibular nerve block and lowers CNS and cardiovascular toxicity. This study aimed to evaluate and compare the clinical efficacy of ropivacaine and lignocaine for implant surgery anesthesia.
Methods
Fifteen patients with bilateral edentulous sites indicated for implant placement were recruited for this study. Patients aged 20–60 years of both sexes were randomly recruited. Thirty implant placements were performed in the test and control groups using ropivacaine and lignocaine with adrenaline as local anesthetics, respectively.
Results
The results were analyzed statistically. The duration of anesthesia was significantly higher in the test group than in the control group. Ropivacaine was found to be superior to lignocaine in terms of the quality of anesthesia. The comparison of mean visual analog scale scores showed ropivacaine to have better anesthetic and analgesic effects than the control group.
Conclusion
Ropivacaine 0.75% provides a significantly longer duration of anesthesia than lignocaine 2% with adrenaline. Ropivacaine 0.75% decreased intraoperative and postoperative analgesia compared to lignocaine 2% with adrenaline. Hence, ropivacaine 0.75% can be used as an alternative to lignocaine in implant surgeries and other intraoral surgical procedures that require a longer duration of anesthesia and analgesia.
Keywords: Dental Implants, Lignocaine, Local Anesthesia, Receptor Theory, Ropivacaine
INTRODUCTION
The clinical application of local anesthetics marked the beginning of a new era in clinical dentistry, providing patient comfort and acceptance for extensive and invasive dental procedures. Local anesthetics (LA) provide reversible anesthesia and analgesia during surgery or for the management of other acute and chronic pain conditions that last for a few hours. Lignocaine is perhaps the most commonly used local anesthetic agent; it is used either in local or regional anesthesia or epidural or spinal blockade [1,2].
There are several local anesthetic solutions available, such as lidocaine, prilocaine, mepivacaine, bupivacaine, articaine, and ropivacaine. However, there has been continuous research to find the ideal local anesthetic solution with a prolonged duration of action, good postoperative analgesia, and low toxicity. The duration of action of a local anesthetic is dependent on two factors: protein binding and redistribution of the local anesthetic. Protein binding of the local anesthetic is an inherent drug characteristic with the longer duration of action indicating more protein binding of the drug. Furthermore, researchers have reported that the piperidine ring of cocaine and the xylidine component of lidocaine combine to form the pipecoloxylidine family of local anesthetics, including long-acting local anesthetics such as mepivacaine, bupivacaine, and ropivacaine. These drugs possess enhanced lipid solubility characteristics (making them extremely potent) and display an increased affinity for protein binding, which dramatically increases the duration of achievable anesthesia. This biochemical trait enhances the superiority of this group of drugs more than their short-acting analogs [3,4,5].
Long-acting local anesthetics not only produce localized sensory and motor anesthesia but also provide effective postoperative pain relief and analgesia. Therefore, there are two primary indications for the use of long-acting local anesthetics in dentistry: (1) extensive dental procedures requiring pulpal anesthesia of more than 90 min and (2) management of postoperative pain [2]. Long-acting local anesthetics include bupivacaine and etidocaine. Studies have reported that bupivacaine has higher tissue toxicity, neurotoxicity, and cardiotoxicity. Etidocaine is less cardiotoxic; however, increased intraoperative bleeding has been observed [6].
Ropivacaine is a local anesthetic of the amide-type that is chemically similar to bupivacaine and mepivacaine. It is available at various concentrations (0.75%, 0.5%, 0.375%, or 0.25%) and is said to have inherent vasoconstrictive properties at low concentrations. Ropivacaine has a 75% greater margin of safety than bupivacaine. The cardiovascular electrophysiology effects of ropivacaine were also found to be intermediate between those of lidocaine and bupivacaine. Ropivacaine can be used as a suitable local anesthetic without a vasoconstrictor for nerve block anesthesia in dental practice [7].
