Fig. 1.
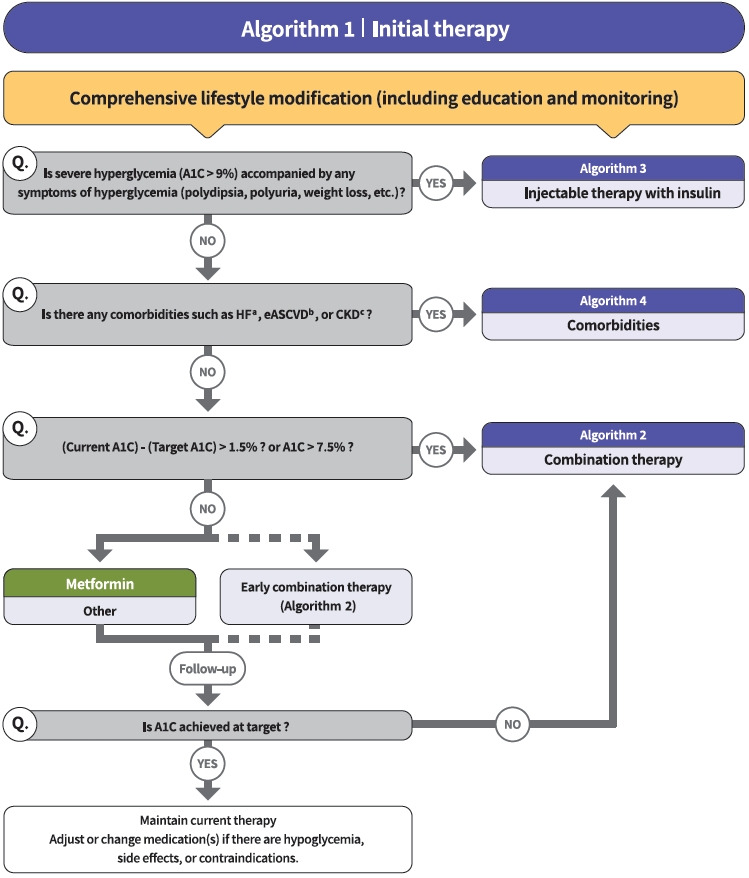
Treatment algorithm 1 (initial therapy) for patients with type 2 diabetes mellitus (T2DM). The algorithm stratifies the strategy of glycemic control for T2DM based on initial glycosylated hemoglobin (A1C) levels and underlying comorbidities. For newly diagnosed T2DM, begin with comprehensive lifestyle modification (LSM) at the time of diagnosis and monitor continuously. If the initial severe hyperglycemia (A1C level >9.0%) is accompanied by symptoms of hyperglycemia (polydipsia, polyuria, weight loss, etc.), insulin treatment should be prioritized (algorithm 3). If heart failure (HF), established atherosclerotic cardiovascular disease (eASCVD), or chronic kidney disease (CKD) are present, follow algorithm 4. If glycemic target is not achieved within 3 months after LSM, then glucose-lowering agent should be initiated promptly. If the current A1C is 1.5% higher than that of the target A1C or the current A1C level is >7.5%, follow algorithm 2 (combination therapy). If the A1C level is 7.5% or less, metformin monotherapy is recommended as a first-line therapy. However, if there are contraindications or intolerable side effects related to metformin use, a different class of medications can be considered. Instead of metformin monotherapy, early combination therapy could be considered to reduce the risk of failure of glycemic control in some patients with newly diagnosed T2DM. eGFR, estimated glomerular filtration rate. aParticularly HF with reduced ejection fraction (HFrEF, clinical diagnosis of HF and left ventricular ejection fraction ≤40%), bA history of an acute coronary syndrome or myocardial infarction, stable or unstable angina, coronary heart disease with or without revascularization, other arterial revascularization, stroke, or peripheral artery disease assumed to be atherosclerotic in origin, ceGFR <60 mL/min/1.73 m2 or urine albumin creatinine ratio ≥30 mg/g.
