Abstract
Background
This factorial, assessor-blinded, randomized, and controlled study compared the effects of perturbation-induced step training (lateral waist-pulls), hip muscle strengthening, and their combination, on balance performance, muscle strength, and prospective falls among older adults.
Methods
Community-dwelling older adults were randomized to 4 training groups. Induced step training (IST, n = 25) involved 43 progressive perturbations. Hip abduction strengthening (HST, n = 25) utilized progressive resistance exercises. Combined training (CMB, n = 25) included IST and HST, and the control performed seated flexibility/relaxation exercises (SFR, n = 27). The training involved 36 sessions for a period of 12 weeks. The primary outcomes were the number of recovery steps and first step length, and maximum hip abduction torque. Fall frequency during 12 months after training was determined.
Results
Overall, the number of recovery steps was reduced by 31% and depended upon the first step type. IST and CMB increased the rate of more stable single lateral steps pre- and post-training than HST and SFR who used more multiple crossover and sequential steps. The improved rate of lateral steps for CMB exceeded the control (CMB/SFR rate ratio 2.68). First step length was unchanged, and HST alone increased hip torque by 25%. Relative to SFR, the fall rate ratios (falls/person/year) [95% confidence interval] were CMB 0.26 [0.07–0.90], IST 0.44 [0.18–1.08], and HST 0.30 (0.10–0.91).
Conclusions
Balance performance through stepping was best improved by combining perturbation and strength training and not strengthening alone. The interventions reduced future falls by 56%–74% over the control. Lateral balance perturbation training may enhance traditional programs for fall prevention.
Keywords: Aging, Falls, Hip strength, Lateral balance, Perturbation step training
Falls and their consequences are among the major problems in the medical care of older individuals (1,2). Impaired balance function is a consistently identified fall risk factor, and exercise training is a frequently used and effective fall prevention strategy in older adults (3,4). Previous randomized controlled studies of exercise effects on fall rates among older adults showed that the greatest improvements occurred with a high level of progressive challenges to balance performed regularly over a longer term, and that muscle strength training did not consistently reduce the risk of falls (5–7). Overall, the effects of conventional balance exercise training on fall reduction have generally been moderately successful with about a 20%–30% reduction (4).
Among the possible reasons why conventional exercise and balance training have shown modest effectiveness in preventing falls, may be that they rely mainly on performing instructed voluntary tasks that are executed relatively slowly with a fixed base of support (BoS). This approach lacks the task specificity required for counteracting many everyday falls involving external perturbations of balance (8,9). For example, sudden slips, trips, and jostles that disturb balance often require rapid reactive movements of the limbs such as stepping and reaching to grasp stable surfaces to alter the body center of mass (CoM)–BoS relationship and stabilize balance (10). External perturbations that evoke protective limb movements such as stepping resemble naturally occurring fall circumstances and are a potentially useful means for learning to prevent falling through perturbation-induced step training (11,12).
Accumulating research has indicated that perturbation-based balance training may be a favorable approach for enhancing protective balance reactions and preventing falls among older adults (11–26). Repeated postural perturbations promote sensorimotor adaptations in balance-stabilizing responses through trial-and-error practice involving reactive and predictive neuromotor control processes that can reduce the risk of falls (12,14–18,22). Such training has mainly utilized perturbations involving the sagittal direction that emphasize anterior–posterior balance recovery through adjustments in the CoM–BoS relationship (9,18,20,21). However, in view of the vulnerability to lateral imbalance among many older individuals (27–29), and the biomechanical differences between medial–lateral (ML) and forward–backward stepping (28,30), the effectiveness of lateral balance perturbation training on enhancing protective stepping and reducing the risk of falls in older adults remains to be determined. Furthermore, there are several daily circumstances where older people may need to take rapid ML protective steps including when turning suddenly to the side while standing or during postural transitions, changing direction of gait, stepping onto uneven terrain, being jostled in a crowd, or when yanked sideways by a pet on a leash.
Following lateral perturbations of balance, effective ML stepping is normally dependent upon high force, high speed usage of the hip abductor-adductor (AB-AD) muscles f (31,32). Among older adults, difficulties with ML stepping include the frequent use of unstable multiple crossover steps and sequential inter-limb recovery steps with collisions between the limbs. In contrast, younger adults more often use more secure single side steps (15,27,29,33). Problematic ML stepping patterns with aging are linked with changes in AB muscle performance and composition precipitating falls (34,35). Furthermore, differences in ML stepping patterns and low hip AB strength (joint torque) discriminate prospectively between fallers and non-fallers, confirming that these factors are common among older people who fall (36). While muscle strengthening exercise inconsistently reduces the risk of falls (4), such training has mainly involved the leg flexor and extensor muscles implicated in anterior–posterior balance control and not muscle groups more directly involved with lateral balance (6). Additionally, isolated muscle and joint strength training, without their functional use in balance-related contexts, is of limited utility because it lacks the important task specificity of exercise training (8,9).
To further address the foregoing issues, the primary aim of this study was to conduct a single-blind, randomized, and controlled trial with 4 training arms to compare the effects of perturbation-induced step training (lateral waist-pulls), hip abductor muscle strengthening, and their combination, on balance performance, muscle strength, and prospective falls among older adults. A sub-aim, not addressed here, was to assess the durability of training improvements in outcome measures after 3 months of no training. We hypothesized that, compared with the control group, the 3 training groups would demonstrate greater improvements in balance function and hip muscle strength, and lower fall rates, and that combined step training and muscle strengthening would result in the greatest improvements in outcomes.
Method
Study Design
This factorial, single-blinded, randomized, controlled trial was conducted at the University of Maryland School of Medicine, Baltimore, Maryland (January 25, 2012 to February 24, 2017). The study was approved by the Institutional Review Board at the University of Maryland School of Medicine and the Baltimore Veterans Affairs Medical Center and registered in the U.S. Clinical Trials Registry (ClinicalTrials.gov, NCT01370174). Four intervention groups received 12 weeks of either induced step training, hip muscle strength training, combined step and strength training, or flexibility and relaxation exercise training (Control). Balance and strength outcomes were assessed prior to training (baseline), immediately after 12 weeks of training, and after 3 months of no training. Fall frequency was tracked for 12 months after the training phase.
Participants
Recruitment, screening, and enrollment of generally healthy older adults aged 65 years or older were coordinated through the Biostatistics, Informatics and Translational Science Core of the University of Maryland Older Adult Independence Center and the Geriatric Assessment Clinic of the Gerontology Research, Education and Clinical Center of the Baltimore Veteran’s Administration Medical Center. Recruitment strategies used were the aging research registry, advertisement in a community aging newsletter, provider referrals, community outreach, contacts with senior centers and continuing care retirement communities, and through local and state agencies serving older adults.