Ropivacaine is equivalent to bupivacaine in terms of potency and efficacy. Ropivacaine can be a good alternative to bupivacaine as a local anesthetic in dental implant surgery as it provides a longer duration of both pulpal and soft tissue anesthesia after mandibular nerve block and lowers CNS and cardiovascular toxicity [8]. Thus, this study aimed to compare the efficacy of ropivacaine with that of lignocaine with adrenaline for prolonged anesthesia and postoperative analgesia in implant surgery.
This study aimed to evaluate and compare the anesthetic efficacy of lignocaine 2% with 1:200,000 adrenaline and ropivacaine 0.75% during implant surgery, and to evaluate the influence of these anesthetic agents on postoperative pain perception after implant surgery.
METHODS
1. Ethical approval
The randomized, controlled, split-mouth study obtained ethical approval from the Institutional Review Board (RRDCHET / 04 / PERIO / 2018)
2. Sample size calculation
A sample size of 30 was calculated based on previous clinical studies of ropivacaine.
Considering a significance level of 5%, power of 80%, and error of 5%, a minimum of 28 samples was necessary.
3. Study samples and allocation
Each patient with a bilateral edentulous site was recruited for this study. The operator randomized the implant sites into A and B using a computer-generated random number table. Sequentially Numbered, Opaque, Sealed Envelope (SNOSE) technique was used to determine the sequence of allocation, that is, the site to be treated first. Site A and B were written on 15 pieces of paper each. These papers were kept in opaque sealed envelopes. Each participant was allowed to pick an envelope that was then opened by the investigator, and the treatment proceeded accordingly.
Fifteen healthy patients (ASA 1) with bilateral partial edentulism indicated for implant placement were randomly selected from both sexes (male and female) aged 20–60 years.
Group I (control group) comprised 15 implant surgeries in which lignocaine with adrenaline was used on one side.
Group II (test group) included 15 implant surgeries in which ropivacaine was used on the other side.
Patients with a history of allergic reactions to LA of amide group and sulfides, acute infections, medications such as monoamine oxidase inhibitors, tricyclic antidepressants, phenothiazine vasodepressor drugs, ergot-type oxytocic drugs, chronic smokers and alcoholics, and pregnant and lactating females were excluded from the study.
4. Evaluation of pain scores and other parameters
The numerical rating scale, visual analog scale (VAS), and verbal descriptive scale (VDS) were explained preoperatively and pain assessment was performed at the following time points: before anesthesia, after anesthesia, postoperatively at 1, 3, 6, 9, and 12 h immediately after surgery and on the first (D1) and second days (D2) postoperatively. The quality of anesthesia was assessed according to the patients' response during implant surgery [9]. All hemodynamic parameters, such as pulse rate, blood pressure, respiratory rate, oxygen saturation, and temperature were recorded.
5. Procedure
Patients were anesthetized using 3 mL of 2% lignocaine with adrenaline (Lignox 2% A, Indoco Remedies Ltd) in the control group and 3 mL of 0.75% plain ropivacaine (Ropin 0.75%, Neon Laboratories Ltd.) in the test group. Patients were informed about the drug and its possible complications, the surgical procedure that was performed, sequelae of the treatment, and possible complications of the procedure. Informed consent was obtained before the procedure. All surgical procedures were performed by the same surgeon. The choice of local anesthetic was randomized using the SNOSE technique and another local anesthetic was administered for the second side. Approximately 0.5 mL of 0.75% ropivacaine was intradermally infiltrated as a test solution. The implant placement in each patient using the control and test local anesthetic was performed at a gap of 7–10 days. Patients were asked to notify as soon as the lip and tongue became numb. The desired area was then anesthetized, and a standard surgical technique was used for implant placement. Mid-crestal incisions with no vertical releasing incisions were placed, and the incisions were extended mesially and distally to ensure accessibility. The incisions were extended to expose a minimum of 5 mm of the bone.
Vital parameters were monitored and pain score assessment was recorded before injecting the drugs, and the same parameters were recorded after injection at intervals of 30 min, 1, 3, 6, 9, and 12 h immediately after surgery and on the first (D1) and second days (D2) postoperatively.
