Fig. 4 |. Restoring connectivity in autonomic systems.
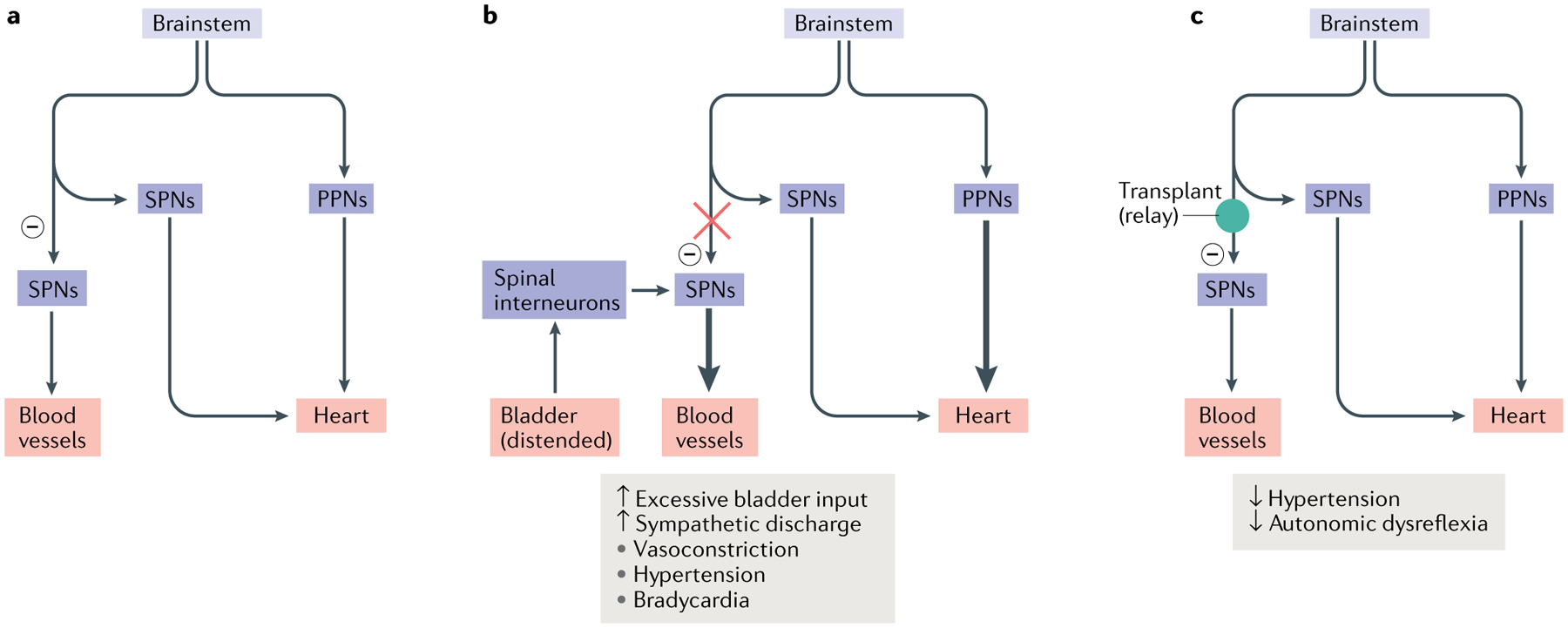
The majority of the vasculature is controlled by sympathetic activity, while the heart is regulated by both the sympathetic system and the parasympathetic system. Sympathetic preganglionic neurons (SPNs) in the spinal cord project to the periphery and synapse onto sympathetic postganglionic neurons. The latter extend axon terminals into the blood vessel and heart. a | In normal conditions, sympathetic excitation induces vasoconstriction and thus increases blood pressure. Subsequently, baroreceptor-mediated parasympathetic excitation decreases the heart rate. In addition, supraspinal vasomotor pathways provide inhibitory regulation (indicated by a minus sign) to suppress the sympathetic activity to blood vessels, leading to recovery of normal blood pressure. b | After spinal cord injury, spinal SPNs lose this descending inhibitory modulation. When excessive sensory or visceral stimulation below the level of injury (for example, bladder distension) activates SPNs via interneurons, the massive discharge of SPNs causes vasoconstriction and increases blood pressure. This causes baroreceptor-mediated bradycardia to occur. However, the absence of supraspinal inhibitory signals to caudal SPNs means that blood pressure remains high. The resulting simultaneous hypertension and bradycardia is known as autonomic dysreflexia. c | Transplantation of early-stage neurons into the lesion of the spinal cord reconstitutes supraspinal vasomotor pathways. Grafted cells relay supraspinal inhibitory signals across the lesion to target neurons in the caudal portion of the spinal cord, which can restore sympathetic regulation of cardiovascular function after spinal cord injury. PPNs, parasympathetic preganglionic neurons.
