Figure 1.
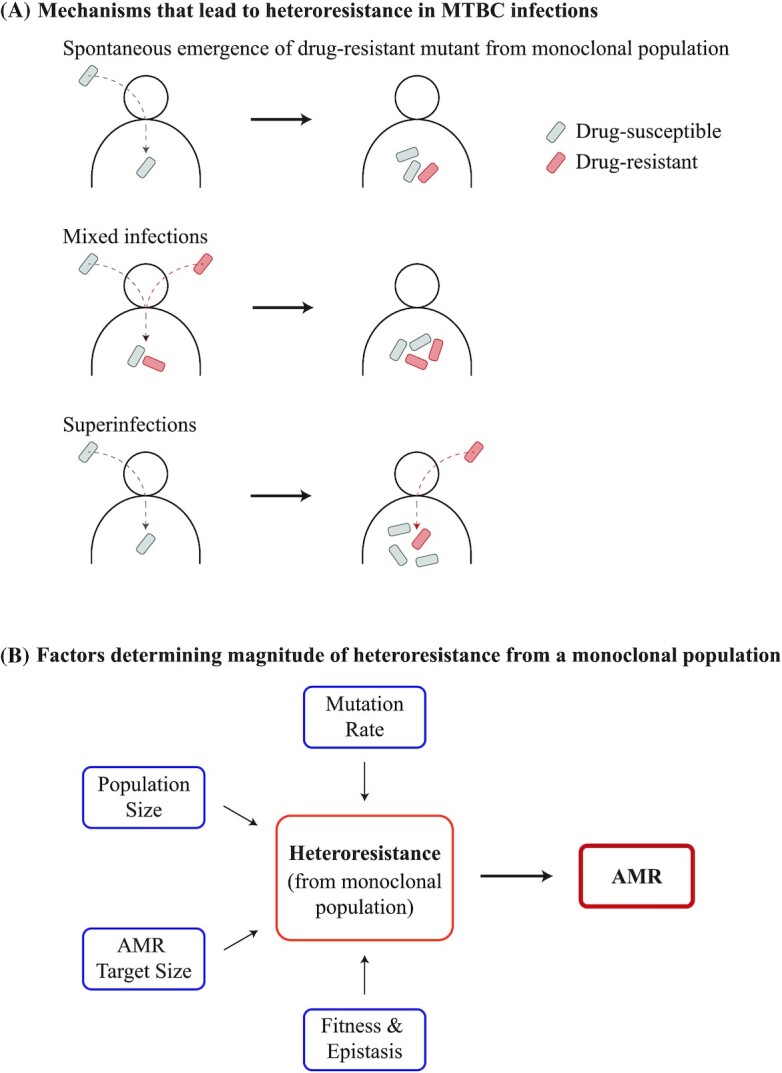
Heteroresistance in the MTBC. (A) Heteroresistance may manifest through three different mechanisms in MTBC infections. Firstly, an AMR mutant may spontaneously emerge from an initially monoclonal and drug-susceptible population. ‘Polyclonal’ infections may also lead to heteroresistance in the MTBC, of which two types are relevant: mixed infections and superinfections. Mixed infections are defined as when two different clones infect a given patient simultaneously. In contrast, superinfections are defined as an infection with one clone following a previous infection with a different clone that was not cleared over time. Polyclonal infections can lead to heteroresistance if one of the clones was an AMR mutant and the other was drug-susceptible. Of particular note, heteroresistance from gene duplications may be common in other bacteria, but have so far not been reported in the MTBC. (B) Bacterial mutation rates, bacterial population sizes, the number of mutations that can confer the AMR phenotype (i.e. AMR target sizes), and the fitness of AMR mutations can all determine the emergence and magnitude of heteroresistance from an initially drug-susceptible, monoclonal MTBC population, which in turn modulates the prevalence of AMR.
