Abstract
We assessed the effects of the Toronto Site Housing First (HF) intervention on hospitalizations and emergency department (ED) visits among homeless adults with mental illness over 7 years of follow-up. The Toronto Site is part of an unblinded multi-site randomized pragmatic trial of HF for homeless adults with mental illness in Canada, which followed participants up to 7 years. Five hundred seventy-five participants were recruited and classified as having high (HN) or moderate need (MN) for mental health support services. Each group was randomized into intervention (HF) and treatment as usual groups, and 567 (98.6%) consented to link their data to health administrative databases. HF participants received a monthly rent supplement of $600 (Canadian) and assertive community treatment (ACT) support or intensive care management (ICM) support based on need level. Treatment as usual (TAU) participants had access to social, housing, and health services generally available in the community. Outcomes included all-cause and mental health-specific hospitalization, number of days in hospital, and ED visit. We used GEE models to estimate ratio of rate ratios (RRR). The results showed HF with ACT had no significant effect on hospitalization rates among HN participants, but reduced the number of days in hospital (RRR = 0.32, 95% CI 0.16-0.63) and number of ED visits (RRR = 0.57, 95% CI 0.34-0.95). HF with ICM resulted in an increase in the number of hospitalizations (RRR = 1.69, 95% CI 1.09-2.60) and ED visit rates (RRR = 1.42, 95% CI 1.01-2.01) but had no effect in days in hospital for MN participants. Addressing the health needs of this population and reducing acute care utilization remain system priorities. Trial registration: http://www.isrctn.com/identifier: ISRCTN42520374
Supplementary Information
The online version contains supplementary material available at 10.1007/s11524-021-00550-1.
Keywords: Homeless persons, Mental illness, Housing First, Hospitalization, Emergency department visit
Introduction
People experiencing homelessness are affected by chronic and acute medical conditions [1–8], neurocognitive impairment, and substance use disorders at higher rates than the general population [1, 9–11]. The unstable living conditions associated with homelessness not only increase heath need complexity but in addition interfere with accessing primary health care and effective disease management. It is therefore not surprising that, individuals experiencing homelessness are higher users of emergency departments (ED) [12] and are more frequently admitted to hospital compared to the general population [2, 12–14]. The provision of stable housing with supportive services has been identified as a promising intervention to decrease ED visits and hospital admissions for this population [15]. However, controlled studies of housing interventions have shown mixed effects on health care utilization [16–19]. These studies have generally used self-reported data on health care use, analyzed only a few specific health care services, or have had a relatively short period of follow-up. These limitations have resulted in uncertainty regarding the long-term impacts of supportive housing programs on health care utilization.
The purpose of this analysis of the Toronto Site At Home/Chez-Soi randomized pragmatic study is to investigate the effects of a Housing First (HF) intervention, including immediate access to housing and mental health support services, on several acute health care utilization outcomes, including all-cause hospitalization, mental health-related hospitalizations, and ED visits, among adults experiencing homelessness and mental illness over a 7-year follow-up period. This analysis leverages comprehensive provincial administrative databases and the longest HF trial to date to ascertain the health utilization outcomes of study participants over an extended follow-up period in a large urban setting with universal health insurance.
Methods
Design and Setting
The present study is a secondary exploratory analysis of the At Home/Chez-Soi (AH|CS) study, Toronto Site, which was part of a multi-site pragmatic randomized trial examining an HF intervention for homeless adults with mental illness in five cities across Canada: Vancouver, Winnipeg, Toronto, Montreal, and Moncton [20]. In contrast to traditional approaches that require homeless individuals to first accept treatment and placement in transitional housing before accessing permanent housing, HF interventions offer homeless individuals immediate access to permanent housing in conjunction with mental health support services. This paper reports findings from the Toronto Site of the At Home/Chez-Soi study. The Full AH|CS trial protocol and the Toronto AH|CS site primary results have been published elsewhere [20, 21].
Participants
The study design, recruitment methods, instruments used, and inclusion criteria have been reported in previous publications [20, 22]. Briefly, participants were included if they fulfilled the following criteria: (1) were ≥18 years old; (2) experienced absolute homelessness or precarious housing; and (3) experienced a mental illness as determined using the Mini International Neuropsychiatric Interview 6.0 (MINI), with or without a co-existing substance use disorder [20, 21]. Individuals were excluded if they were not legally residing in Canada or were already receiving support services equivalent to those provided by the intervention.
Out of 1342 referred candidates, a total of 575 Toronto AH|CS’ participants met eligibility criteria and were recruited from October 1, 2009, to June 2011 and followed over a period of 24 months after randomization. Subsequently, the study received additional funding to extend the intervention and participant follow-up up for a further 4 years. Hence, participants were further followed from January 1, 2014, to March 31, 2017, for an overall long-term follow-up period of up to 7 years.
At baseline, participants were classified as having high need (HN) if they fulfilled all three of the following criteria: (1) having a current psychotic disorder or bipolar disorder based on the MINI; (2) having a Multnomah Community Ability Scale (MCAS) score of 62 or lower, which indicates at least moderate disability; and (3) at least one of three conditions: 2 or more hospitalizations for mental illness in any 1 of the last 5 years, recent arrest or incarceration, or co-morbid substance use based on the MINI. All other participants were classified as having moderate needs (MN) [20, 23].
