Abstract
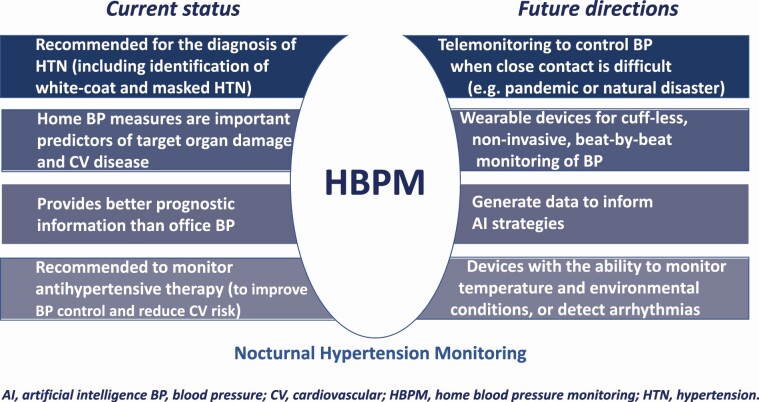
Home blood pressure monitoring (HBPM) is a reliable, convenient, and less costly alternative to ambulatory blood pressure monitoring (ABPM) for the diagnosis and management of hypertension. Recognition and use of HBPM have dramatically increased over the last 20 years and current guidelines make strong recommendations for the use of both HBPM and ABPM in patients with hypertension. The accuracy and reliability of home blood pressure (BP) measurements require use of a validated device and standardized procedures, and good patient information and training. Key HBPM parameters include morning BP, evening BP, and the morning–evening difference. In addition, newer semi-automatic HBPM devices can also measure nighttime BP at fixed intervals during sleep. Advances in technology mean that HBPM devices could provide additional relevant data (e.g., environmental conditions) or determine BP in response to a specific trigger (e.g., hypoxia, increased heart rate). The value of HBPM is highlighted by a growing body of evidence showing that home BP is an important predictor of target organ damage, and cardiovascular disease (CVD)- and stroke-related morbidity and mortality, and provides better prognostic information than office BP. In addition, use of HBPM to monitor antihypertensive therapy can help to optimize reductions in BP, improve BP control, and reduce target organ damage and cardiovascular risk. Overall, HBPM should play a central role in the management of patients with hypertension, with the goal of identifying increased risk and predicting the onset of CVD events, allowing proactive interventions to reduce risk and eliminate adverse outcomes.
Keywords: blood pressure, cardiovascular disease, home blood pressure monitoring, hypertension, out-of-office blood pressure measurement, target organ damage
Graphical Abstract
Graphical Abstract.
HISTORY AND GUIDELINES
Home blood pressure monitoring (HBPM) uses similar technology to ambulatory blood pressure monitoring (ABPM), but allows patients to perform their own blood pressure (BP) measurements at a time and frequency that suits them. HBPM provides information on BP at specific times and under everyday conditions over long time periods. Key advantages of HBPM include its relatively widespread availability, the ability to take multiple daily readings over a long period of time, avoidance of white-coat reactions, the ability to detect masked hypertension and BP variability, improved management of hypertension due to immediate feedback and patient involvement in their healthcare, and relatively low cost.1–3 Disadvantages include the requirement for patient education and training, measurement errors, and lack of funding in some healthcare settings.1
Although ABPM is the gold standard out-of-office BP measurement, HBPM is recommended as a more practical and less expensive alternative, especially for long-term monitoring of treated patients with hypertension.4,5 Recognition and use of HBPM have increased dramatically over the last 20 years.6 Current hypertension guideline documents make strong recommendations for the use of out-of-office BP monitoring techniques, including HBPM and ABPM, for the diagnosis of hypertension and for the monitoring and management of antihypertensive therapy (Table 1).1,7–10
Table 1.
