Figure 1.
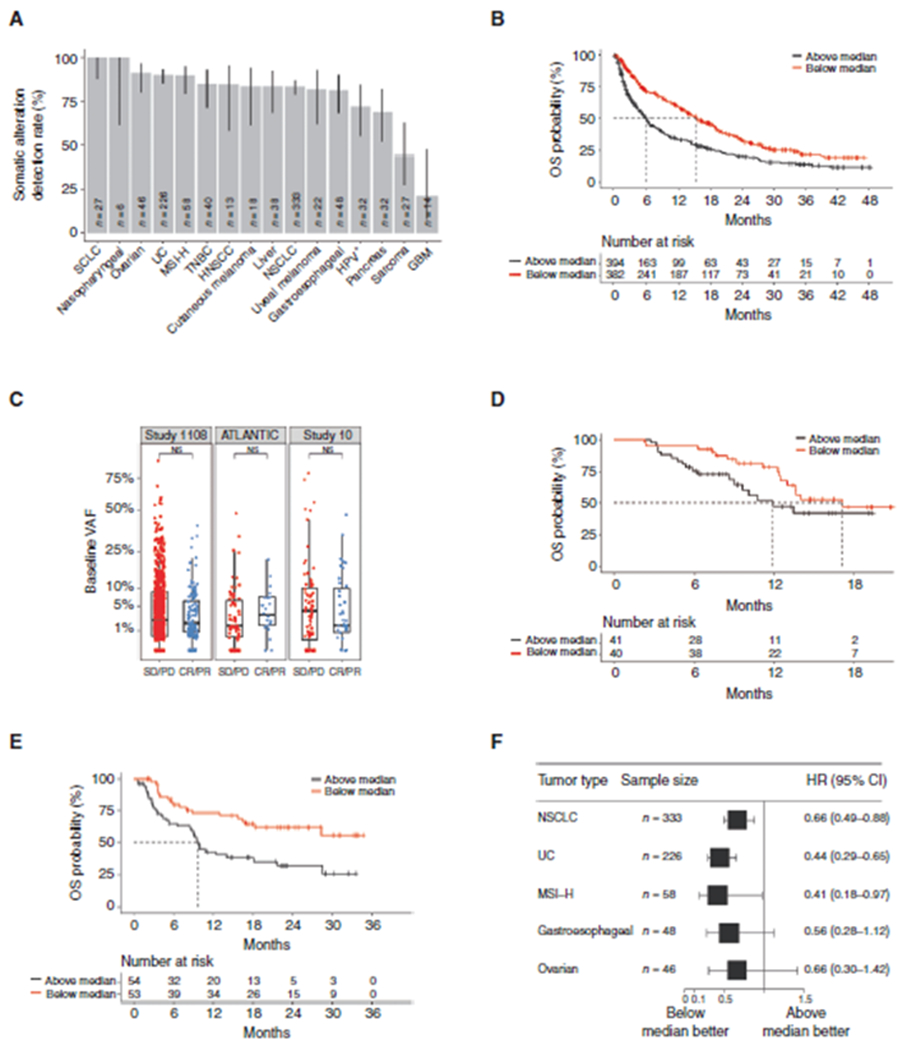
A, Somatic alteration detection rate by tumor type. Detection rate varied from 21.4% for patients with GBM to >95% for patients with SCLC and nasopharyngeal carcinoma. The error bars denote the 95% CI of detection rate for each tumor type given the sample sizes. B, Kaplan–Meier analysis of OS in the discovery cohort stratified by ≥median versus <median pretreatment VAF. For OS, unadjusted HR, 0.58; 95% CI, 0.49–0.69; P < 0.0001 and adjusted HR, 0.58; 95% CI, 0.48–0.7; P < 0.0001. C, Pretreatment VAF stratified by objective response (complete and partial responses vs. SD and progressive disease) in the discovery and validation cohorts. Pretreatment VAF was not significantly associated with response in any cohort. The horizontal bar represents the mean, the box represents the 25th and 75th percentiles, and whiskers ± 1.5 × interquartile range. Kaplan–Meier analysis of OS in the validation cohorts. D, Pretreatment VAF was not significantly associated with OS in ATLANTIC (HR, 0.58; 95% CI, 0.3–1.16; P = 0.12). E, Pretreatment VAF was significantly associated with OS in Study 10 (HR, 0.42; 95% CI, 0.24–0.74; P = 0.0019). F, Forest plot for OS by tumor type stratified by median pretreatment VAF using pooled data from the discovery cohort and both validation cohorts. CR, complete response; HNSCC, head and neck squamous cell carcinoma; HPV, human papillomavirus; PD, progressive disease; PR, partial response; TNBC, triple-negative breast cancer; UC, urothelial cancer.