Postoperative assessment
Patients were instructed to palpate the lower lip every 15 min to record the time at which numbness of the lip completely disappeared and there was a return to normal sensation (absence of pins-and-needles sensations). The time from the onset of anesthesia to the time when the numbness of the lip and tongue receded, as assessed by pricking, was taken as the duration of anesthesia. Patients were advised to refrain from analgesic intake until numbness of the lip and tongue receded. The duration of analgesia was recorded as the time from the start of numbness to when the patient first requested a dose of oral analgesic (50 mg BID for 3 days). Patients were instructed to rate the severity of their pain before anesthesia, after anesthesia, postoperatively at 1, 3, 6, 9, and 12 h immediately after surgery and on the first (D1) and second day (D2) postoperatively using VDS. The number of tablets used daily was considered for postoperative analgesia consumption: on the day of surgery (D1), the first day after surgery (D2), and the second day after surgery (D3).
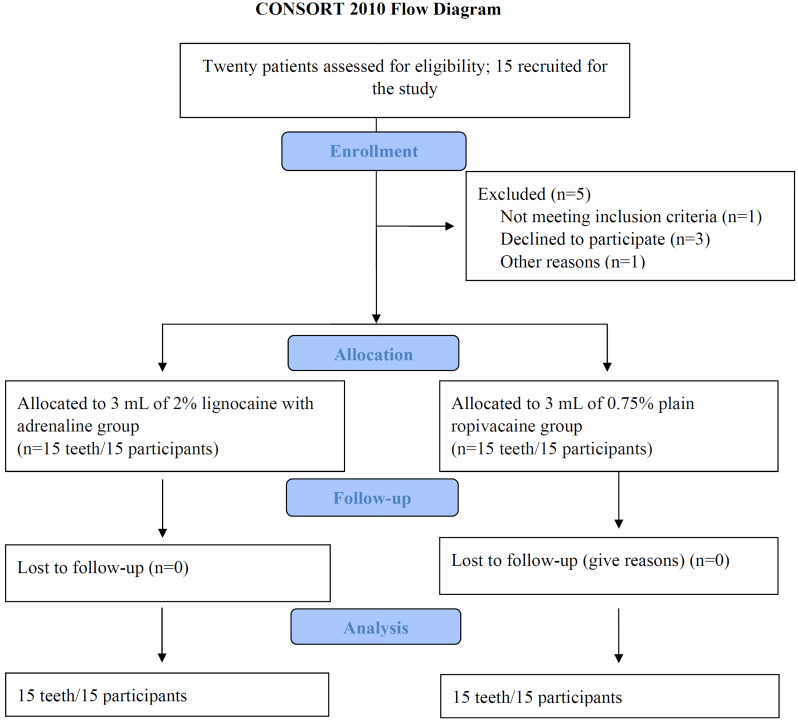
Postoperatively, patients were given a treatment regimen of antibiotics and analgesics and were instructed not to take any analgesics until the lip and tongue were no longer numb. The day after surgery, all patients were contacted telephonically and encouraged to complete their questionnaires and were reviewed for adverse events. The patients were recalled after 7 days for suture removal. The figure 1 shows the CONSORT diagram detailing patient recruitment and follow-up.
Fig. 1. The consort diagram detailing patient recruitment and follow-up.
6. Statistical analysis
Data were analyzed using statistical software (SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp). The student's paired t-test was used to compare the mean volume of LA, duration of anesthesia, and surgery between the test and control sites. McNemar's test was used to compare the quality of anesthesia between the test and control sites. The Wilcoxon signed-rank test was used to compare the mean pain scores between the test and control sites at different time intervals. Friedman's test was used to compare the mean pain scores at different time intervals in the test and control sites. The level of significance was set at a P value < 0.05.
RESULTS
The values obtained were subjected to statistical analysis following the assessment of the subjective and objective parameters.
1. General characteristics of the patient
Table 1 illustrates the distribution of demographic characteristics among study participants. The sample comprised 15 patients, with 11 men and four women, mean age of 28.5 years and a range of 15–54 yrs.