Intervention
Using a computerized adaptive randomization algorithm implemented by the central data collection system [20], HN participants were randomly assigned to either treatment as usual (TAU) or HF with assertive community treatment (ACT) support plus monthly rent supplement (C$ 600). ACT included an inter-professional team offering nursing and medical care, case management support, and peer support with 24/7 coverage [20]. Participants assigned to TAU had access to social housing and services that were generally available in the community. MN participants were randomly assigned to either treatment as usual (TAU) or the HF with intensive case management (ICM) support plus a monthly rent supplement of C$ 600. ICM services included case management and referral to other services as needed [24, 25].
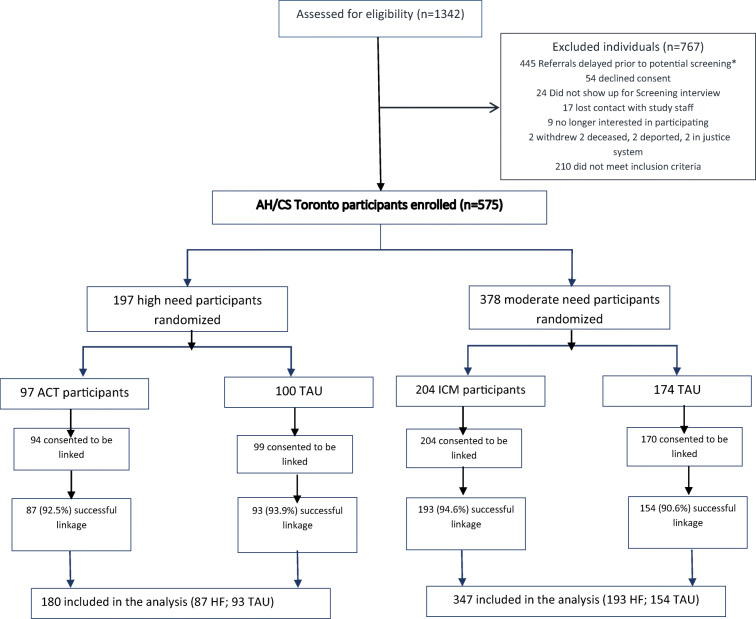
Assuming an attrition rate of 40%, a minimum sample size at baseline of at least 100 participants per intervention group was estimated to have an 80% power to detect a medium effect size (Cohen d = 0.5) [20]. The enrolled, allocated, and analyzed number of participants are shown in Fig. 1.
Fig. 1.
Study flowchart. *Referrals were kept for a period of up to 3 months. During the early phases of the study, there were more referrals than staff available to accept new participants; therefore, many referrals were delayed beyond the 3-month period and were excluded prior to screening
Ethical Approvals
All study participants provided written consent to participate in the study. The study has been approved by the Research Ethics Board at St. Michael’s Hospital in Toronto, Canada. The study has been registered with the International Standard Randomized Control Trial Number Register (ISRCTN 42520374).
Health Administrative Data
Study data were linked with health administrative data and analyses at ICES, which houses administrative health data over the entire Ontario population. Data for all-cause hospitalization were extracted from the Discharge Abstract Database (DAD). Mental health hospitalizations were derived from the Ontario Mental Health Reporting System (OMHRS) combined with mental health admissions in the DAD. Emergency department visits were retrieved from the National Ambulatory Care Reporting System (NACRS). These datasets were linked using unique encoded identifiers and analyzed at ICES.
Outcome Measures
The main outcomes of this analysis were all-cause hospitalization incidence and number of hospitalizations, mental health hospitalization incidence and number of hospitalizations, number of days in hospital, and ED visit incidence and number of visits. The outcomes were extracted from administrative data over the following observation period: (1) the 1-year period prior to randomization; (2) 0-2-year post-randomization (i.e., the 24-month follow-up period planned in the original study design); (3) 2-7-year post-randomization (i.e., the extended follow-up period); and (4) 0-7-year post-randomization (i.e., the entire follow-up period).
Analysis
We analyzed outcomes among all participants and stratified by level of need for mental health services (HN and MN). First, for each observation period, we computed (1) incidence rate (IR), using the first hospitalization or ED visit, and the time-at-risk (calculated in person-years) at the end of each observation period or censored for death or withdrawal from the study; and (2) rate of the total number of hospitalization, number of days hospitalized, and ED visits over each observation period, and the time-at-risk at the end of the analyzed observation periods, or censored at the date of death or withdrawal from the study.
Second, to assess the impact of the intervention on health care utilization rates, we considered both treatment group and time period. We used generalized estimating equation (PROCGENDMOD) models and chose the health care utilization outcome distribution by comparing their mean and variance. We included HF intervention group, time period, and the interaction term between treatment group and time to determine whether the program had a differential impact on the outcome change. For all the estimated models, analyses were conducted at the individual level, and the unstructured covariance matrix was used in all models. An offset equal to the natural log of person-years was included in all models to account for differential time-at-risk for each participant at each observation period. Based on the outcome dispersion, a Poisson distribution was used. Ratios of rate ratios (RRR), comparing prior-randomization and post-randomization rate ratios and 95% CIs and a p-value, were estimated. SAS version 9.4 was used for all analyses (SAS Institute Inc. 2013. SAS® 9.4 Statements: Reference. Cary, NC: SAS Institute Inc.).
