Figure 1: Flow chart of study population selection.
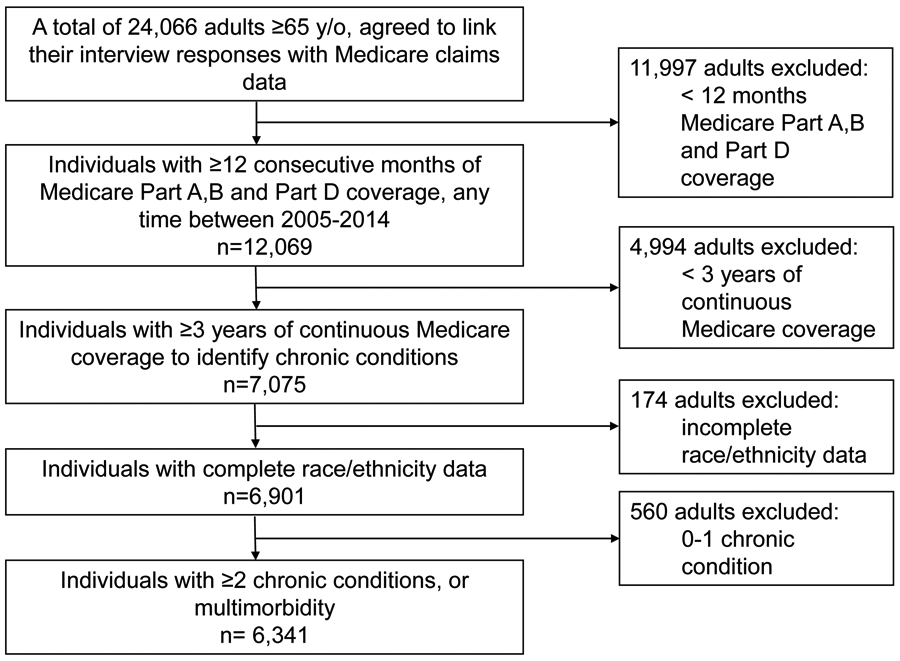
As Medicare claims data were annualized, and follow-up spanned a 10-year period, inclusion of participant information was assessed for each year of Medicare enrollment. For a year to be included in our study, we required participants to have 12 consecutive months of Medicare Parts A, B and Part D coverage, any time between 2005- 2014. A number of our chronic conditions of interest, as defined by the CMS Chronic Conditions Data Warehouse, required at least three years of Medicare coverage in order to assign a diagnosis (e.g. dementia).25