Volunteers received a standard first-phase telephone screen using identified inclusion/exclusion criteria. Those passing the initial screen were examined by the medical team to confirm that they met the study criteria and to assure they could participate with no more than a minimal safety risk. Participant inclusion or exclusion was verified by the study geriatrician. At any point, participants were excluded who had conditions that compromised either their own safety or the researchers’ ability soundly to interpret the study results. Examples include (a) cognitive impairment (Mini-Mental Score Exam <24); (b) sedative use; (c) non-ambulatory; (d) any clinically significant functional impairment related to musculoskeletal, neurological, cardiopulmonary, metabolic, or other general medical problem; and (e) diabetes, renal, or liver disease by routine chemistry. Qualified individuals provided written informed consent prior to participation.
Outcome Measurements
Outcome measures were collected at 3 time points, pretraining, immediately post-training (within 3 days of completing training). Herein, we present comparisons between the performance at baseline and after 3 months of training. Testers and data analysts were blinded to participants’ group assignment. Data clinical balance assessments included the Berg Balance Scale, the Dynamic Gait Index, the Four-Square Step Test (FSST), and the Activities-specific Balance Confidence Scale. These performance measures were chosen based on their association with risk of falling, psychometric properties, and feasibility for use in clinical practice (37–41). An instrumented walkway system (GAITrite; CIR Systems Inc., Clifton, NJ) measured the spatial and temporal parameters of gait (42) while participants walked at their fastest comfortable speed during 3 trials. Outcomes included step length, step time, and walking speed. Overall physical and mental health was assessed by the 12-item Medical Outcomes Study Short-Form Health Survey (SF-12) (43). Maximum isokinetic hip AB joint torque was measured bilaterally (Biodex, Shirley, NY) at 60 deg/s through 0–30 degrees of motion with the hip initially positioned at 30° of AB while standing in a customized stabilization frame (44). The mean of 5 trials for each side was normalized to individuals’ weight and height.
Fall frequency was tracked for 12 months after training through monthly phone contacts and postcards (45). Falls were defined as “events that resulted in a person coming to rest unintentionally on the ground or other lower level, not as the result of a major intrinsic event or an overwhelming hazard” (1).
Protective stepping was evaluated using lateral postural perturbations applied via a motorized, waist-pull system (29). Participants wore a mobile safety harness and their usual walking shoes and stood with their feet shoulder-width apart on 2 separate force platforms (AMTI Inc., Newton, MA). A waist-belt was secured and separate cables were attached on each side to transmit ML perturbations. Participants held a light-weight baton with both hands in front of them to minimize motion capture marker obstruction. Perturbations in the right and left lateral directions were applied pseudo-randomly over 3 trials at 6 different pulling magnitudes (range 4.5–22.5 cm displacement, 9–54 cm/s velocity, 180–900 cm/s2 acceleration). The balance tolerance limit (BTL), defined as the minimum perturbation intensity at which the average number of recovery steps was greater than one, was determined (33,46,47).
Three-dimensional motion capture (Vicon, Oxford, UK) was used to collect kinematic data with 44 retro-reflective markers placed on body landmarks (sampling rate = 120 Hz, low-pass filtered at 6 Hz using a dual-pass fourth-order Butterworth filter). Ground reaction forces were recorded via the 2 force platforms beneath each foot at 600 Hz and low-pass filtered with a 10 Hz cutoff frequency.
Intervention Protocols
Participants were randomly assigned to 1 of the 4 training groups using blocked randomization, blocked on sex and fall risk, in an effort to assign an equal number of participants in each category to each of the training groups: (a) perturbation-induced step training (IST), (b) hip strength training (HST), (c) combination of induced stepping and hip strength training (CMB), and (d) control group consisting of standard flexibility and relaxation exercises (SFR). Laboratory-based training was conducted by trainers and lasted for 36 sessions conducted 3 times per week for a 12-week period. Participants unable to complete 34 sessions within 13 weeks were excluded from the analysis.
Training sessions began and ended with a 10-minute warm-up consisting of light repetitive stretching of major muscle groups or low-level aerobic stationary cycling or treadmill walking. Exercise intensities were determined by a licensed physical therapist (PT). Training was supervised by a PT or research assistant. IST involved lateral waist-pull perturbations using the same pulling system used for testing. Participants received 43 randomly presented waist-pull trials that induced stepping (2 directions × 20 pulls plus 3 catch trials with no perturbation applied) in blocks of 10 trials (excluding catch trials). Instructions were to “React naturally to the pull and try and maintain your balance. If you step, catch your balance with as few steps as possible.” While the perturbation testing consisted of the same 6 equally spaced pulling intensities for all participants, training programs were individually customized depending on their baseline BTL. The initial training intensity was set at 15% above the lowest of each participant’s left and right BTL levels. Progression consisted of 10% incremental increases in pull intensity, for example, 115%, 125%, and 135%, and occurred when a participant either (a) did not step 5 times within a 10-pull block or (b) executed 5 consecutive single steps within a 10-pull block. Several participants tolerated the maximum perturbation stimulus by averaging less than 1 response step at the highest puller perturbation level. If the maximum perturbation occurred without stepping, participants were further challenged by altering their BoS configuration.
The HST training involved 3 resistance exercises, each performed for 3 sets of 10 repetitions per set with 2–3 minutes rest between sets: (a) supine hip AB with resistance provided by elastic Thera-Bands of varying resistances (red = light to black = heavy). Progression occurred when a participant could perform all repetitions without excessive fatigue or compromised form. (b) Side-lying hip AB with cuff weights. Resistance was set at 35% of the side-lying 1 repetition maximum (1 RM) for set 1, 55% of 1 RM for set 2, and 75% of 1 RM for set 3. The side-lying 1 RM was reassessed every 2 weeks. (c) Standing isometric hip AB exerted against a wall-mounted force transducer with visual display. Isometric contractions were exerted for 6 seconds and for 5–10 repetitions as tolerated. Resistance exercise ceased when participants reported fatigue or when the maximum force decreased. For the side-lying exercise, the eccentric contraction phase was performed more slowly than the concentric phase.
CMB training involved both IST and HST protocols that were alternated for successive sessions. SFR training involved minimal-intensity flexibility and relaxation exercises performed while sitting with controlled rhythmic breathing (44). Following the standard warm-up, participants performed about 20 minutes of stretching exercises involving toe bending–straightening, ankle bending–straightening and rotation, knee bending–straightening and rotation, hand clenching, wrist bending–straightening and rotation, elbow bending–straightening, shoulder rotation, and bending–straightening and rotation of the trunk and neck. All exercises were repeated 10 times with each stretch held for about 15 seconds. Participants were asked not to perform the exercises outside of the scheduled training sessions during the study.
After 12 weeks of laboratory training, all participants performed a home-based maintenance program to enhance retention that combined step training and hip strengthening exercises. Hip strengthening included supine and standing hip AB with the elastic resistance Thera-band level the participant achieved when the training ended. Step training involved rapid voluntary stepping in 4 directions (forward, right, left, and back). Frequency and repetitions were the same as the training. Participants were encouraged to perform the program 2–3 times weekly. Maintenance training was recorded in a journal and a weekly follow-up phone call was made to each participant to assess compliance during the 3-month post-training period.