Home blood pressure monitoring recommendations in major guideline and consensus documents
| Diagnosis of hypertension | Diagnostic BP threshold, mm Hg | Titration and monitoring of antihypertensive therapy | Target BP threshold, mm Hg | |
|---|---|---|---|---|
| ACC/AHA 20179 | ✓ | ≥130/80 | ✓ | <130/80 |
| ESC/ESH 201810 | ✓ | ≥135/85 | ✓ | ≤130/80 |
| ISH 20208 | ✓ | ≥135/85 | ✓ | <135/85 |
| JSH 20197 | ✓ | ≥135/85 | ✓ | <125/75 (age <75 y) or <135/85 (age ≥75 y) |
| China 201911 | ✓ | ≥135/85 | ✓ | <140/90 or <130/80 if tolerated or in high-risk pts |
| Taiwan 201512 | ✓ | ≥135/85 | ✓ | <140/90 or <130/80 if tolerated or in high-risk pts |
| South Korea 201813 | ✓ | ≥135/85 | ✓ | <140/90 (uncomplicated/elderly) or <130/80 (high-risk pts) |
| HOPE Asia Network14 | ✓ | ≥135/85 | ✓ | <135/85 |
Abbreviations: pts, patients; y, years.
Patients for whom out-of-office BP monitoring with HBPM is indicated include those with high office BP (to detect white-coat hypertension), high-normal office BP or normal office BP with hypertension-mediated organ damage or high cardiovascular (CV) risk (to detect masked hypertension), highly variable office BP or resistant hypertension, and for evaluating BP control (especially in high-risk patients).8,10,15 The Japanese guidelines state that where there is a discrepancy between office BP and home BP readings, a home BP-based diagnosis should take precedence.7
HOME BP MEASUREMENT: SCHEDULE, THRESHOLDS, AND APPROACHES
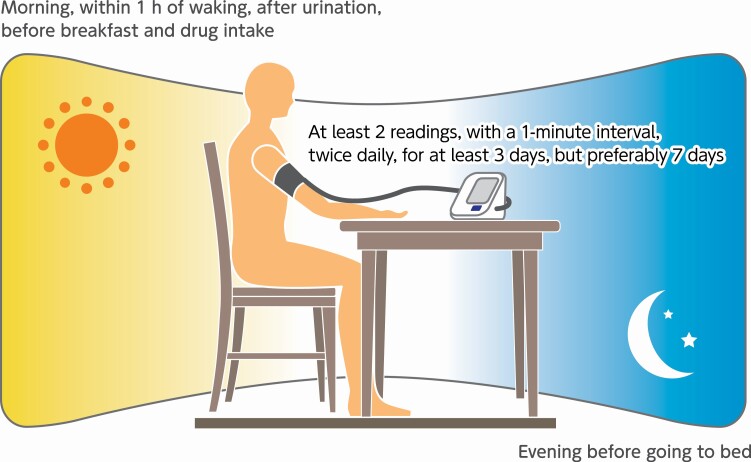
Good patient information and training, use of standardized procedures and use of a validated device are essential for ensuring the accuracy and reliability of home BP measurements (Figure 1).16 Patients need to be provided with general information about hypertension diagnosis and treatment, along with guidance on how to select an appropriate HBPM device and how to measure their own BP (ideally accompanied by a hands-on demonstration).1,5,16 It is important to remind patients not to overuse HBPM and not to modify their antihypertensive therapy without consulting their physician.1 In addition to being validated, the HBPM device should use an upper-arm cuff oscillometric method (with an appropriately sized cuff) and be able to automatically store all readings; telehealth-equipped devices that can transmit readings to healthcare providers are preferable.1,5,16,17 The patient should have an empty bladder, and rest quietly in a seated position with the back supported and both feet on the floor for 2–5 minutes before taking home BP measurements. The cuff of the device should be placed directly above the elbow and pulled taut, with the arm supported on a flat surface. Morning measurements should be made before breakfast and before taking any antihypertensive drugs, and evening measurements should be taken before going to bed. At least 2 readings should be taken, 1–2 minutes apart, and measurements should be made for at least 3 (preferably 7) consecutive days.1,14,16,18
Figure 1.
Key recommendations for ensuring accurate measurement of home blood pressure.14, 16, 18
The key parameters provided by HBPM include morning BP, evening BP, and the morning–evening difference in BP. The relationship between values for these home BP measures and office BP is shown in Table 2. However, 1 limitation of standard HBPM is that measurements are only taken at 2 times during the day (morning and evening) in a relatively low-stress environment (i.e., the patient’s home). Given that young adult workers often show increased work site BP, especially during stressful conditions, even when home BP is well controlled,19,20 there may be also be a role for HBPM in the work place.
Table 2.