Results
Characteristics of Participants
Out of 575 study participants, 567 (98.6%) provided consent to link their survey data with administrative ICES data, and 527 (92.9%) were successfully linked for these analyses. Of these, 180 (34.2%) were from the HN group (HF, n = 87 vs. TAU, n = 93) and 347 (65.8%) from the MN group (HF, n = 193 vs. TAU, n = 154) (Fig. 1). Comparison between our final sample and the not linked participants showed no significant differences regarding sociodemographic characteristics (Supplementary Information Table A1, available on-line).
Tables 1 and 2 present the characteristics of the 527 participants with linked administrative data, by level of need and intervention group at baseline. All sociodemographic characteristics and mental health diagnoses were similar between treatment groups, except for the HN group, where there was a lower mean age and a higher proportion of females in the HF group. Health care utilization patterns over 1 year prior the baseline are depicted by randomized groups and level of need in the Supplementary Information (see Table A2 to A5, available on-line).
Table 1.
Baseline Socioeconomic characteristics of study participants with linked administrative data, by level of need and treatment group
| High Needs (N=180) |
Moderate Needs (N=347) |
|||||||
|---|---|---|---|---|---|---|---|---|
| HF (n=87) |
TAU (n=93) |
HF (n=193) |
TAU (n=154) |
|||||
| n | % or mean ± SD |
% or mean ± SD |
p-value | n | % or mean ± SD |
% or mean ± SD |
p-value | |
| Demographics | ||||||||
| Age (years) | 180 | 37.67±11.06 | 41.45±12.03 | 0.030 | 347 | 39.56±11.60 | 40.79±12.51 | 0.345 |
| Gender, self-reported | ||||||||
| Male | 129 | 57 (65.5%) | 72 (77.4%) | 0.042 | 234 | 131 (67.9%) | 103 (66.9%) | 0.931 |
| Femalea | 49 | 30 (34.5%) | 21 (22.6%) | 113 | 62 (32.1%) | 51 (33.1%) | ||
| Self-Identified ethno-racial group (self-reported) | ||||||||
| Others | 43 | 18 (20.7%) | 25 (26.9%) | 0.451 | 120 | 66 (34.2%) | 54 (35.1%) | 0.068 |
| Black | 55 | 30 (34.5%) | 25 (26.9%) | 115 | 73 (37.8%) | 42 (27.3%) | ||
| White | 82 | 39 (44.8%) | 43 (46.2%) | 112 | 54 (28.0%) | 58 (37.7%) | ||
| Socioeconomic factors | ||||||||
| Marital status | ||||||||
| Single | 127 | 65 (74.7%) | 62 (66.7%) | 0.428 | 231 | 128 (66.3%) | 103 (66.9%) | 0.883 |
| Other | 43 | 19 (21.8%) | 24 (25.9%) | 112 | 63 (32.6%) | 49 (31.8%) | ||
| Education | ||||||||
| Less than high school | 82 | 41 (47.1%) | 41 (44.1%) | 0.566 | 164 | 98 (50.8%) | 66 (42.9%) | 0.328 |
| Completed high school | 33 | 15 (17.2%) | 18 (19.4%) | 63 | 31 (16.1%) | 32 (20.8%) | ||
| Some post-secondary school | 51 | 29 (33.3%) | 22 (23.7%) | 112 | 61 (31.6%) | 51 (33.1%) | ||
| Homelessness during lifetime (years) | ||||||||
| <3 years | 65 | 35 (40.2%) | 30 (32.3%) | 0.543 | 171 | 97 (50.3%) | 74 (48.1%) | 0.663 |
| ≥3years | 104 | 51 (58.6%) | 53 (57.0%) | 171 | 93 (48.2%) | 78 (50.6%) | ||
a= Includes seven transsexual or transgender participants
Table 2.