Statistical Analyses
All data were analyzed according to per-protocol analysis. Analysis of variance was used to compare the change (post–pre) value in our 3 training groups to the control group. The analyses were adjusted for the training group and, when there were significant differences between groups at baseline, for the baseline value. The comparisons of change in each group to the change in the control group were adjusted for multiple comparisons using the method of Dunnett.
To assess changes in the type of first step taken, Poisson regression was used to compute, in all 4 groups, the fraction of all steps, post and baseline, that were lateral steps. The analysis was adjusted for baseline values, time (post or pre), and a group × time interaction. Generalized estimating equations were used to account for the serial autocorrelation of multiple observations obtained from each participant. We used Quasi-likelihood Information Criteria to choose the best correlation structure from unstructured, compound symmetry, and first-order autoregression. Post hoc contrasts were used to determine (a) the change in the fraction of steps (rate ratio) that were lateral in each group (fraction post/fraction baseline); (b) compare the change in the fraction that was lateral in each group to the change in the control group (rate ratio, [fraction post groupx/fraction baseline groupx]/[fraction post SFR group/fraction baseline SFR group)], x = CMB, IST, HST; and (c) determine the group that showed the greatest improvement, that is, largest change comparing baseline rate of lateral steps to that seen after training (rate ratio, [fraction post groupx/fraction baseline group]/[fraction post groupy/fraction baseline groupy]), x = CMB, IST, HST, x ≠ y. Bonferroni’s method was used to adjust for multiple comparisons.
Poisson regression was used to compare the number of falls reported in each of the 3 intervention groups to the number of falls in the control group. The analyses were adjusted for the training group. The method of Dunnett was used to adjust for multiple comparisons. For all analyses, Cooks’ D, a diagnostic measure that examines the influence each observation has on the estimates produced by the model, was computed and reviewed.
Results
Participants and Characteristics
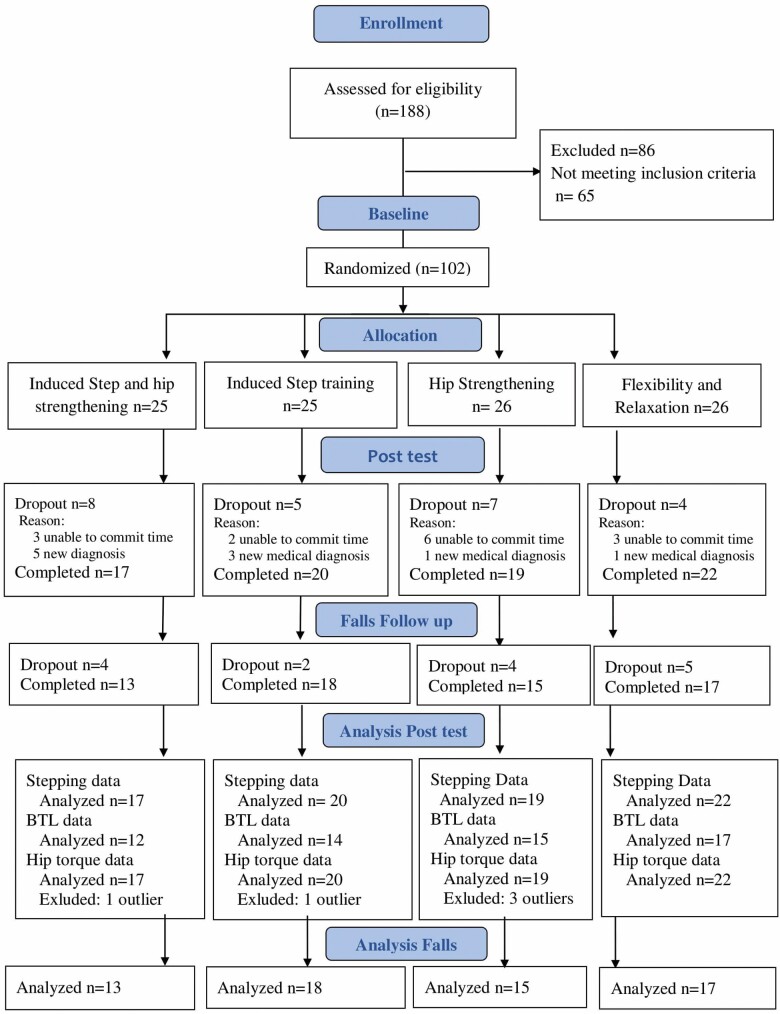
Eighty-six of the 188 older adults screened for eligibility were excluded due to inclusion or exclusion criteria (n = 65), and 21 people declined to participate or were lost to follow-up contact without being excluded. The remaining 102 participants were randomly assigned to each of the 4 intervention groups and participated in the initial baseline assessment. Between the baseline and immediate post-test, participant dropouts for CMB (n = 8), IST (n = 5), HST (n = 7), and SFR (n = 4) were due to either new medical diagnosis or an inability to commit to completing the study (Figure 1). The characteristics of the 78 participants included in the final analyses are presented in Table 1.
Figure 1.
Randomized controlled trial flow diagram.
Table 1.
Participant Characteristics
| CMB, n = 17 | IST, n = 20 | HST, n = 19 | SFR, n = 22 | |
|---|---|---|---|---|
| Age, years (mean ± SD) | 73.6 ± 6.5 | 73.7 ± 6.3 | 72.5 ± 7.2 | 70.8 ± 4.4 |
| Gender, % (male/female) | 58.8% males (10/7) | 40.0% males (8/12) | 36.8% males (7/12) | 27.3% males (6/16) |
| Height, m (mean ± SD) | 1.67 ± 0.033 | 1.67± 0.090 | 1.65 ± 0.088 | 1.62 ± 0.095 |
| Weight, kg (mean ± SD) | 76.1 ± 14.5 | 76.6 ± 17.8 | 72.8 ± 15.1 | 73.8 ± 14.6 |
| BMI, kg/m2 (mean ± SD) | 27.4 ± 4.0 | 28.4 ± 5.0 | 26.6 ± 4.5 | 28.0 ± 4.45 |
| Physical activity level, PASE | 124.4 ± 39.0 | 118.2 ± 43.4 | 130.0 ± 54.1 | 121.6 ± 61.2 |
Note: BMI = body mass index; CMB = combined induced step training and hip strengthening; HST = hip strengthening training; IST = induced step training; PASE = Physical Activity Scale for the Elderly; SFR = stretching, flexibility, and relaxation.
Balance Tolerance Limit
Although the BTL was evaluated for all participants pre- and post-training, post-training BTL values were missing for technical reasons in 20 participants distributed across the groups. Nevertheless, the BTL was significantly changed with training (Table 2, Omnibus p = .001) with CMB and IST groups showing a greater increase than the control group after adjustment for multiple comparisons (adjusted p = .0209 and .0122, respectively). The HST change in BTL was not different from that of the SFR (adjusted p = .9408).