Home blood pressure (BP) values (mm Hg) corresponding to clinic measurements (reproduced, with permission, from Kario et al.)14
| Clinic BP (mm Hg) | Home BP (mm Hg) | |||
|---|---|---|---|---|
| Morning | Evening | Nighttime | ME average | |
| 120/80 | 120/80 | 120/80 | 100/65 | 120/80 |
| 130/80 | 130/80 | 130/80 | 110/65 | 130/80 |
| 140/90a | 135/85a | 135/85a | 120/70a | 135/85a |
| 160/100 | 145/90 | 145/90 | 140/85 | 145/90 |
Abbreviation: ME average, average of morning and evening BP values.
aPathologic threshold.
Although morning and evening BP are important from a prognostic perspective (see below), information on BP during everyday activities, such as work, and overnight is also helpful. Determination of BP during physical activity or home- or work-related psychological stress would require complementary use of ABPM, but semi-automatic HBPM devices are now available that measure BP at fixed intervals during sleep. These have been used successfully to monitor nighttime BP in a number of clinical trials.21–26 A 2-night schedule with 6 readings per night appears to be the minimum requirement for reliable assessment of nighttime home BP. This showed reasonable agreements with ABPM and acceptable associations with markers of preclinical organ damage.27 The reliability of nocturnal HBPM appeared to be similar when HBPM was performed at intervals based on bedtime (e.g., 2, 3, or 4 hours after a chosen bedtime) or when fixed times were chosen (e.g., 2 am, 3 am, and 4 am).28
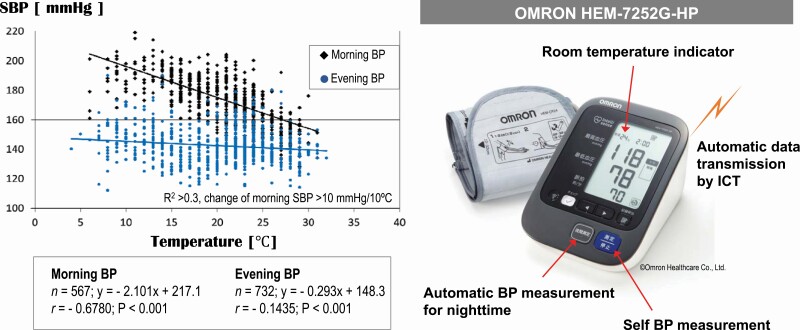
More sophisticated devices can monitor temperature as well as BP, providing data on potential factors associated with changes in BP, including environmental factors such ambient temperature (Figure 2). These devices were used in clinical trials enrolling patients with uncontrolled nocturnal hypertension,29,30 and may also have potential applications in clinical practice. Other approaches that allow assessment of nighttime BP include “trigger nighttime HBPM” where BP measurement is triggered by an episode of hypoxia or an elevation in heart rate, and beat-by-beat continuous surge BP monitoring.31,32 Combining individual time-series data with environmental factors is another novel approach to HBPM, which facilitates a more holistic approach to the measurement and management of BP.33 Technological advances such as these will increase the applicability and usefulness of HBPM for a range of different hypertension patient phenotypes.
Figure 2.
Thermosensitive morning hypertension documented using a home blood pressure (BP) monitoring device including a temperature sensor. Left: A case of thermosensitive hypertension [Measured from March 7, 2015 to December 18, 2015] (reproduced, with permission, from Kario).34
PROGNOSTIC VALUE OF HBPM
The value of HBPM is highlighted by data from multiple studies showing that home BP is an important predictor of target organ damage, and cardiovascular disease (CVD)- and stroke-related morbidity and mortality, and provides better prognostic information than office BP.35–41 Of these, the first study to show that home BP was a better predictor of mortality than screening office BP was the Ohasama study, conducted in a general population in Japan.40 The HONEST study also provides evidence that morning hypertension determined using HBPM is superior to office BP measurements for predicting the future occurrence of CV events.42,43 Furthermore, HBPM parameters have been shown to improve CV risk stratification in untreated patients with hypertension.44
An overview of studies investigating the link between HBPM parameters and target organ damage/CV risk is provided in Table 3. In addition, the sections below provide specific information relating to each key HBPM parameter.
Table 3.
