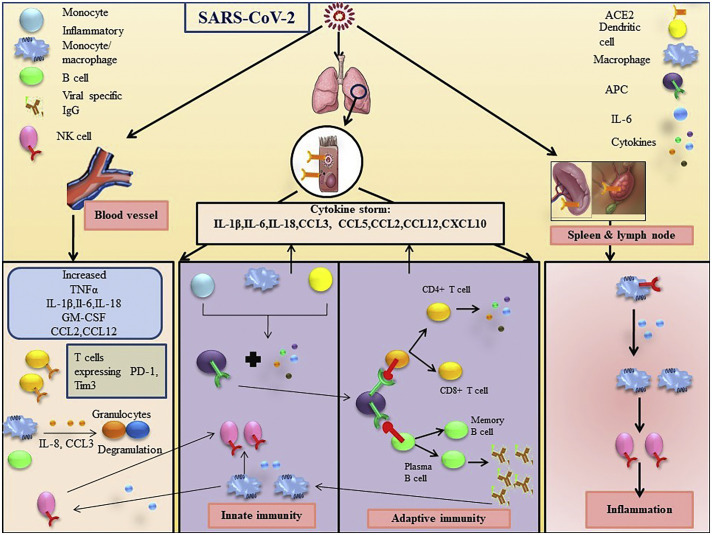
Fig. 1.
Immune response following SARS-CoV-2 infection. SARS-CoV-2 mostly affects the lungs because of higher expression of angiotensin converting enzyme 2 (ACE2) receptor. Upon binding with ACE2 receptor, SARS-CoV-2 enters into cells and elicits immune responses. Dendritic cells, monocytes, macrophages act as antigen presenting cells (APCs) that interact with CD4+ and CD8+ T cells to induce the proliferation of virus specific T cells and facilitate secretion of various cytokines in the lungs. APCs also induce the release of viral specific antibodies, which recruit natural killer (NK) cells from peripheral blood to the lungs, B cells in the lungs and ultimately results in cytokine storm by increasing the secretions of various interleukins (ILs) including IL-6, IL-6, IL-β, TNF-α, C-C motif chemokine ligand (CCL)3, CCL5, CCL2, CCL12, C-X-C motif chemokine ligand (CXCL)10, granulocyte-monocyte colony stimulating factor (GM-CSF). On the other hand, in peripheral blood, in response to virus entry in concert with the high expression of exhaustion markers such as T cell immunoglobulin and mucin domain 3 (Tim3), programmed death-1 (PD-1) in T cells, the expressions of IL-1β, IL-6, IL-18, TNF-α, GM-CSF, CCL2, CCL12 are also elevated. Inflammatory monocytes (IMs) induce the degranulation of granulocytes by secreting CCL3 and IL-8. Due to the expression of ACE2 receptor, SARS-CoV-2 affects spleen along with lymph nodes to the same extent. Virus entry also induces IMs to secret IL-6 and recruits NK cells in tissue microenvironment.