Table 2.
Group Comparisons of Change in Balance Tolerance Limit (BTL), Four-Square Step Test, Maximum Hip Abduction (AB) Torque, and Prospective Falls Rate
| BTL* (units = levels of perturbation magnitude; 6 perturbation levels) | CMB (n = 12) | IST (n = 14) | HST (n = 15) | SFR (n = 17) |
|---|---|---|---|---|
| Baseline | 4.92 (0.34) | 4.78 (0.26) | 4.53 (0.26) | 4.50 (0.32) |
| Post-test | 6.25 (0.29) | 6.14 (0.21) | 4.83 (0.27) | 4.94 (0.27) |
| p = .021 | p = .012 | p = .941 | ||
| Max Hip AB Torque* (Nm/kg-m) | CMB (n = 17) | IST (n = 20) | HST (n = 19) | SFR (n = 22) |
| Baseline | 0.59 (0.04) | 0.49 (0.04) | 0.49 (0.02) | 0.523 (0.03) |
| Post-test | 0.62 (0.05) | 0.52 (0.03) | 0.61 (0.03) | 0.55 (0.03) |
| p = 1.000 | p = .984 | p = .017 | ||
| Four-Square Step Test* (seconds) | CMB (n = 17) | IST (n = 20) | HST (n = 19) | SFR (n = 22) |
| Baseline | 10.61 (0.73) | 10.08 (0.57) | 9.86 (0.53) | 9.28 (0.46) |
| Post-test | 8.80 (0.83) | 8.83 (0.42) | 8.72 (0.45) | 9.16 (0.51) |
| p = .007 | p = .080 | p = .136 | ||
| Prospective Falls** (#falls/person/year) | CMB (n = 13) | IST (n = 18) | HST (n = 15) | SFR (n = 17) |
| 0.23 (0.07–0.72) | 0.39 (0.19–0.82) | 0.27 (0.10–0.71) | 0.88 (0.53–1.16) | |
| p = .034/.097 | p = .074/.199 | p = .034/.095 |
Note: CMB = combined induced step training and hip strengthening; HST = hip strengthening training; IST = induced step training; SFR = stretching, flexibility, and relaxation.
*Mean (±standard error), p-value compared to control condition.
**Mean fall rate, 1-year post-training (95% CI), p-value compared to control condition/Dunnett’s adjusted p.
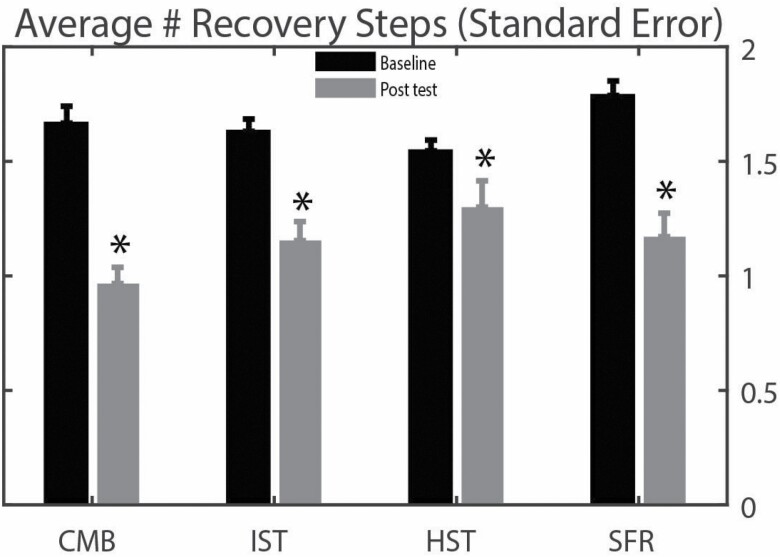
Number of Recovery Steps and Type of Steps
The main effect (p = .0332) indicated that the number of steps taken across all first step types was reduced with training (Figure 2). Between baseline and post-tests, the CMB group decreased the average number of recovery steps taken from 1.67 to 0.97, the IST group from 1.63 to 1.14, the HST group from 1.55 to 1.24, and the SFR group from 1.78 to 1.24. However, this outcome was of borderline significance when adjusted for group differences in the number of steps taken at baseline (Omnibus p = .0708). As shown in Figure 2, although differences between the intervention and control groups were not statistically different when adjusted for multiple comparisons, the CMB group showed a trend to reduce their average step count to less than 1 recovery step. Successive analyses where participants with large values of Cook’s D were inspected for exclusion did not change the observations.
Figure 2.
The mean (SE) number of recovery steps taken at baseline and post-training testing for the different intervention training groups. CMB = Combined induced step training (IST) and hip muscle strength training (HST) groups, SFR = seated stretching and flexibility exercise training control group. *Indicates that all conditions decreased the number of balance recovery steps following training, unadjusted p = .0332, adjusted for baseline differences p = .0708.
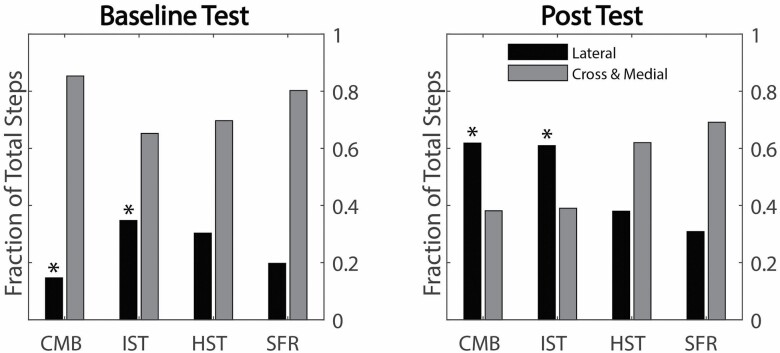
Because the type of first step performed is a major determinant of the number of steps taken (28,32,46), the change with training in the proportion of first steps that were more stabilizing single lateral protective steps was determined and expressed in relation to the number of unloaded limb steps (crossover and ML step sequence). All 4 groups (Figure 3) showed a trend to improve the fraction of steps that were lateral with training (rate ratio >1). After adjusting for multiple comparisons, the improvement was significant in both perturbation-based step training groups (CMB p = .0001, IST p = .0030) but not for the hip strength and control groups. The CMB group showed a larger improvement in rate of lateral steps than the other 3 groups, with rate ratios of CMB/IST = 2.39, p < .0031, CMB/HST = 3.34, p = .0001, and CMB/SFR = 2.68, p = .0014. After adjusting for 3 comparisons (CMB/SFR, IST/SFR, HST/SFR), only the CMB group showed a significantly larger increase in the rate of lateral steps than the control group, CMB/SFR rate ratio 2.68 adjusted p = .0041.
Figure 3.
The fraction of the total number of recovery steps taken at baseline and post-training testing which were either single lateral sidesteps or multiple crossover or sequential medial–lateral step types. *Indicates significant changes following training for CMB (p = .0001) and IST (p = .0030). Abbreviations are as indicated in Figure 2.
