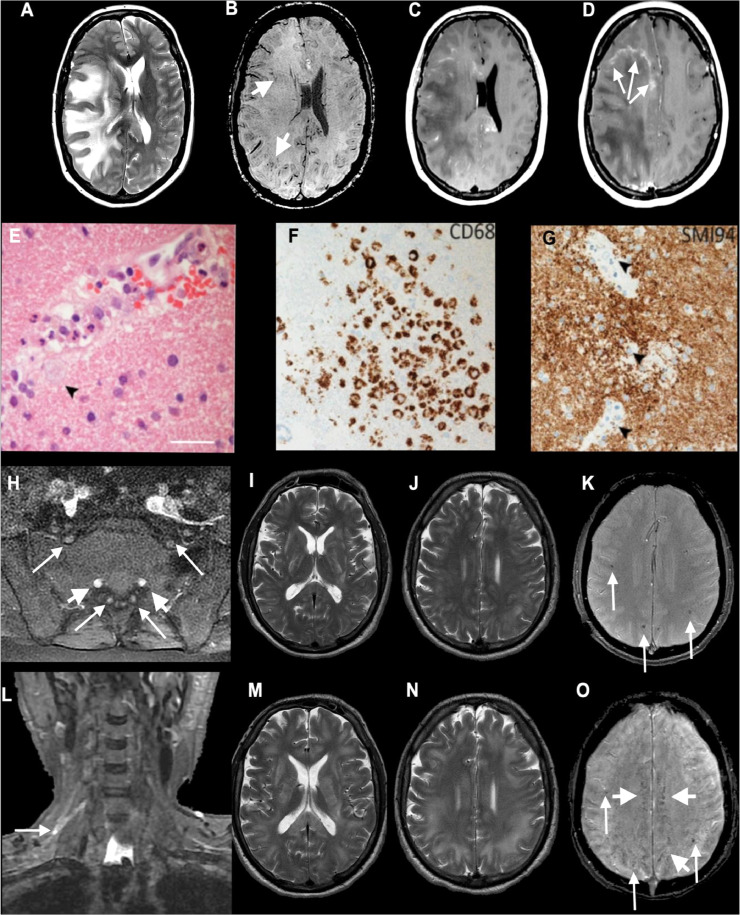
Fig. 2.
Axial MRI (A–D) and histopathology (E–G) from Patient 218, diagnosed with ADEM with a high aPS/PT IgG antibody titre (30.5 units/ml), and imaging (H–O) from Patient 218: axial T2-weighted (A), SWI (B), post-gadolinium (C and D) images show extensive confluent 'tumefactive' lesions involving the white matter of the right cerebral hemisphere, corpus callosum and corona radiata with mass effect, subfalcine herniation (A), clusters of prominent medullary veins (B, short arrows) and peripheral rim enhancement (D, arrows). (E) The white matter shows scattered small vessels with surrounding infiltrates of neutrophils and occasional foamy macrophages extending into the parenchyma (arrow). The endothelium is focally vacuolated but there is no evidence of vasculitis or fibrinoid vessel wall necrosis in any region. There were a few perivascular T cells in the white matter but the cortex appears normal (not shown). (F) CD68 stain confirms foci of foamy macrophages in the white matter, mainly surrounding small vessels. There was no significant microgliosis in the cortex (not shown). (G) Myelin basic protein stain (SMI94) shows areas with focal myelin debris in macrophages around vessels in the white matter (arrows) in keeping with early myelin breakdown. There is no evidence of axonal damage on neurofilament stain (not shown). Scale bars: E = 45 µm; F and G = 70 µm. (H–O) Patient 218; axial post-gadolinium fat-suppressed T1-weighted images (H) demonstrating pathologically enhancing extradural lumbosacral nerve roots (arrows). Note physiological enhancement of nerve root ganglia (short arrows). Coronal short tau inversion recovery (STIR) image (L) shows hyperintense signal abnormality of the upper trunk of the right brachial plexus (arrow). Initial axial T2 (I and J) and T2*-weighted images (K) show multifocal confluent T2 hyperintense lesions involving internal and external capsules, splenium of corpus callosum (I), and the juxtacortical and deep white matter (J), associated with microhaemorrhages (K, arrows). Follow-up T2-weighted images (M and N) show marked progression of the confluent T2 hyperintense lesions, which involve a large proportion of the juxtacortical and deep white matter, corpus callosum and internal and external capsules. The follow-up SWI image (O) demonstrates not only the previously seen microhaemorrhages (arrows) but also prominent medullary veins (short arrows). CT pulmonary angiogram excluded a pulmonary embolism but showed mild patchy ground-glass changes peripherally at the lung bases bilaterally characteristic of COVID-19 (not shown). REPRODUCED FROM PATERSON AND COLLEAGUES, BY PERMISSION OF OXFORD UNIVERSITY PRESS.