Prospective studies investigating the relationship between home blood pressure monitoring parameters and the occurrence of cardiovascular events
| Study | Design and location | Population and follow-up | Outcomes |
|---|---|---|---|
| Ohasama study Ohkubo et al.40 | Prospective cohort study (Japan) |
N = 1,789 (age ≥40 y) Mean FU 6.6 y |
Relative HR (95% CI) for CV mortality associated with a 1-mm Hg increase in home BP was 1.021 (1.001–1.041; P < 0.05) |
| Kahoku-chyo study Okumiya et al.45 |
Prospective cohort study (Japan) |
N = 1,186 (mean age 73.5 y) 4-y FU |
Adjusted HR (95% CI) values for CV mortality associated with home SBP ≥135–144 and ≥145 mm Hg vs. 125–134 mm Hg (reference) were 2.3 (1.0–5.6; P < 0.05) and 2.1 (0.9–5.0; P < 0.1), respectively |
| Tsunoda et al.36 | Longitudinal, cross-sectional study (Japan) |
N = 209 (age 31–86 y) 5-y FU |
Home BP was more closely related to target organ damage (especially LVMI) than office BP |
| SHEAF study Bobrie et al.37 |
Prospective cohort study (France) |
N = 4,939 (mean age 70 ± 6.5 y) Mean FU 3.2 y |
In treated pts with HTN, each 10-mm Hg increase in home SBP increased CV event risk by 17.2% (95% CI 11.0–23.8%) and each 5-mm Hg increase in home DBP increased CV event risk by 11.7% (95% CI 5.7–18.1%); similar increases in office BP were not associated with a significant increase in CV event risk |
| Ohasama study Asayama et al.46 |
Prospective cohort study (Japan) |
N = 1,702 (age ≥40 y) Mean FU 11 y |
Home BP-based JNC-7 classification was a stronger predictor of stroke risk than clinic BP-based classification |
| PAMELA study Sega et al.47 |
Prospective cohort study (Italy) |
N = 2,051 (age 25–74 y) Mean FU 131 months |
Office, home, and ambulatory BP values showed a significant exponential direct relationship with risk of CV or all-cause death, greater for SBP vs. DBP and for nighttime BP vs. daytime BP, but not better for home or ambulatory vs. office BP; however, the slope of the relationship was progressively greater from office to home and ambulatory BP. The HR for CV mortality with a 1-mm Hg increase in BP was 1.05 (95% CI 1.04–1.06; P < 0.0001)a |
| Fagard et al.38 | Prospective cohort study (Belgium) |
N = 391 (mean age 71 y) Mean FU 10.9 y |
Adjusted relative HR for CV events associated with a 1 SD increase in home BP (22.9 mm Hg) was 1.32 (95% CI 1.06–1.64; P = 0.01); the prognostic value of home BP was better than that of office BP |
| Shimbo et al.35 | Prospective cohort study (United States) |
N = 163 (mean age 53.9 ± 14.5 y) 10-Week FU |
In a multivariate regression analysis including age, sex, BMI, office BP, awake ambulatory BP and home BP, only age, sex, and home BP were significant predictors of LVMI |
| Niiranen et al.39 | Prospective cohort study (Finland) |
N = 2,081 (age 45–74 y) Median FU 6.8 y |
Home SBP/DBP (HR 1.22/1.15, 95% CI 1.09–1.37/1.05–1.26), but not office SBP/DBP (HR 1.01/1.06, 95% CI 0.92–1.12/0.97–1.16), was a significant predictor of CV events; the only significant predictor of total mortality was home SBP (HR 1.11, 95% CI 1.01–1.23) |
| HOMED-BP study Asayama et al.48 |
Randomized intervention study (Japan) |
N = 3,518 (mean age 59.6 y) Median FU 5.3 y |
Adjusted HR (95% CI) for fatal or nonfatal CV events associated with a 1 SD (13.2 mm Hg) increase in home BP was 1.47 (1.23–1.75, P < 0.0001), irrespective of the antihypertensive used |
| J-HOP study Ishikawa et al.22 |
Prospective observational study (Japan) |
N = 854 (mean 63.0 ± 10.6 y) Mean FU 4 y |