Mental health disorders of study participants with linked administrative data, by level of need and treatment group at baseline
| High Needs (N=180) |
Moderate Needs (N=347) |
|||||||
|---|---|---|---|---|---|---|---|---|
| HF (n=87) |
TAU (n=93) |
HF (n=87) |
TAU (n=93) |
|||||
| n |
% or mean ± SD |
% or mean ± SD |
p-value | n |
% or mean ± SD |
% or mean ± SD |
p-value | |
| Mental health and substance usea | ||||||||
| Major depressive episode | ||||||||
| No | 148 | 72 (82.8%) | 76 (81.7%) | 0.856 | 192 | 106 (54.9%) | 86 (55.8%) | 0.864 |
| Yes | 32 | 15 (17.2%) | 17 (18.3%) | 155 | 87 (45.1%) | 68 (44.2%) | ||
| Manic or hypomanic episode | ||||||||
| No | 163 | 76 (87.4%) | 87 (93.5%) | 0.156 | 309 | 171 (88.6%) | 138 (89.6%) | 0.765 |
| Yes | 17 | 11 (12.6%) | 6 (6.5%) | 38 | 22 (11.4%) | 16 (10.4%) | ||
| Post-traumatic stress disorder | ||||||||
| No | 157 | 74 (85.1%) | 83 (89.2%) | 0.400 | 250 | 137 (71.0%) | 113 (73.4%) | 0.622 |
| Yes | 23 | 13 (14.9%) | 10 (10.8%) | 97 | 56 (29.0%) | 41 (26.6%) | ||
| Panic disorder | ||||||||
| No | 172 | 82 (94.3%) | 90 (96.8%) | 0.412 | 281 | 157 (81.3%) | 124 (80.5%) | 0.845 |
| Yes | 8 |
1 to 5 (0.6 to 5.8%)b |
1 to 5 (1.1% to 5.5%)b |
66 | 36 (18.7%) | 30 (19.5%) | ||
| Mood disorder with psychotic features | ||||||||
| No | 134 | 65 (74.7%) | 69 (74.2%) | 0.936 | 282 | 158 (81.9%) | 124 (80.5%) | 0.750 |
| Yes | 46 | 22 (25.3%) | 24 (25.8%) | 65 | 35 (18.1%) | 30 (19.5%) | ||
| Psychotic disorder | ||||||||
| No | 74 | 37 (42.5%) | 37 (39.8%) | 0.709 | 260 | 145 (75.1%) | 115 (74.7%) | 0.923 |
| Yes | 106 | 50 (57.5%) | 56 (60.2%) | 87 | 48 (24.9%) | 39 (25.3%) | ||
| Substance use disorder | ||||||||
| No | 161 | 75 (86.2%) | 86 (92.5%) | 0.172 | 318 | 175 (90.7%) | 143 (92.9%) | 0.465 |
| Yes | 19 | 12 (13.8%) | 7 (7.5%) | 29 | 18 (9.3%) | 11 (7.1%) | ||
| Alcohol abuse | ||||||||
| No | 148 | 70 (80.5%) | 78 (83.9%) | 0.550 | 304 | 165 (85.5%) | 139 (90.3%) | 0.181 |
| Yes | 32 | 17 (19.5%) | 15 (16.1%) | 43 | 28 (14.5%) | 15 (9.7%) | ||
a= Based on the DSM-IV criteria using the Mini International Neuropsychiatric Interview [MINI] version 6.0, c=Absolute numbers less than six have been suppressed to reduce the risk of identification
Over the 7-year follow-up period, participants had similar incidence rate for all-cause hospitalization (HF: 0.23, 95% CI [0.20-0.27] vs. TAU: 0.20, 95% CI [0.17-0.23] per person year) or for ED visits (HF: 0.63, 95% CI [0.55-0.71] vs. TAU: 0.64, 95% CI [0.56-0.73]). However, compared to the TAU group, HF participants had lower number of days in hospital (HF: 7.82, 95% CI [7.69-7.95] vs. TAU: 10.74, 95% CI [10.58-10.91]) and lower number of ED visits (HF: 3.28, 95% CI [3.19-3.36] vs. TAU: 4.07 95% CI [3.97-4.17]). When analyzing the incidence and count rates by level of needs for mental health services, HN participants had higher acute health care utilization rates compared to MN participants, regardless of their intervention group (HF or TAU) (see Table A2 to A2 in the Supplementary Information, available on-line).
Table 3 shows the intervention group by time interaction results from models comparing each post-randomization period (0-2 years, 2-7 years, 0-7 years) with 1-year pre-randomization. Over the 7 years of follow-up, the HF intervention had differential effects on hospitalizations and ED visits according to the need level of participants. In the HN group, HF was not associated with changes in all-cause or mental health incidence hospitalization rates. However, HF was associated with reduction in the number of days in hospital (ratio of rate ratio—RRR = 0.32 95% CI: 0.16-0.63) and the number of ED visits (RRR = 0.57 95% CI: 0.34-0.95) compared to TAU.
Table 3.
