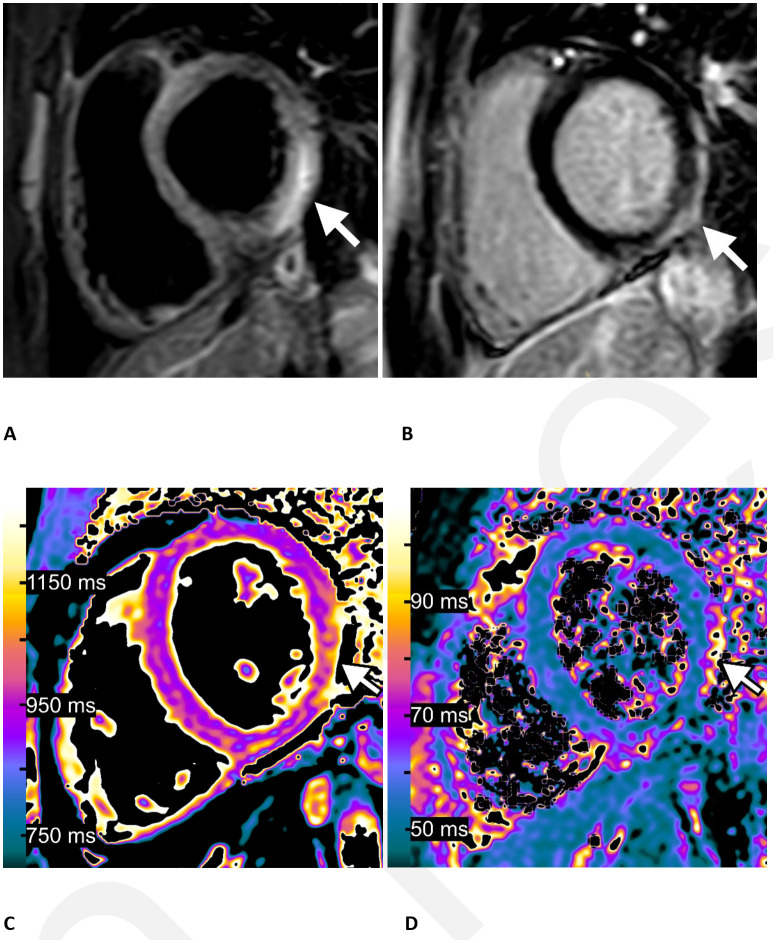
A healthy 15-year-old boy received his second vaccination dose (BNT162b2-mRNA SARS-CoV2, Biontech/Pfizer) and the following day he developed fever, myalgia, and intermittent tachycardia. At presentation to the hospital his electrocardiogram showed ST-segment elevation in the left precordial leads. High-sensitive cardiac troponin and C-reactive protein levels were elevated. Serology tests for cardiotropic viruses were negative. Transthoracic echocardiography showed normal myocardial function without wall motion abnormalities. Cardiac MRI at 1.5 T showed a normal left ventricular size, normal left ventricular ejection fraction and a small pericardial effusion. T2-weighted short TI inversion recovery sequences displayed focal myocardial edema involving the lateral wall, most emphasized in the basal inferolateral segment (Figure). Corresponding subepicardial enhancement was detected by late gadolinium enhancement imaging indicating inflammatory necrosis (Figure). Quantitative myocardial mapping parameters were elevated confirming the qualitatively assessed findings (Figure). The 2018 Lake Louise criteria for the diagnosis of an acute myocarditis were fulfilled (1, 2). Furthermore, vaccine-induced unilateral axillary lymphadenopathy was also observed. Due to the close temporal relation between the mRNA SARS-CoV-2 vaccination and the onset of symptoms (one day), vaccine-induced hypersensitivity myocarditis was clinical diagnosis. The patient was discharged in stable condition after 7 days of hospitalization.
Myocarditis following COVID-19 vaccination in a 15-year-old boy. One day after receiving his second vaccination dose he developed fever, myalgia, and intermittent tachycardia: (A) T2-weighted short TI inversion recovery MRI at 1.5 T in short-axis view shows focal high signal intensities at the basal lateral and inferior wall (arrow) indicating myocardial edema. (B) Late gadolinium enhancement imaging in short-axis view displays corresponding linear subepicardial enhancement (arrow) indicating inflammatory myocardial necrosis. (C) T1 mapping and (D) T2 mapping in short-axis view show elevated T1 and T2 relaxation times at the mid ventricular lateral and inferolateral wall (arrows), indicating acute myocardial injury (focal T1 relaxation time: 1165 ms, focal T2 relaxation time: 70 ms; institution-specific cutoff values for acute myocarditis: T1 global: ≥1000 ms, T2 global: ≥55.9 ms).
Cardiac MRI characteristics of vaccine-induced hypersensitivity myocarditis are similar to other virus-induced causes of myocarditis. This case shows that clinicians should be aware of vaccine-induced myocarditis as a possible adverse effect in children with thoracic/cardiovascular complaints after mRNA SARS-CoV-2-vaccination. As children are now scheduled to be vaccinated in many countries, cases of vaccine-induced myocarditis will have been noted in association with mRNA vaccines. Vaccine associated myocarditis is rare, but more common in the young population, especially in males (e.g. incidence of 40.6 cases per million second doses of mRNA SARS-CoV-2 vaccinations in males aged 12-29 years (3)). Clinical course is typically self-limited (4).
Footnotes
Funding: A. I. was supported by a grant from the BONFOR research program (2021-1A-05). The funders had no influence on manuscript preparation as well as the decision to publish.
References
- 1. Ferreira VM , Schulz-Menger J , Holmvang G , et al . Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations . J Am Coll Cardiol 2018. ; 72 ( 24 ): 3158 – 3176 . 10.1016/j.jacc.2018.09.072 . [DOI] [PubMed] [Google Scholar]
- 2.Luetkens JA, Faron A, Isaak A, et al. Comparison of Original and 2018 Lake Louise Criteria for Diagnosis of Acute Myocarditis: Results of a Validation Cohort. Radiol Cardiothorac Imaging 2019;1(3):e190010. 10.1148/ryct.2019190010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gargano JW , Wallace M , Hadler SC , et al . Use of mRNA COVID-19 Vaccine After Reports of Myocarditis Among Vaccine Recipients: Update from the Advisory Committee on Immunization Practices - United States, June 2021 . MMWR Morb Mortal Wkly Rep 2021. ; 70 ( 27 ): 977 – 982 . 10.15585/mmwr.mm7027e2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Montgomery J , Ryan M , Engler R , et al . Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military . JAMA Cardiol 2021. . 10.1001/jamacardio.2021.2833 . [DOI] [PMC free article] [PubMed] [Google Scholar]