Nighttime home SBP was more strongly related to the UACR and LVMI than nighttime ambulatory SBP (P < 0.001 for difference) |
| J-HOP study Kario et al.24 |
Prospective observational study (Japan) |
N = 2,562 (mean 64.8 ± 10.9 y) Mean FU 4 y |
Home sleep SBP values were correlated with markers of target organ damage (UACR, LVMI, baPWV, maximum carotid IMT, and plasma NT-proBNP levels (all P < 0.001); the associations between home sleep SBP and UACR, LVMI and baPWV remained significant after controlling for clinic SBP and home morning and evening SBPs (all P < 0.008) |
| Dallas Heart study Tientcheu et al.49 |
Prospective cohort study (United States) |
N = 3,027 (age 18–65 y) Median FU 9 y |
Adjusted HR (95% CI) for the risk of composite CV events in pts with masked hypertension diagnosed using HBPM vs. normotensive pts was 2.03 (1.36–3.03; P = 0.0005) |
| J-HOP study Hoshide et al.50 |
Prospective observational study (Japan) |
N = 4,310 (mean age 65 y) Mean FU 4 y |
Adjusted HR (95% CI) for the occurrence of stroke with each 10-mm Hg increase in home BP was 1.36 (1.19–1.56; P < 0.001) Morning home SBP improved the discrimination of incident stroke beyond traditional risk factors, including office BP |
| Didima study Ntineri et al.51 |
Cross-sectional population study (Greece) |
N = 694 (mean age 54.4 ± 17.7 y) Mean FU 19.1 ± 1.4 y |
Home BP was not a significant predictor of CVD events after adjustment for baseline risk factors Home SBP variability was a significant independent predictor of total mortality (adjusted HR 1.18 [95% CI 1.03–1.36] per 1 SD increase; P < 0.05) |
| J-HOP Nocturnal BP study Kario et al.26 |
Prospective cohort study (Japan) |
N = 2,547 (mean age 63 ± 10.4 y) Mean FU 7.1 ± 3.8 y |
Adjusted HR (95% CI) for CV events with a 10-mm Hg increase in nighttime home SBP was 1.201 (1.046–1.378) |
| J-HOP Nocturnal BP study Fujiwara et al.52 |
Prospective cohort study (Japan) |
N = 2,547 (mean age 63 ± 10.4 y) Mean FU 7.1 ± 3.8 y |
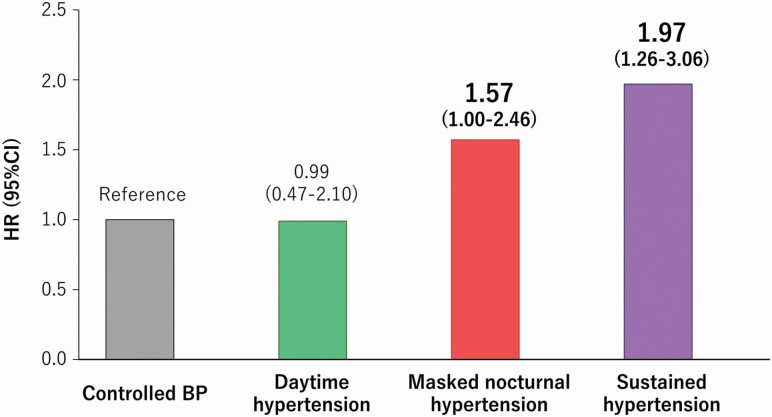
The cumulative incidence of CVD events was higher in pts with masked nocturnal HTN and sustained HTN (both based on HBPM) than in those with controlled BP Masked nocturnal HTN (adjusted HR [95% CI] 1.57 [1.00–2.46]) and sustained HTN (1.97 [1.263.06]) were associated with an increased risk of CVD events |
| J-HOP study Mokwatsi et al.53 |
Prospective observational study (Japan) |
N = 1,005 (mean age 63.2 ± 10.8 y) Mean FU 7.6 ± 3.4 y |
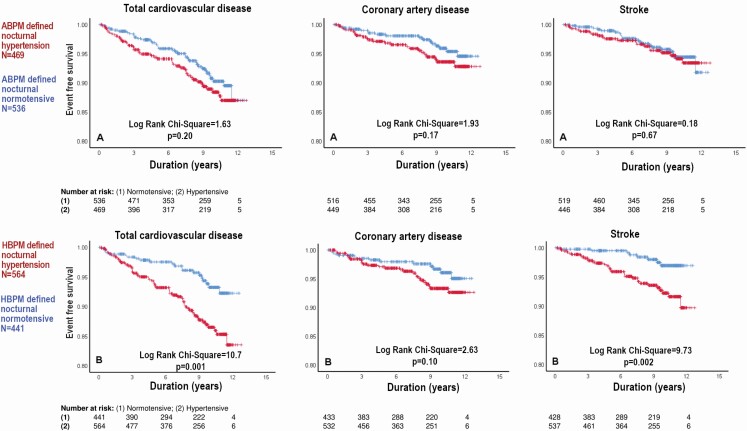
Adjusted HR (95% CI) for the risk of total CVD events (CAD + stroke) was 1.78 (1.00–3.15; P < 0.01) for HBPM-defined nocturnal HTN and 1.24 (0.75–2.06) for ABPM-defined nocturnal HTN Adjusted HR (95% CI) for the risk of stroke was 2.65 (1.14–6.20; P < 0.05) for HBPM-defined nocturnal HTN and 1.08 (0.55–2.15) for ABPM-defined nocturnal HTN |
Abbreviations: APBM, ambulatory blood pressure monitoring; baPWV, brachial-ankle pulse wave velocity; BMI, body mass index; BP, blood pressure; CAD, coronary artery disease; CI, confidence interval; CV, cardiovascular; CVD, cardiovascular disease; DBP, diastolic BP; FU, follow-up; HBPM, home blood pressure monitoring; HF, heart failure; HR, hazard ratio; HTN, hypertension; IMT, intima–media thickness; JNC-7, Seventh Joint National Committee; LVMI, left ventricular mass index; MH, masked hypertension; NT-proBNP, amino terminal pro B-type natriuretic peptide; SBP, systolic blood pressure; UACR, urinary albumin–creatinine ratio; y, years.