Treatment and time interaction results from models comparing each post-randomization period with 1 year pre-randomization
| Outcome | Randomization groups | 0 to 2 years post-randomization vs | 2 to 7 years post-randomization vs | 0 to 7 years post-randomization vs |
|---|---|---|---|---|
| 1 year pre-randomization | 1 year pre-randomization | 1 year pre-randomization | ||
| Ratio of rate ratios (95%CI) | Ratio of rate ratios (95%CI) | Ratio of rate ratios (95%CI) | ||
| Hospitalization | All Interventions vs. All Treatment as Usual | 0.98 (0.72-1.33) | 1.32 (0.95-1.84) | 1.15 (0.85-1.56) |
| HN-HF vs. TAU | 0.70 (0.45-1.07) | 0.89 (0.52-1.52) | 0.83 (0.52-1.35) | |
| MN-HF vs. TAU | 1.31 (0.82-2.10) | 1.66 (1.06-2.61) | 1.40 (0.92-2.13) | |
| Number of hospitalizations | All Interventions vs. All Treatment as Usual | 1.10 (0.79-1.52) | 1.20 (0.81-1.76) | 1.16 (0.83-1.62) |
| HN-HF vs. TAU | 0.69 (0.45-1.04) | 0.87 (0.49-1.55) | 0.80 (0.49-1.30) | |
| MN-HF vs. TAU | 1.80 (1.13-2.88) | 1.64 (1.01-2.70) | 1.69 (1.09-2.60) | |
| Mental health Hospitalization | All Interventions vs. All Treatment as Usual | 1.06 (0.75-1.50) | 1.28 (0.88-1.87) | 1.15 (0.83-1.60) |
| HN-HF vs. TAU | 0.72 (0.46-1.15) | 0.82 (0.47-1.45) | 0.71 (0.44-1.16) | |
| MN-HF vs. TAU | 1.61 (0.91-2.86) | 1.87 (1.07-3.27) | 1.66 (1.01-2.74) | |
| Number of mental health Hospitalizations | All Interventions vs. All Treatment as Usual | 1.08 (0.72-1.63) | 1.13 (0.71-1.80) | 1.11 (0.74-1.65) |
| HN-HF vs. TAU | 0.62 (0.37-1.04) | 0.77 (0.41-1.45) | 0.71 (0.42-1.22) | |
| MN-HF vs. TAU | 1.99 (1.11-3.56) | 1.79 (0.95-3.38) | 1.86 (1.09-3.17) | |
| Number of days in hospital | All Interventions vs. All Treatment as Usual | 0.62 (0.38-1.03) | 0.42 (0.22-0.77) | 0.48 (0.29-0.81) |
| HN-HF vs. TAU | 0.45 (0.24-0.83) | 0.28 (0.12-0.66) | 0.32 (0.16-0.63) | |
| MN-HF vs. TAU | 1.81 (0.96-3.39) | 0.99 (0.43-2.29) | 1.29 (0.63-2.65) | |
| Emergency Department (ED) visit | All Interventions vs. All Treatment as Usual | 1.02 (0.78-1.34) | 1.26 (0.95-1.65) | 1.10 (0.82-1.48) |
| HN-HF vs. TAU | 0.63 (0.39-1.03) | 0.75 (0.44-1.27) | 0.57 (0.31-1.03) | |
| MN-HF vs. TAU | 1.29 (0.92-1.80) | 1.59 (1.15-2.20) | 1.42 (1.01-2.01) | |
| Number of ED visits | All Interventions vs. All Treatment as Usual | 0.89 (0.65-1.22) | 0.82 (0.52-1.29) | 0.84 (0.60-1.19) |
| HN-HF vs. TAU | 0.75 (0.44-1.26) | 0.49 (0.25-0.94) | 0.57 (0.34-0.95) | |
| MN-HF vs. TAU | 1.12 (0.81-1.53) | 1.51 (1.02-2.23) | 1.36 (0.99-1.88) |
Bold means “statistically significant at a level of 5%”
On the other hand, for the MN group, HF was associated with an increase in all-cause of incidence hospitalizations (RRR = 1.69 (95% CI: 1.09-2.60)), mental health hospitalizations (RRR = 1.66 (95% CI: 1.01-2.74)), and ED visit rates (RRR = 1.42 (95% CI: 1.01-2.01)). HF was not associated with the number of days in hospital.
Similar results were found where 0-2 years and 2-7 years to 1-year pre-randomization were compared.
Discussions
This study, leveraging 7-year follow-up data from a randomized trial of Housing First, examined the long-term effects of HF interventions on acute health care utilization among homeless adults with mental illness by linking to administrative provincial health records. Findings revealed that the effects of the intervention differed substantially by participant baseline need levels and service support intensity. For participants with high needs at baseline, receiving HF with ACT support, there were no significant effects on all-cause and mental health hospitalizations, but a significant reduction in the number of days in hospital as well as the number of ED visits. A study of an HF intervention in four French cities among high-need participants similarly found no significant effects on hospitalization or ED visits, but reduced inpatient days [26]. Another randomized study of the effects of permanent supportive housing for chronically homeless high users of multiple systems in Santa Clara County, California (USA) found no effects on ED or inpatient care use [27].
For individuals with moderate needs at baseline, receiving HF with ICM, the intervention resulted in an increase in the number of all-cause and mental health hospitalizations, and ED visits, but had no statistically significant effect on days in hospital, compared to TAU participants. Previous analyses similarly highlighted mixed effects of housing interventions on health outcomes and health care utilization [28, 29] when analyzing high and moderate-need participants separately. These analyses found a reduction in ED visits among HN participants, compared to the TAU group, and no effect among MN participants over a 2-year period [30, 31]. Differential effects between high and moderate groups were also found for other outcomes, such as quality of life scores [32], food security [33], or rapid and stable rehousing [29, 34].
Several factors inherent to the HF intervention could underline these findings. Prior AH|CS analyses demonstrated that HF can facilitate rapid rehousing among the MN group, contrarily to the HN group [29, 34]. Rapid rehousing enables MN participants to shift priorities, from housing and survival to other basic needs, including health care for chronic comorbidities that may require both preventive and acute care. This may have contributed to the increase of the number of all-cause hospitalizations (RRR = 1.80 95% CI: 1.13-2.88) and mental health hospitalization (RRR = 1.99 95% CI: 1.11-3.56) during the 0-2-year post-randomization.