Table 1. Distribution of demographic characteristics among study subjects.
| Variables | Category | n | % |
|---|---|---|---|
| Age | <20 yrs | 4 | 26.7% |
| 21–30yrs | 7 | 46.7% | |
| >30yrs | 4 | 26.7% | |
| Mean | SD | ||
| Mean & SD | 28.5 | 11.5 | |
| Range | 15–54 | ||
| Gender | Males | 11 | 73.3% |
| Females | 4 | 26.7% |
2. Duration of anesthesia
Table 2 shows the comparison of mean LA volume in milliliters and duration of anesthesia and surgery in minutes between control and test sites using the Student's paired t-test. The duration of anesthesia was significantly greater (P < 0.001) in the ropivacaine group than in the lignocaine group, with a mean difference of 193.33.
Table 2. Comparison of mean LA volume (mL) and duration of anesthesia and surgery (min) between control and test sites using student paired t-test.
| Sites | N | Mean | SD | Mean diff | P-value | |
|---|---|---|---|---|---|---|
| LA Volume (mL) | Control | 15 | 3.17 | 0.31 | 0.00 | .. |
| Test | 15 | 3.17 | 0.31 | |||
| Quality of anesthesia | Control | 15 | 198.67 | 30.15 | 193.33 | < 0.001* |
| Test | 15 | 392.00 | 40.96 | |||
| Duration of surgery | Control | 15 | 70.33 | 18.47 | 0.67 | 0.33 |
| Test | 15 | 71.00 | 19.38 |
*P < 0.05 is statistically significant. LA, local anesthetics; SD, standard deviation.
3. Quality of anesthesia
Table 3 shows the quality of anesthesia obtained at the control and test sites, assessed using a rating scale. Considering the surgical sites treated, all sites in the ropivacaine group and only 70% in the lignocaine group reported a score of ≤ 3. The above observations suggest that ropivacaine is superior to lignocaine in terms of the quality of anesthesia.
Table 3. Comparison of quality of anesthesia between control and test sites using McNemar's test.
| Variables | Category | Control site | Test site | P-value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Quality of anesthesia | Score 2 | 3 | 20% | 9 | 60% | 0.001* |
| Score 3 | 9 | 60% | 6 | 40% | ||
| Score 4 | 2 | 13.3% | 0 | 0.0% | ||
| Score 5 | 1 | 6.7% | 0 | 0.0% | ||
*P < 0.05 is statistically significant.
4. Pain scores
Table 4 shows the comparison of VAS scores at different time intervals/points between two groups. The scores in the ropivacaine group were consistently lower than the lignocaine group. The difference in scores was statistically significant in favor of the ropivacaine group.
Table 4. Comparison of mean pain scores between control and test sites at different time intervals using Wilcoxon signed rank test.
| Time | Sites | N | Mean | SD | Mean diff | P-value |
|---|---|---|---|---|---|---|
| Baseline | Control | 15 | 3.27 | 0.59 | −0.07 | 0.56 |
| Test | 15 | 3.20 | 0.56 | |||
| 30 Mins | Control | 15 | 2.93 | 0.70 | −0.53 | 0.01* |
| Test | 15 | 2.40 | 0.51 | |||
| 1 Hour | Control | 15 | 2.40 | 0.63 | −0.67 | 0.008* |
| Test | 15 | 1.73 | 0.46 | |||
| 3 hours | Control | 15 | 2.13 | 0.64 | −0.80 | 0.006* |
| Test | 15 | 1.33 | 0.49 | |||
| 6 Hours | Control | 15 | 1.27 | 0.59 | −0.47 | 0.04* |
| Test | 15 | 0.80 | 0.56 | |||
| 12 Hours | Control | 15 | 0.80 | 0.68 | −0.47 | 0.04* |
| Test | 15 | 0.33 | 0.49 | |||
| 1 Day | Control | 15 | 0.27 | 0.46 | −0.20 | 0.18 |
| Test | 15 | 0.07 | 0.26 | |||
| 2 Day | Control | 15 | 0.00 | 0.00 | 0.00 | 1.00 |
| Test | 15 | 0.00 | 0.00 |
*P < 0.05 is statistically significant.
