Figure 4.
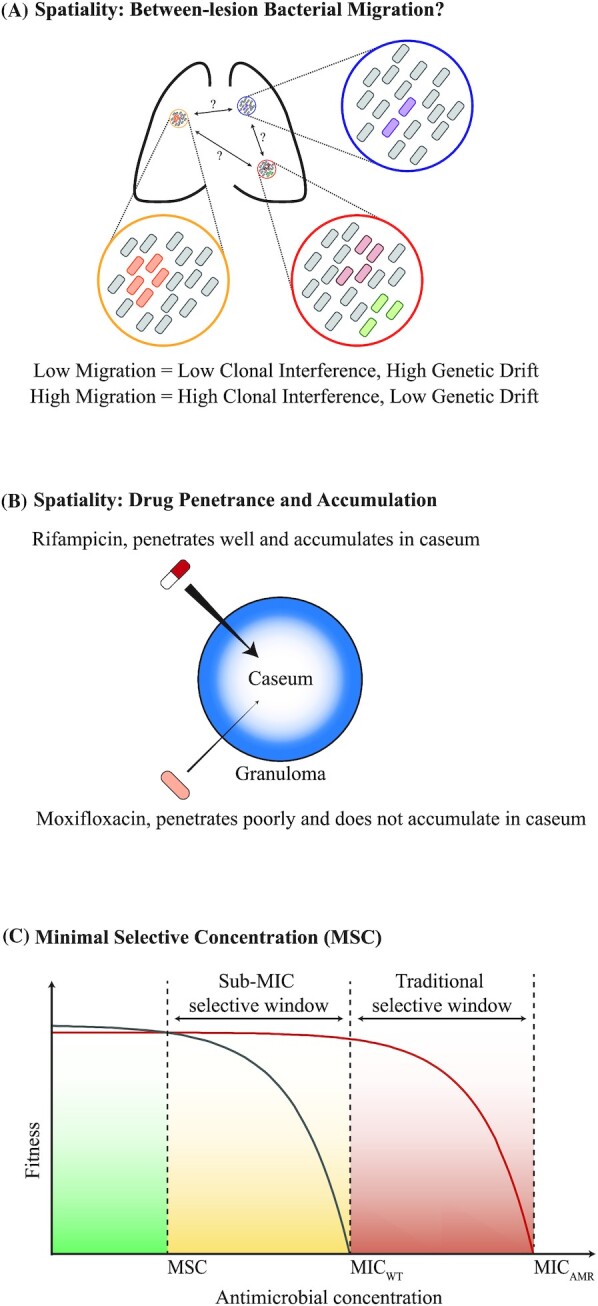
Role of spatiality in the within-host evolution of AMR in the MTBC. (A) MTBC populations may be spatially-segregated in different lung lesions. Not much is known about population mixing between these different lesions. Hypothetically, low levels of migration between lesions would lead to lower clonal interference, a greater role of genetic drift and higher regional genetic differentiation. In contrast, high migration levels would lead to greater clonal interference, smaller role of genetic drift and less regional differentiation. (B) Different anti-TB drugs have been shown to have different capacities to penetrate into granulomas. This leads to differences in antimicrobial accumulation rates and total concentrations in the caseum, the lesion site that generally harbors the greatest density of MTBC bacilli. General pharmacokinetics of rifampicin and moxifloxacin are shown here as an example. (C) Concept of minimal selective concentration (MSC). Antimicrobials impose a dose-dependent reduction in the fitness of bacteria. Although the fitness of drug-susceptible wild-type and AMR mutants is zero at their respective minimum inhibitory concentrations (MICWT and MICAMR = minimum inhibitory concentration for wild-type and AMR mutant, respectively), the fitness reduction occurs earlier in the antimicrobial concentration gradient for wild-type compared to the AMR mutant. The antimicrobial concentration where the fitness of the wild-type is equivalent to the fitness of the AMR mutant is the MSC. The MSC can be well below MICWT, and antimicrobial concentrations above this point will already select for the AMR mutant (Fig. 4C adapted from Gullberg et al. 2011, with permission).
