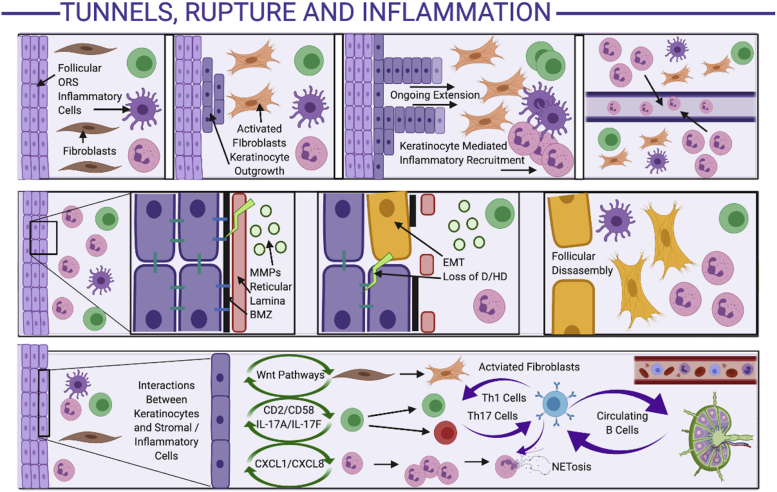
Fig 3.
Mechanisms of tunnel formation, follicular rupture, and perpetuation of inflammation in hidradenitis suppurativa. Development of tunnels (top panel): Inflammation adjacent to the follicular outer root sheath activates fibroblasts, with stromal-keratinocyte feedback resulting in keratinocyte outgrowth from the follicular wall. The ongoing keratinocyte outgrowth results in keratinocyte-mediated inflammatory cell recruitment, further amplifying the stromally mediated keratinocyte outgrowth in a positive-feedback loop. The inflammatory cells are attracted to the keratinocyte chemokine (CXCL1/CXCL8) gradient, resulting in migration into the lumen of the tunnels. Mechanisms of follicular rupture (middle panel): The inflammatory infiltrate is associated with high levels of matrix metalloproteinases, which degrade the reticular lamina. Keratinocyte-leucocyte cross talk activated epithelial-mesenchyme-transition mechanisms, leading to degradation of the basement membrane zone, loss of hemidesmosomes and desmosomes, and keratinocytes expressing mesenchymal cell surface markers (yellow keratinocytes). Eventually, the follicular wall is disassembled, replaced by mesenchymal cells and dense inflammatory infiltrates. Mechanisms of inflammatory amplification (bottom panel): Activated keratinocytes interact with inflammatory and stromal cells via various pathways to result in activated fibroblasts, T-helper cell types 1 and 17, and infiltration of dendritic cells and neutrophils. Circulating B cells (circulating to and from regional lymph nodes; far right of lower panel), activated by the high-interferon-mediated milieu, interact with multiple cell types to amplify existing inflammatory loops, as well as recirculate in the lymphatic and vascular system, contributing to systemic inflammation. D, Desmosome; HD, hemidesmosome; MMP, matrix metalloproteinase; ORS, outer root sheath.