DISCUSSION
Ropivacaine is a long-duration local anesthetic agent (90 min/more pulpal anesthesia) that is extensively used in surgical procedures as well as in clinical dentistry. It has inherent vasoconstrictive properties, fewer cardiac and CNS adverse effects, and provides a concentration-dependent separation of sensory and motor effects [10]. Several studies have reported that sensory blockade is obtained at lower concentrations; therefore, ropivacaine at low concentrations may be suitable for providing postoperative analgesia [9,11,12].
In a randomized single-blind study, Bansal and Kumar in terms of quality of anesthesia had reported that ropivacaine 0.75% had a longer duration of action and effective diffusion property than that of lignocaine 2% with adrenaline 1:200000. Additionally, in our study, a comparison of VAS scores at different time points between the two groups demonstrated that the scores in the ropivacaine group were consistently lower than those in the lignocaine group [13]. Furthermore, the difference in the scores was statistically significant at all time points. Mishra et al. observed that ropivacaine demonstrates comparable efficacy as lignocaine with the added advantage of a longer duration of action and superior postoperative pain control. However, Ranjan et al. compared the efficacy of 0.75% ropivacaine and 2% lidocaine hydrochloride with 1:200000 adrenaline in the extraction of mandibular posterior teeth and concluded that even though ropivacaine had a long duration of action, they did not find any advantage of using 0.75% ropivacaine in pterygomandibular nerve block [14]. Emberg et al. determined the optimal concentration and volume of ropivacaine for dental anesthesia and concluded that ropivacaine had a remarkably long duration of both pulpal and soft tissue anesthesia, which could be favorable in reducing postoperative pain [6]. The study by Rajpari et al. compared the efficacy of 0.75% ropivacaine alone and 0.5% ropivacaine with 2% lignocaine along with 1:200,000 adrenaline and found that ropivacaine (0.75%, 0.5%) was more efficacious than 2% lignocaine demonstrating faster onset and longer duration of action. The onset of action of 0.75%/0.5% ropivacaine (101.84 ± 16.92 s/113.03 ± 12.77 s) was faster than LWA (Group I - 218 ± 21.51 s, Group II - 196.47 ± 26.27 s) [15]. Ropivacaine has a similar potency to bupivacaine at higher doses and with 1:200,000 epinephrine both demonstrating equivalent pharmacologic action [16].
In this study, ropivacaine was found to be safe, and no side effects or complications were reported. Ropivacaine has a moderate onset of action with a longer duration of anesthesia and potent postoperative analgesia than lignocaine with epinephrine.
In conclusion, ropivacaine, when used as a local anesthetic, demonstrated a longer duration of anesthesia and good postoperative analgesia. These observations suggest that ropivacaine is a potent and effective local anesthetic that can be used for clinical procedures of extended duration, as an alternative to lignocaine.
ACKNOWLEDGMENTS
The authors would like to thank Dr. S. Savita (Head, Department of Periodontology), Dr. Nimmi Janardhanan, and Dr. Alina Pauly for their support.
Footnotes
- Remya Nath Kalath: Conceptualization, Data curation, Formal analysis, Methodology, Writing — original draft.
- Rithesh Kulal: Conceptualization, Project administration, Software, Supervision, Visualization.
- Sharika Gopinath: Writing — review & editing.
FUNDING AND SPONSORSHIP: This research received no sponsorship or external funding.
CONFLICTS OF INTEREST: The authors declare no conflict of interest.
ETHICAL APPROVAL: This study was approved by the Institutional Review Board of Rajarajeswari Dental College and Hospital, Bangalore (RRDCHET/04/PERIO/2018)
DECLARATION OF PATIENT CONSENT: We certify that they have obtained consent forms before the procedure. In this form, the patient(s) has/have given their consent for clinical information, which is reported in the journal.The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CLINICAL TRIAL REGISTER: The study was approved by the Institutional Review Board Ethics Committee, and the study started only after obtaining ethical clearance. (RRDCHET/04/PERIO/2018).