The ICM support provided to MN participants, based on need level at enrolment, seems limited to cope with these new challenges, compared to ACT services for HN participants. Contrary to ICM, the ACT model included intensive support available 7 days/week and 24 h/day, including psychiatric support [25, 35]. A recent systematic review of the effects of different case management intervention models on health and social outcomes of homeless populations highlighted that intensive case management (ICM), offered to moderate-need participants, had limited and mixed effects on participants’ hospitalization outcomes [25]. ICM interventions resulted in small reductions in the number of ED visits in some settings, but showed no effect on the utilization of other hospital services, when compared to usual care [36–38]. However, the effects of ACT interventions on hospitalization outcomes were mainly positive, reducing by half the number days in hospital, compared to standard case management [39] or resulting in fewer ED visits and number of days in hospital compared to usual care [25, 40].
The strengths of our study included a rigorous randomized controlled design, long duration of follow-up, use of administrative databases to ascertain hospitalization and ED visits with an extremely high level of completeness, and the ability to compare effects in participants with both moderate and high support needs.
Nonetheless, our study has certain limitations. First, the study focused specifically on homeless adults with mental illness and with access to Ontario Health Insurance Plan, and our findings may not be applicable to other homeless populations. A second limitation is that the support services provided to high-need and moderate-need groups were different, and it is not possible to determine if the different outcomes observed in these groups were due to the type of services provided, the baseline characteristics of the participants, or a combination of the two. Finally, regarding the generalisability of our results, the study was conducted in a country with universal health care and a broad social safety network. Thus, TAU participants were able to access to housing, social and economic services in the community, potentially reducing the apparent effectiveness of the intervention.
Conclusion
In summary, the provision of immediate housing and ICM support to homeless adults with moderate need for mental health services was associated with increased hospitalization rates and ED visits, but had no effect on the days in hospital. In contrast, a Housing First intervention providing immediate housing and ACT support had no effect on hospitalization rates among homeless adults with high need for mental health services, but reduced the number of days in hospital and ED visits. These findings demonstrate the importance of addressing the health and support needs of this population, especially those that may not qualify for ACT services that may require more comprehensive and coordinated supports, than those available through ICM.
Supplementary Information
(DOCX 59 kb)
Acknowledgments
We thank the At Home/Chez-Soi participants whose willingness to share their lives, experiences, and stories with us made this project possible. We also thank the At Home/Chez-Soi project team, site coordinators, and service providers who have contributed to the design, implementation, and follow-up of the project at the Toronto Site. The Toronto Site of the AH|CS study was funded by the Mental Health Commission of Canada, Ontario Ministry of Health and Long-Term Care (HSRF #259), and the Canadian Institute of Health Research (CIHR MOP-130405). Initials of authors who received Grants: HSRF #259: VS and SWH CIHR operating grant: MOP-130405: VS, PO, and SWH. CML have reported receiving funding from St. Michael’s Hospital Research Training Centre Scholarship award (2019). JL acknowledges support from the Canadian Institute of Health Research-Institute of Population and Public through a fellowship award recipient in Research and Knowledge Translation on Urban Housing and Health (201910RAT-435231-65841) in partnership with Canada Mortgage and Housing Corporation.
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). ICES is an independent, non-profit research institute funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). As a prescribed entity under Ontario’s privacy legislation, ICES is authorized to collect and use health care data for the purposes of health system analysis, evaluation and decision support. Secure access to these data is governed by policies and procedures that are approved by the Information and Privacy Commissioner of Ontario. (In 2018, the institute formerly known as the Institute for Clinical Evaluative Sciences formally adopted the initialism ICES as its official name. This change acknowledges the growth and evolution of the organization’s research since its inception in 1992, while retaining the familiarity of the former acronym within the scientific community and beyond.)
Parts of this material are based on data and/or information compiled and provided by Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed in the material are those of the authors, and not necessarily those of CIHI.
Author Contribution
Stephen W. Hwang, James Lachaud, Vicky Stergiopoulos, Patricia Ocampo, Rosane Nisenbaum, and Cilia Mejia-Lancheros conceptualized this analysis. James Lachaud, Cilia Mejia-Lancheros, Rosane Nisenbaum, Ri Wang, Anna Durbin, and Stephen W. Hwang oversaw the statistical analyses. James Lachaud and Stephen W. Hwang wrote the first manuscript version. All the authors contributed to the validation and interpretation of the findings and critical revision and editing of the first manuscript version. Patricia Ocampo, Vicky Stergiopoulos, and Stephen W. Hwang are also the co-principal investigators of the Toronto Site of the AH|CS study. All co-authors revised and approved the final version of the manuscripts and are accountable for all aspects of the work.