First Step Characteristics
Across the different first step types, there were no training-related changes in first step length (Omnibus p = .3823), step time (Omnibus p = .3836), or step speed (Omnibus p = .9205).
Hip AB Torque
There was a trend for maximum hip AB torque to increase with training but no significant overall group changes were found (Table 2, Omnibus p = .1145). However, successive analysis with Cook’s D identified observations that had an excessive influence on the data. These outlier observations involved 5 participants including 3 from the HST group and one each from the CMB and IST groups. After dropping these observations with large values of Cook’s D and reanalyzing the data, a stronger group effect was identified for AB torque (Omnibus p = .0225). Post hoc comparisons indicated that the change in AB torque was greater only for HST compared with SFR (adjusted p = .0061).
Clinical Balance and Mobility
The FSST (Table 2) was the only functional measure with a significant group effect (Omnibus p = .0177). The CMB group demonstrated improved performance time compared with SFR (adjusted p = .0068). The IST group also showed marginal improvement in performance time over SFR (adjusted p = .0816) indicating a tendency for both step training groups to show improvement in rapid voluntary stepping during the FSST.
Number of Falls During 1-Year Follow-Up
Data on the number of falls occurring during a 1-year period post-training (Table 2) were available for 63 participants: 13/24 (54%) in the CMB group, 18/25 (72%) in the IST group, 15/26 (58%) in the HST group, and 17/26 (65%) in the SFR group. There was no difference between the percentages of available fall data for each group (p < .59, Fisher’s Exact Test). The 1-year group fall rates (falls/person/year) were [estimate (95% CI)]: CMB 23% (7%–72%), IST 39% (19%–82%), HST 27% (10%–71%), and SFR 88% (53%–146%). The rate ratios comparing the rate in each of the intervention groups to the control group were CMB 0.26 (0.07–0.90) unadjusted p = .034, Dunnett’s adjusted p = .097, IST 0.44 (0.18–1.08) unadjusted p = .074, Dunnett’s adjusted p = .199, HST 0.30 (0.10–0.91) unadjusted p = .034, and Dunnett’s adjusted p = .095.
Adverse Events
Of the health-related occurrences during the study’s enrollment period, 16 events, CMB (n = 5), IST (n = 6), HST (n = 4), and SFR (n = 1), were possibly directly related to the intervention phase. Participant dropout reasons possibly related to training were CMB (knee pain, foot injury during fall at home), IST (knee pain, abdominal pressure/burping, swelling of scrotum, groin injury), HST (back pain, unresolved hypertension in 3 cases), and SFR (pain and tingling in neck/upper back). All the possible training-related cases were mild to moderate in severity.
Discussion
The main new findings of this study were that a 3-month program of ML perturbation-based step training was effective in improving lateral balance function through protective stepping and reducing fall risk and can be reinforced by hip AB muscle strengthening in community-living older adults. While both interventions, CMB and IST, involving a perturbation-based step training component increased their BTL and decreased their four-square step time compared with the control group, isolated hip strength training was not effective in improving protective stepping, balance tolerance, or functional outcomes. All 3 intervention groups showed significantly fewer falls than did control participants prior to Dunnett’s adjustment. After the adjustment, the improvements generally approached significance for CMB and HST (p < .10) and likely indicated insufficient statistical power.
The novel perturbation training effects on lateral balance function through ML protective stepping adds to and extends previous findings showing that perturbation-based approaches can effectively enhance balance and potentially reduce fall risk among community-living older adults (10–26). The findings also provide new information about the relative effectiveness of training highly challenging balance recovery actions by forcing adaptive changes in the CoM–BoS relationship, compared with more conventionally used isolated muscle strength training.
The magnitude level of lateral waist-pull where each participant took an average of more than 1 ML step to recover their balance for a given block of trials served as an index of their BTL (33,46,47). Compared with SFR, both perturbation training groups increased their BTL pre- and post-training indicating an enhanced ability to respond effectively to larger challenges to balance with step training. In contrast, the strength training group did not show a change in their BTL compared with the control group. It was expected that the step training groups would improve their BTL levels given that the balance training and assessment involved the same testing procedure and optimized the potential for the specificity of the training principle to be demonstrated (8,9). However, a similar improvement in the clinical balance outcome indicated the generalization of the training improvements to other balance performance contexts (26).
When the number of balance recovery steps was determined across the different first step types, a significant effect of training was observed. However, this difference was not significant when the analysis was adjusted for baseline differences in step number between the groups. When the first step type was next considered, robust changes in the predominant type and the associated number of recovery steps were identified for the CMB and IST groups compared with the control group. These results indicated a training-related conversion of first step type from more problematic multiple crossover and sequential stepping strategies prior to training, to more single lateral steps after training. While combining hip muscle strengthening with perturbation training further improved step type conversion and number of steps than step training alone, strength training alone did not improve these measures. Older individuals who repeatedly use more than 1 ML step to recover sideways balance are at increased risk of falling (29,33,36). Furthermore, multiple stepping recovery of balance is dependent on the type of first step executed following a perturbation (27,29,33,47). Whereas a single and more mechanically stabilizing lateral step with the limb ipsilateral to the direction of a fall is used more often by younger adults and older non-fallers, multiple stepping patterns initiated with the limb contralateral to the fall direction accompany generally less stabilizing crossover steps or an ML step sequence characteristic of aging and increased fall risk (47). The present findings indicated that both the number and types of recovery steps can be improved to enhance ML balance function through repeated exposure to progressively more challenging, but controlled, postural perturbations. These observations are consistent with previous reports indicating adaptive improvements in balance-stabilizing responses to perturbation training that emphasized reactions to slipping, tripping, and other BoS or CoM disturbances of balance (11–26).
As anticipated, compared with SFR, there were improvements in the maximum isokinetic hip AB torque for the HST group. There were no improvements in hip torque for the step training groups. Given the rapid nature of ML protective stepping, a resistance exercise training program emphasizing muscular power (force × velocity of contraction) may be a more effective approach for improving protective stepping and other balance-stabilizing actions requiring higher speeds of muscle contraction at different levels of force production than muscle strengthening without an emphasis on contractile speed (48,49).
The FSST was the only clinical balance and mobility outcome that showed training-related improvement over the control condition. Both CMB and IST groups improved their FSST performance while the HST group did not. These changes suggested that the improvements in balance performance derived from waist-pull testing and training may generalize to other challenges to balance. Moreover, the reactive and proactive balance control processes engaged by perturbation-based training appeared to have the potential to positively affect voluntary balance-recovery abilities such as rapid stepping during the FSST or reaction time stepping as previously reported (50–52).
While the issue of what effects of training are retained in the longer term is not addressed here, participants performed a 3-month post-training home-based maintenance exercise program emphasizing rapid stepping and hip muscle strengthening. Moreover, previous reports of healthy older adults showed retention of balance improvements after perturbation-based training for periods of 6–12 months (13,53) and found reductions in falls incidence at 1-year follow-up (16,17). Therefore, it is conceivable, or even likely, that the training effects we observed followed similar trends and lasted over the follow-up period.
