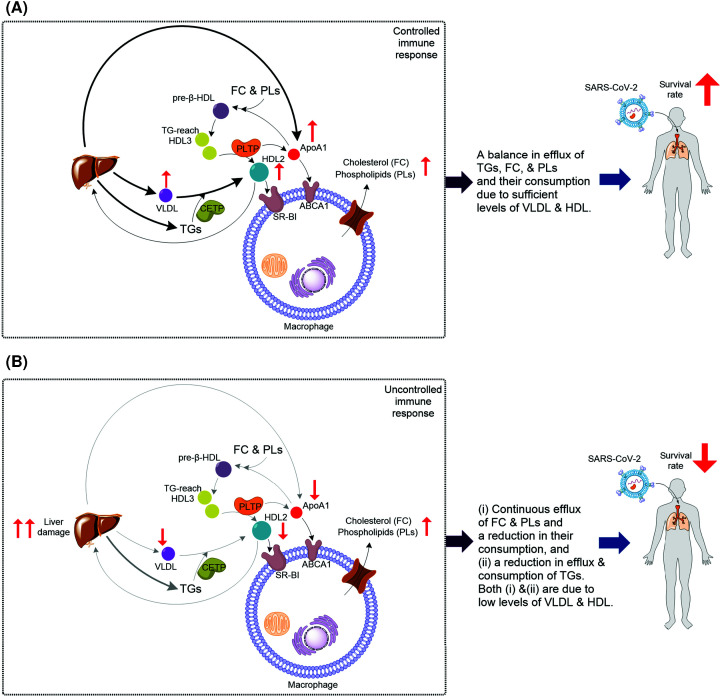
Figure 3. The postulated model linking cellular lipid metabolism to systemic lipid homeostasis and the outcomes of COVID-19 disease.
(A) When HDL level is sufficient, TGs, FC, and PLs produced by immune cells are consumed. Therefore, their blood levels are balanced leading to a controlled immune response and positive outcome. Enrichment of HDL3 with TGs enhances HDL conversion: fusion of two HDL3 by enzymatic activity of PLTP and formation of HDL2 with concomitant release of ApoA1. HDL2 is taken up by liver, and HDL2 and ApoA1 stimulate cholesterol efflux in macrophages. This response has both pro-inflammatory and anti-inflammatory effects. Thus, HDL regulates macrophage function to induce a controlled immune response increasing the survival rate of COVID-19 patients. (B) When there is not a sufficient level of HDL, which could be caused by severe liver damage or other factors, or when HDL is defective, e.g. due to aging, TGs, FC, and PE are produced by immune cells but are not consumed. This results in an uncontrolled immune response and negative outcome for patients. Both in (A,B) the change in level of TGs is the result of the net difference between efflux/production and consumption. Thus, in both (A,B) the level of TGs could increase. It is possible that the types of TGs involved in (A) are different than those involved in (B).