Declarations
Disclaimer
The desing, analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Data Access, Responsibility, and Analysis
Drs Hwang and Lachaud had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Data Sharing Statement
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (e.g., healthcare organizations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–1540. doi: 10.1016/S0140-6736(14)61132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hwang SW, Chambers C, Chiu S, Katic M, Kiss A, Redelmeier DA, Levinson W. A comprehensive assessment of health care utilization among homeless adults under a system of universal health insurance. Am J Public Health. 2013;103(SUPPL. 2):294–301. doi: 10.2105/AJPH.2013.301369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mackelprang JL, Graves JM, Rivara FP. Homeless in America: injuries treated in US emergency departments, 2007-2011. Int J Inj Control Saf Promot. 2014;21(3):289–297. doi: 10.1080/17457300.2013.825631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baggett TP, O’Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. 2010;100(7):1326–1333. doi: 10.2105/AJPH.2009.180109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferenchick GS. The medical problems of homeless clinic patients: a comparative study. J Gen Intern Med. 1990;7(3):294–297. doi: 10.1007/BF02598086. [DOI] [PubMed] [Google Scholar]
- 6.Gelberg L, Linn LS. Assessing the physical health of homeless adults. JAMA J Am Med Assoc. 1989;262(14):1973–1979. doi: 10.1001/jama.1989.03430140091031. [DOI] [PubMed] [Google Scholar]
- 7.Savage CL, Lindsell CJ, Gillespie GL, Dempsey A, Lee RJ, Corbin A. Health care needs of homeless adults at a nurse-managed clinic. J Community Health Nurs. 2006;23(4):225–234. doi: 10.1207/s15327655jchn2304_3. [DOI] [PubMed] [Google Scholar]
- 8.Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859–870. doi: 10.1016/S1473-3099(12)70177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hwang SW. Homelessness and health. Cmaj. 2001;164(2):229–233. doi: 10.1136/bmj.327.7406.110-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in Western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):1670–1681. doi: 10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. J Am Med Assoc. 2000;283(16):2152–2157. doi: 10.1001/jama.283.16.2152. [DOI] [PubMed] [Google Scholar]
- 12.Chambers C, Chiu S, Katic M, et al. High utilizers of emergency health services in a population-based cohort of homeless adults. Am J Public Health. 2013;103(SUPPL. 2) 10.2105/AJPH.2013.301397. [DOI] [PMC free article] [PubMed]
- 13.Hwang S, Henderson M. Health care utilization in homeless people: translating research into policy and practice. Agency Healthc Res Qual Work. 2010;(10002):1–73. http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Health+Care+Utilization+in+Homeless+People:+Translating+Research+into+Policy+and+Practice#1. Accessed Jan 2021
- 14.Clark RE, Weinreb L, Flahive JM, Seifert RW. Health care utilization and expenditures of homeless family members before and after emergency housing. Am J Public Health. 2018;108(6):808–814. doi: 10.2105/AJPH.2018.304370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Academies of Sciences, Engineering and M. Permanent supportive housing: evaluating the evidence for improving health outcomes among people experiencing chronic homelessness. The National Academies Press.; 2018. doi:10.17226/25133 [PubMed]
- 16.Mackelprang JL, Collins SE, Clifasefi SL. Housing first is associated with reduced use of emergency medical services. Prehospital Emerg Care. 2014;18(4):476–482. doi: 10.3109/10903127.2014.916020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larimer ME, Malone DK, Garner MD, Atkins DC, Burlingham B, Lonczak HS, Tanzer K, Ginzler J, Clifasefi SL, Hobson WG, Marlatt GA. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA - J Am Med Assoc. 2009;301(13):1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- 18.Wright BJ, Vartanian KB, Li H-F, Royal N, Matson JK. Formerly homeless people had lower overall health care expenditures after moving into supportive housing. Health Aff. 2016;35(1):20–27. doi: 10.1377/hlthaff.2015.0393. [DOI] [PubMed] [Google Scholar]
- 19.Fenwick E, Macdonald C, Thomson H. Economic analysis of the health impacts of housing improvement studies: a systematic review. J Epidemiol Community Health. 2013;67(10):835–845. doi: 10.1136/jech-2012-202124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goering PN, Streiner DL, Adair C, Aubry T, Barker J, Distasio J, Hwang SW, Komaroff J, Latimer E, Somers J, Zabkiewicz DM. The at Home/Chez Soi trial protocol: a pragmatic, multi-site, randomised controlled trial of a Housing First intervention for homeless individuals with mental illness in five Canadian cities. BMJ Open. 2011;1(2):1–18. doi: 10.1136/bmjopen-2011-000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hwang SW, Stergiopoulos V, O’Campo P, Gozdzik A. Ending homelessness among people with mental illness: the at Home/Chez Soi randomized trial of a Housing First intervention in Toronto. BMC Public Health. 2012;12(787):1–16. doi: 10.1186/1471-2458-12-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Canadian Population Health Initiative of the Canadian Institute for Health. Mental health, mental illness, and homelessness in Canada (200(. In: Hulchanski JD, Campsie P, Chau SBY, Hwang SW, Paradis E, eds. Finding home: policy options for addressing homelessness in Canada (e‐book). Toronto (Canada), Cities Centre, University of Toronto; 2009:306-353. https://www.homelesshub.ca/FindingHome. Accessed Jan 2021.