Overall, there was a clear trend for the training groups to have lower prospective fall rates than the control group. While CMB showed the lowest fall rate among the training groups followed successively by HST and IST, the reduction for IST was not statistically significant (p = .072) and probably reflected lower statistical power. The significance of the group differences from SFR was reduced when adjusted for multiple comparisons. Nevertheless, the fall rate for the SFR group ranged from 2.3- to 3.8-fold greater than the intervention training groups. Furthermore, the tendency for the CMB group to have the lowest fall rate suggested that there may have been synergistic benefits of using perturbation and strengthening approaches together. The findings also resembled past observations indicating that the likelihood of falling can be reduced following even a single session of perturbation-based slip training among older adults, especially for those with a history of falls (12,54). While the present approach utilized a much larger training dosage than the other reports, it remains to be determined what the optimal dosage is for reducing the occurrence of falls (20,21). In addition, rather than to target such interventions at highly specific fall provoking mechanisms such as slipping or tripping, our approach used a more generalized circumstance requiring active changes in the CoM–BoS relationship to stabilize balance and prevent falling through disturbances applied near the CoM. It was reasoned that by repetitively engaging this fundamental balance-stabilizing requirement through trial-and-error practice, global adaptive changes in stepping ability would be an advantage over the specific recovery responses involved with slips, trips, and stumbles. While this postulation remains to be established, it would appear to have relevance for video surveillance findings of older adult care facility residents showing that incorrect weight shifting led to more falls than trips and slips combined (55). In this case, ML step training, as investigated here, emphasized inter-limb weight transfer control as an important element of successful lateral balance stability through protective stepping (32,49).
With respect to the clinical feasibility of applying the training approach used in the present study, the adverse events reported were mainly unrelated to the assessment and intervention protocols. Of the 14 mild to moderately severe adverse events resulting in dropouts during the interventions, 6 involved waist-pull perturbations which may or may not have been directly associated with the events. Therefore, the perturbation approach appeared to be generally well tolerated by healthy older adults. Concerning the accessibility of the waist-pull balance testing and training system, and other laboratory-based perturbation systems more generally, commercially available perturbation systems are currently available. Moreover, simpler clinical tools for balance assessment and training use a similar principle of applying pulling (pushing) through manual contact or restraint release balance perturbations through tether-release that can be readily implemented clinically (56,57).
Among the limitations of the study, the focus was on generally healthy community-living older adults who were functionally independent. Thus, the findings may not be directly applicable to other older adult populations with clinical conditions of aging that limit function and contribute to disability. There is also a risk of bias due to the per-protocol analysis used in analyzing data only for those who completed the study protocol, and to the relatively high rate of loss to follow-up for physical measures and falls. While falls can occur in virtually any direction, our training focused on stabilizing lateral balance that may have had less of an impact on other directions of falling. However, there is evidence suggesting that there may be a greater vulnerability to age-associated imbalance and falls in the frontal plane than in other directions of motion (27–29). Furthermore, it is also known that balance-recovery responses in the forward–backward directions involve an ML balance component (58,59). While our muscle resistance exercise intervention used conventional strength training, it is possible that focusing on muscular power training emphasizing contractile speed might have more optimally enhanced rapid and forceful postural actions that are often needed to stabilize balance and prevent falling (32,48,49).
In summary, this study corroborates and expands on previous reports indicating that postural perturbation-training can enhance balance function and reduce the risk of falls among community-living older adults. Furthermore, the results identified that lateral balance performance through protective stepping, BTL, and FSST were improved by perturbation-training but not by hip muscle strengthening alone as used in standard clinical care, though combining perturbation and strength training did result in further benefits. Overall, each of the interventions reduced the rate of falls in comparison with the control group. These findings have relevance for improving diminished weight-shifting ability accompanying ML stepping as a causal factor for falls that may serve as therapeutic targets for enhancing balance stability and preventing falls.
Acknowledgments
The contributions and assistance of Woei-Nan Bair, Alexandra Cirillo, Masahiro Fujimoto, Andrew Goldberg, Valentina Graci, Marjorie Hilliard, Andrea Howe, Hao-Yuan Hsiao, Mario Inacio, Les Katzel, Chen-Chieh Lin, Kathy Martinez, Michelle Prettyman, Kaitlin Riddle, Alice Ryan, Ozell Sanders, Kathy Simpson, Chieh-Ling Yang, and Tricia Young are gratefully acknowledged. The support of the Baltimore Veterans Affairs Medical Center, and the Geriatric Research, Education and Clinical Center is acknowledged with appreciation.
Funding
This work was supported by the National Institutes of Health (R01AG033607 to M.W.R), P30 AG028747; the National Institute on Disability and Rehabilitation Research (90AR50280 to M.W.R) and National Institute on Disability, Independent Living, and Rehabilitation Research (90AR5004 formerly H133P100014 to M.W.R.); and the Baltimore Veterans Affairs Medical Center, Geriatric Research, Education and Clinical Center support to B.A.B. and J.D.S.
Conflict of Interest
None declared.
Author Contributions
M.W.R. and J.D.S. were involved in the design of the study. R.A.C., V.G., J.A., and S.M.W. were responsible for data acquisition and intervention delivery. R.A.C. and V.G. were responsible for data entry. B.A.B. provided medical examination and oversight and determined participant suitability. V.G. coordinated the study. R.A.C. (masked) completed the data analysis. M.W.R. and J.D.S. developed the statistical analysis plan and J.D.S. managed statistical analyses. M.W.R., R.A.C., J.D.S., and V.G. drafted the manuscript. All authors were involved in interpreting the data and revising the manuscript.
References
- 1. World Health Organization. WHO Global Report on Falls Prevention in Older Age. WHO Press; 2007. [Google Scholar]
- 2. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-Based Injury Statistics Query and Reporting System (WISQARS). https://www.cdc.gov/injury/wisqars/index.html. Accessed November 30, 2010.