References
- 1.Budenz AW. Local anesthetics in dentistry: then and now. J Calif Dent Assoc. 2003;31:388–396. [PubMed] [Google Scholar]
- 2.Gordon SM, Mishenko AV, Dionne RA. Long acting local anesthetics and perioperative pain management. Dent Clin North Am. 2010;54:611–620. doi: 10.1016/j.cden.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Paxton K, Thome DE. Efficacy of articaine formulations: quantitative reviews. Dent Clin North Am. 2010;54:643–653. doi: 10.1016/j.cden.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Mansour NA, Belasy, Marzook HA. Ropivacaine versus bupivacaine in postoperative pain control. J Biotechnol Biomater. 2012;2:137–144. [Google Scholar]
- 5.French J, Sharp LM. Local anaesthetics. Ann R Coll Surg Engl. 2012;94:76–80. doi: 10.1308/003588412X13171221502185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ernberg M, Kopp S. Ropivacaine for dental anesthesia: a dose-finding study. J Oral Maxillofac Surg. 2002;60:1004–1010. doi: 10.1053/joms.2002.34409. [DOI] [PubMed] [Google Scholar]
- 7.Budharapu A, Sinha R, Uppada UK, Subramanya Kumar AV. Ropivacaine: a new local anesthetic agent in maxillofacial surgery. Br J Oral Maxillofac Surg. 2015;53:451–454. doi: 10.1016/j.bjoms.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 8.Sisk AL. Long-acting local anesthetics in dentistry. Anesth Prog. 1992;39:53–60. [PMC free article] [PubMed] [Google Scholar]
- 9.El-Sharrawy E, Yagiela JA. Anesthetic efficacy of different ropivacaine concentrations for inferior alveolar nerve block. Anesth Prog. 2006;53:3–7. doi: 10.2344/0003-3006(2006)53[3:AEODRC]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuthiala G, Chaudhary G. Ropivacaine: a review of its pharmacology and clinical use. Indian J Anaesth. 2011;55:104–110. doi: 10.4103/0019-5049.79875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knudsen K, Beckman Suurküla M, Blomberg S, Sjövall J, Edvardsson N. Central nervous and cardiovascular effects of IV infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78:507–514. doi: 10.1093/bja/78.5.507. [DOI] [PubMed] [Google Scholar]
- 12.Brkovic BM, Zlatkovic M, Jovanovic D, Stojic D. Maxillary infiltration anesthesia by ropivacaine for upper third molar surgery. Int J Oral Maxillofac Surg. 2010;39:36–41. doi: 10.1016/j.ijom.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Bansal V, Kumar D, Mowar A, Bansal A. Comparison of ropivacaine 0.75% and lignocaine 2% with 1:200,000 adrenaline in dental extractions: single blind clinical trial. J Maxillofac Oral Surg. 2018;17:201–206. doi: 10.1007/s12663-016-0902-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ranjan R, Santhosh Kumar SN, Singh M. Comparison of efficacy of 0.75% ropivacaine and 2% lidocaine with 1:200,000 adrenaline in pain control in extraction of mandibular posterior teeth: a double-blind study. Indian J Dent Res. 2018;29:611–615. doi: 10.4103/ijdr.IJDR_150_17. [DOI] [PubMed] [Google Scholar]
- 15.Rajpari KN, Andrade NN, Nikalje T. Comparison of anesthetic efficacy of ropivacaine (0.75% & 0.5%) with 2% lignocaine with adrenaline (1:200000) in surgical extraction of bilateral mandibular 3rd molars using IANB:a prospective, randomized, single blind study. J Oral Biol Craniofac Res. 2021;11:263–268. doi: 10.1016/j.jobcr.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kennedy M, Reader A, Beck M, Weaver J. Anesthetic efficacy of ropivacaine in maxillary anterior infiltration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:406–412. doi: 10.1067/moe.2001.114000. [DOI] [PubMed] [Google Scholar]