- 23.Stergiopoulos V, Hwang SW, Gozdzik A, Nisenbaum R, Latimer E, Rabouin D, Adair CE, Bourque J, Connelly J, Frankish J, Katz LY, Mason K, Misir V, O’Brien K, Sareen J, Schütz CG, Singer A, Streiner DL, Vasiliadis HM, Goering PN. Effect of scattered-site housing using rent supplements and intensive case management on housing stability among homeless adults with mental illness: a randomized trial. JAMA - J Am Med Assoc. 2015;313(9):905–915. doi: 10.1001/jama.2015.1163. [DOI] [PubMed] [Google Scholar]
- 24.De Vet R, Van Luijtelaar MJA, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JRLM. Effectiveness of case management for homeless persons: a systematic review. Am J Public Health. 2013;103(10) 10.2105/AJPH.2013.301491. [DOI] [PMC free article] [PubMed]
- 25.Ponka D, Agbata E, Kendall C, et al. The effectiveness of case management interventions for the homeless, vulnerably housed and persons with lived experience: a systematic review. PLoS One. 2020;15(4) 10.1371/journal.pone.0230896. [DOI] [PMC free article] [PubMed]
- 26.Tinland A, Loubière S, Boucekine M, Boyer L, Fond G, Girard V, Auquier P. Effectiveness of a housing support team intervention with a recovery-oriented approach on hospital and emergency department use by homeless people with severe mental illness: a randomised controlled trial. Epidemiol Psychiatr Sci. 2020;29:e169. doi: 10.1017/S2045796020000785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raven MC, Niedzwiecki MJ, Kushel M. A randomized trial of permanent supportive housing for chronically homeless persons with high use of publicly funded services. Health Serv Res. 2020;55(S2):797–806. doi: 10.1111/1475-6773.13553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: a systematic review. Am J Prev Med. 2005;29(4):311–319. doi: 10.1016/j.amepre.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 29.Stergiopoulos V, Mejia-Lancheros C, Nisenbaum R, Wang R, Lachaud J, O'Campo P, Hwang SW. Long-term effects of rent supplements and mental health support services on housing and health outcomes of homeless adults with mental illness: extension study of the At Home/Chez Soi randomised controlled trial. Lancet Psychiatry. 2019;6(11):915–925. doi: 10.1016/S2215-0366(19)30371-2. [DOI] [PubMed] [Google Scholar]
- 30.Goldfinger SM, Schutt RK, Tolomiczenko GS, et al. Housing placement and subsequent days homeless among formerly homeless adults with mental illness. Psychiatr Serv. 1999;50(5):674–679. doi: 10.1176/ps.50.5.674. [DOI] [PubMed] [Google Scholar]
- 31.Aubry T, Nelson G, Tsemberis S. Housing first for people with severe mental illness who are homeless: a review of the research and findings from the At Home-Chez soi demonstration project. Can J Psychiatr Rev Can Psychiatr. 2015;60(11 PG-467-74):467–474. doi: 10.1177/070674371506001102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aubry T, Goering P, Veldhuizen S, Adair CE, Bourque J, Distasio J, Latimer E, Stergiopoulos V, Somers J, Streiner DL, Tsemberis S. A multiple-city RCT of housing first with assertive community treatment for homeless Canadians with serious mental illness. Psychiatr Serv. 2016;67(3):275–281. doi: 10.1176/appi.ps.201400587. [DOI] [PubMed] [Google Scholar]
- 33.O’Campo P, Hwang SW, Gozdzik A, Schuler A, Kaufman-Shriqui V, Poremski D, Lazgare LIP, Distasio J, Belbraouet S, Addorisio S. Food security among individuals experiencing homelessness and mental illness in the At Home/Chez Soi Trial. Public Health Nutr. 2017;20(11):2023–2033. doi: 10.1017/S1368980017000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lachaud J, Mejia-Lancheros C, Nisenbaum R, Stergiopoulos V, O’Campo P, Hwang SW. Housing First model and severe mental disorders: the challenge of exiting homelessness. Ann Am Acad Pol Soc Sci. Published online 2020:In Press.
- 35.Bond GR, Drake RE, Mueser KT, Latimer E. Assertive community treatment for people with severe mental illness: critical ingredients and impact on patients. Dis Manag Heal Outcomes. 2001;9(3):141–159. doi: 10.2165/00115677-200109030-00003. [DOI] [Google Scholar]
- 36.Rosenblum A, Nuttbrock L, McQuistion H, Magura S, Joseph H. Medical outreach to homeless substance users in New York City: preliminary results. Subst Use Misuse. 2002;37:1269–1273. doi: 10.1081/JA-120004184. [DOI] [PubMed] [Google Scholar]
- 37.Shumway M, Boccellari A, O’Brien K, Okin RL. Cost-effectiveness of clinical case management for ED frequent users: results of a randomized trial. Am J Emerg Med. 2008;26(2):155–164. doi: 10.1016/j.ajem.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 38.Malte CA, Cox K, Saxon AJ. Providing intensive addiction/housing case management to homeless veterans enrolled in addictions treatment: a randomized controlled trial. Psychol Addict Behav. 2017;31:231–241. doi: 10.1037/adb0000273. [DOI] [PubMed] [Google Scholar]
- 39.Essock SM, Frisman LK, Kontos NJ. Cost-effectiveness of assertive community treatment teams. Am J Orthop. 1998;68(2):179–190. doi: 10.1037/h0080328. [DOI] [PubMed] [Google Scholar]
- 40.Essock SM, Mueser KT, Drake RE, Covell NH, McHugo GJ, Frisman LK, Kontos NJ, Jackson CT, Townsend F, Swain K. Comparison of ACT and standard case management for delivering integrated treatment for co-occurring disorders. Psychiatr Serv. 2006;57(2):185–196. doi: 10.1176/appi.ps.57.2.185. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 59 kb)