- 3. Gillespie LD, Robertson MC, Gillespie WJ, et al. . Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sherrington C, Fairhall NJ, Wallbank GK, et al. . Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:CD012424. doi: 10.1002/14651858.CD012424.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sherrington C, Tiedemann A, Fairhall N, Close JC, Lord SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull. 2011;22:78–83. doi: 10.1071/NB10056 [DOI] [PubMed] [Google Scholar]
- 6. Orr R. Contribution of muscle weakness to postural instability in the elderly. A systematic review. Eur J Phys Rehabil Med. 2010;46:183–220. [PubMed] [Google Scholar]
- 7. Ishigaki EY, Ramos LG, Carvalho ES, Lunardi AC. Effectiveness of muscle strengthening and description of protocols for preventing falls in the elderly: a systematic review. Braz J Phys Ther. 2014;18:111–118. doi: 10.1590/s1413-35552012005000148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grabiner MD, Crenshaw JR, Hurt CP, Rosenblatt NJ, Troy KL. Exercise-based fall prevention: can you be a bit more specific? Exerc Sport Sci Rev. 2014;42:161–168. doi: 10.1249/JES.0000000000000023 [DOI] [PubMed] [Google Scholar]
- 9. Kümmel J, Kramer A, Giboin LS, Gruber M. Specificity of balance training in healthy individuals: a systematic review and meta-analysis. Sports Med. 2016;46:1261–1271. doi: 10.1007/s40279-016-0515-z [DOI] [PubMed] [Google Scholar]
- 10. Maki BE, McIlroy WE. Change-in-support balance reactions in older persons: an emerging research area of clinical importance. Neurol Clin. 2005;23:751–83, vi. doi: 10.1016/j.ncl.2005.01.002 [DOI] [PubMed] [Google Scholar]
- 11. Mansfield A, Peters AL, Liu BA, Maki BE. A perturbation-based balance training program for older adults: study protocol for a randomised controlled trial. BMC Geriatr. 2007;7:12. doi: 10.1186/1471-2318-7-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pai YC, Bhatt T, Wang E, Espy D, Pavol MJ. Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Arch Phys Med Rehabil. 2010;91:452–459. doi: 10.1016/j.apmr.2009.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bhatt T, Yang F, Pai YC. Learning to resist gait-slip falls: long-term retention in community-dwelling older adults. Arch Phys Med Rehabil. 2012;93:557–564. doi: 10.1016/j.apmr.2011.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Parijat P, Lockhart TE. Effects of moveable platform training in preventing slip-induced falls in older adults. Ann Biomed Eng. 2012;40:1111–1121. doi: 10.1007/s10439-011-0477-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Carty CP, Cronin NJ, Lichtwark GA, Mills PM, Barrett RS. Mechanisms of adaptation from a multiple to a single step recovery strategy following repeated exposure to forward loss of balance in older adults. PLoS One. 2012;7:e33591. doi: 10.1371/journal.pone.0033591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosenblatt NJ, Marone J, Grabiner MD. Preventing trip-related falls by community-dwelling adults: a prospective study. J Am Geriatr Soc. 2013;61:1629–1631. doi: 10.1111/jgs.12428 [DOI] [PubMed] [Google Scholar]
- 17. Pai YC, Bhatt T, Yang F, Wang E. Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2014;69:1586–1594. doi: 10.1093/gerona/glu087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mansfield A, Wong JS, Bryce J, Knorr S, Patterson KK. Does perturbation-based balance training prevent falls? Systematic review and meta-analysis of preliminary randomized controlled trials. Phys Ther. 2015;95:700–709. doi: 10.2522/ptj.20140090 [DOI] [PubMed] [Google Scholar]
- 19. Dijkstra BW, Horak FB, Kamsma YP, Peterson DS. Older adults can improve compensatory stepping with repeated postural perturbations. Front Aging Neurosci. 2015;21(7):201. doi: 10.3389/fnagi.2015.00201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gerards MHG, McCrum C, Mansfield A, Meijer K. Perturbation-based balance training for falls reduction among older adults: current evidence and implications for clinical practice. Geriatr Gerontol Int. 2017;17:2294–2303. doi: 10.1111/ggi.13082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McCrum C, Gerards MHG, Karamanidis K, Zijlstra W, Meijer K. A systematic review of gait perturbation paradigms for improving reactive stepping responses and falls risk among healthy older adults. Eur Rev Aging Phys Act. 2017;14:3. doi: 10.1186/s11556-017-0173-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Krause A, Freyler K, Gollhofer A, et al. . Neuromuscular and kinematic adaptation in response to reactive balance training—a randomized controlled study regarding fall prevention. Front Physiol. 2018;9:1075. doi: 10.3389/fphys.2018.01075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wang Y, Bhatt T, Liu X, et al. . Can treadmill-slip perturbation training reduce immediate risk of over-ground-slip induced fall among community-dwelling older adults? J Biomech. 2019;84:58–66. doi: 10.1016/j.jbiomech.2018.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Okubo Y, Sturnieks DL, Brodie MA, Duran L, Lord SR. Effect of reactive balance training involving repeated slips and trips on balance recovery among older adults: a blinded randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2019;74:1489–1496. doi: 10.1093/gerona/glz021 [DOI] [PubMed] [Google Scholar]
- 25. Aviles J, Allin LJ, Alexander NB, Van Mullekom J, Nussbaum MA, Madigan ML. Comparison of treadmill trip-like training versus tai chi to improve reactive balance among independent older adult residents of senior housing: a pilot controlled trial. J Gerontol A Biol Sci Med Sci. 2019;74:1497–1503. doi: 10.1093/gerona/glz018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. König M, Epro G, Seeley J, Potthast W, Karamanidis K. Retention and generalizability of balance recovery response adaptations from trip perturbations across the adult life span. J Neurophysiol. 2019;122:1884–1893. doi: 10.1152/jn.00380.2019 [DOI] [PubMed] [Google Scholar]
- 27. Maki BE, Edmondstone MA, McIlroy WE. Age-related differences in laterally directed compensatory stepping behavior. J Gerontol A Biol Sci Med Sci. 2000;55:M270–M277. doi: 10.1093/gerona/55.5.m270 [DOI] [PubMed] [Google Scholar]
- 28. Rogers MW, Mille ML. Lateral stability and falls in older people. Exerc Sport Sci Rev. 2003;31:182–187. doi: 10.1097/00003677-200310000-00005 [DOI] [PubMed] [Google Scholar]
- 29. Mille ML, Johnson-Hilliard M, Martinez KM, Zhang Y, Edwards BJ, Rogers MW. One step, two steps, three steps more. Directional vulnerability to falls in community-dwelling older people. J Gerontol A Biol Sci Med Sci. 2013;68:1540–1548. doi: 10.1093/gerona/glt062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mansfield A, Maki BE. Are age-related impairments in change-in-support balance reactions dependent on the method of balance perturbation? J Biomech. 2009;42:1023–1031. doi: 10.1016/j.jbiomech.2009.02.007 [DOI] [PubMed] [Google Scholar]
- 31. Rietdyk S, Patla AE, Winter DA, Ishac MG, Little CE. Balance recovery from medio-lateral perturbations of the upper body during standing. J Biomech. 1999;32(11):1149–1158. doi: 10.1016/s0021-9290(99)00116-5 [DOI] [PubMed] [Google Scholar]
- 32. Inacio M, Creath R, Rogers MW. Effects of aging on hip abductor-adductor neuromuscular and mechanical performance during the weight transfer phase of lateral protective stepping. J Biomech. 2019;82:244–250. doi: 10.1016/j.jbiomech.2018.10.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bair WN, Prettyman MG, Beamer BA, Rogers MW. Kinematic and behavioral analyses of stepping strategies and risk for falls among community living older adults. Clin Biomech. 2016;36:74–82. doi: 10.1016/j.clinbiomech.2016.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Inacio M, Ryan AS, Bair WN, Prettyman M, Beamer BA, Rogers MW. Gluteal muscle composition differentiates fallers from non-fallers in community dwelling older adults. BMC Geriatr. 2014;14:37. doi: 10.1186/1471-2318-14-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Addison O, Inacio M, Bair WN, Beamer BA, Ryan AS, Rogers MW. Role of hip abductor muscle composition and torque in protective stepping for lateral balance recovery in older adults. Arch Phys Med Rehabil. 2017;98:1223–1228. doi: 10.1016/j.apmr.2016.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hilliard MJ, Martinez KM, Janssen I, et al. . Lateral balance factors predict future falls in community-living older adults. Arch Phys Med Rehabil. 2008;89:1708–1713. doi: 10.1016/j.apmr.2008.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Guralnik JM, Branch LG, Cummings SR, Curb JD. Physical performance measures in aging research. J Gerontol. 1989;44:M141–M146. doi: 10.1093/geronj/44.5.m141 [DOI] [PubMed] [Google Scholar]
- 38. Hayes KW, Johnson ME. Adult function—general performance tests. Arthritis Care Res. 2003;49(5S):S28–S42. [Google Scholar]
- 39. Shumway-Cook A, Gruber W, Baldwin M, Liao S. The effect of multidimensional exercises on balance, mobility, and fall risk in community-dwelling older adults. Phys Ther. 1997;77:46–57. doi: 10.1093/ptj/77.1.46 [DOI] [PubMed] [Google Scholar]
- 40. Moore M, Barker K. The validity and reliability of the four square step test in different adult populations: a systematic review. Syst Rev. 2017;6:187. doi: 10.1186/s13643-017-0577-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Myers AM, Powell LE, Maki BE, Holliday PJ, Brawley LR, Sherk W. Psychological indicators of balance confidence: relationship to actual and perceived abilities. J Gerontol A Biol Sci Med Sci. 1996;51:M37–M43. doi: 10.1093/gerona/51a.1.m37 [DOI] [PubMed] [Google Scholar]
- 42. Menz HB, Latt MD, Tiedemann A, Mun San Kwan M, Lord SR. Reliability of the GAITRite walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait Posture. 2004;20:20–25. doi: 10.1016/S0966-6362(03)00068-7 [DOI] [PubMed] [Google Scholar]
- 43. Resnick B, Parker R. Simplified scoring and psychometrics of the revised 12-item Short-Form Health Survey. Outcomes Manag Nurs Pract. 2001;5:161–166. [PubMed] [Google Scholar]
- 44. Johnson ME, Mille ML, Martinez KM, Crombie G, Rogers MW. Age-related changes in hip abductor and adductor joint torques. Arch Phys Med Rehabil. 2004;85:593–597. doi: 10.1016/j.apmr.2003.07.022 [DOI] [PubMed] [Google Scholar]
- 45. Lord SR, Tiedemann A, Chapman K, et al. . The effect of an individualized fall prevention program on fall risk and falls in older people: a randomized, controlled trial. J Am Geriatr Soc. 2005;53:1296–1304. doi: 10.1111/j.1532-5415.2005.53425.x [DOI] [PubMed] [Google Scholar]
- 46. Yungher DA, Morgia J, Bair WN, et al. . Short-term changes in protective stepping for lateral balance recovery in older adults. Clin Biomech (Bristol, Avon). 2012;27:151–157. doi: 10.1016/j.clinbiomech.2011.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Borrelli J, Creath RA, Pizac D, Hsiao H, Sanders OP, Rogers MW. Perturbation-evoked lateral steps in older adults: why take two steps when one will do? Clin Biomech (Bristol, Avon). 2019;63:41–47. doi: 10.1016/j.clinbiomech.2019.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Orr R, de Vos NJ, Singh NA, Ross DA, Stavrinos TM, Fiatarone-Singh MA. Power training improves balance in healthy older adults. J Gerontol A Biol Sci Med Sci. 2006;61:78–85. doi: 10.1093/gerona/61.1.78 [DOI] [PubMed] [Google Scholar]
- 49. Inacio M, Creath R, Rogers MW. Low-dose hip abductor-adductor power training improves neuromechanical weight-transfer control during lateral balance recovery in older adults. Clin Biomech (Bristol, Avon). 2018;60:127–133. doi: 10.1016/j.clinbiomech.2018.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rogers MW, Johnson ME, Martinez KM, Mille ML, Hedman LD. Step training improves the speed of voluntary step initiation in aging. J Gerontol A Biol Sci Med Sci. 2003;58:46–51. doi: 10.1093/gerona/58.1.m46 [DOI] [PubMed] [Google Scholar]
- 51. Gimmon Y, Shapiro A, Debi R, Snir Y, Melzer I. Unexpected perturbation training improves balance control and voluntary stepping times in older adults—a double blind randomized control trial. BMC Geriatr. 2016;16:58. doi: 10.1186/s12877-016-0223-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Okubo Y, Schoene D, Lord SR. Step training improves reaction time, gait and balance and reduces falls in older people: a systematic review and meta-analysis. Br J Sports Med. 2017;51:586–593. doi: 10.1136/bjsports-2015-095452 [DOI] [PubMed] [Google Scholar]
- 53. Pai YC, Yang F, Bhatt T, Wang E. Learning from laboratory induced falling: long-term motor retention among older adults. Age. 2014;36(3):1367–13760. doi: 10.1007/s11357-014-9640-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lee A, Bhatt T, Liu X, Wang Y, Pai YC. Can higher training practice dosage with treadmill slip-perturbation necessarily reduce risk of falls following overground slip? Gait Posture. 2018;61:387–392. doi: 10.1016/j.gaitpost.2018.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Robinovitch SN, Feldman F, Yang Y, et al. . Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet. 2013;381:47–54. doi: 10.1016/S0140-6736(12)61263-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Horak FB, Wrisley DM, Frank J. The Balance Evaluation Systems Test (BESTest) to differentiate balance deficits. Phys Ther. 2009;89:484–498. doi: 10.2522/ptj.20080071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. DePasquale L, Toscano L. The spring scale test: a reliable and valid tool for explaining fall history. J Geriatr Phys Ther. 2009;32:159–167. [PubMed] [Google Scholar]
- 58. McIlroy WE, Maki BE. Age-related changes in compensatory stepping in response to unpredictable perturbations. J Gerontol A Biol Sci Med Sci. 1996;51:M289–M296. doi: 10.1093/gerona/51a.6.m289 [DOI] [PubMed] [Google Scholar]
- 59. Rogers MW, Hedman LD, Johnson ME, Cain TD, Hanke TA. Lateral stability during forward-induced stepping for dynamic balance recovery in young and older adults. J Gerontol A Biol Sci Med Sci. 2001;56:M589–M594. doi: 10.1093/gerona/56.9.m589 [DOI] [PubMed] [Google Scholar]