aCalculated from presented data of beta coefficient and SE in this study.
Morning home BP
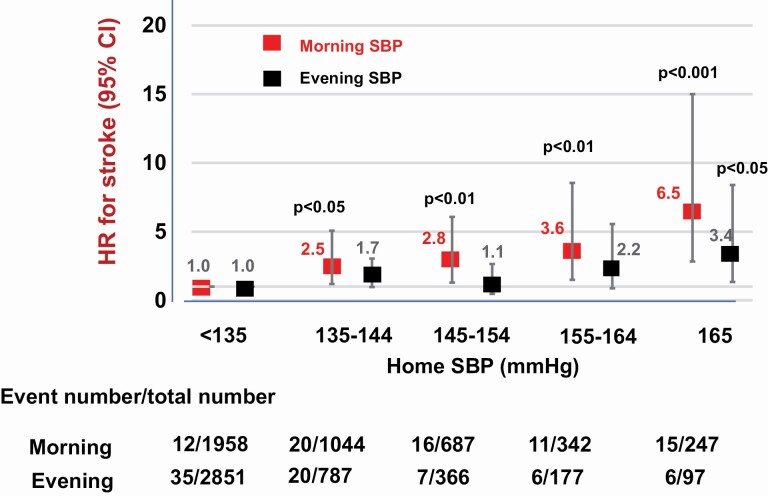
Even when office BP is normal, patients with masked hypertension and high morning systolic BP (SBP) have a high risk of CV events.42 When detected by HBPM or ABPM, the presence of masked hypertension and masked uncontrolled hypertension is associated with poor clinical outcomes.54 Morning home SBP ≥155 mm Hg has been shown to increase the risk of developing coronary artery disease by more than 6-fold, almost twice the risk associated with office SBP ≥160 mm Hg.43 Morning home BP has also been shown to have better reproducibility than ambulatory BP measurements, and a stronger correlation with indices of vascular function.55 Furthermore, morning home SBP improves the discrimination of incident stroke over and above traditional risk factors (including office BP) and was a better predictor of stroke risk than evening home BP (Figure 3).50 This suggests that morning home SBP should be monitored and controlled to ensure optimal protection against CVD and stroke in clinical practice. Guideline recommendations note that morning home BP should be measured prior to antihypertensive drug dosing.7,9,10
Figure 3.
Association between home blood pressure and stroke risk in the J-HOP study (adapted, with permission, from Hoshide et al.).50 Abbreviations: CI, confidence interval; HR, hazard ratio; SBP, systolic blood pressure.
Nighttime home BP
Control of nocturnal BP is also an important part of CV risk management strategies,34,56 and nocturnal hypertension is common in hypertensive patients with comorbidities such as diabetes mellitus, chronic kidney disease, or obstructive sleep apnea. Until relatively recently, the only option for measuring nighttime BP was ABPM. However, new HBPM devices have been developed that provide another option for nighttime BP measurement.32,57 These have been shown to provide similar BP values to ABPM, and similar associations with target organ damage.58
One of the first studies to highlight the importance of nighttime BP was the Ohasama study, which showed that nighttime BP had a better prognostic value than daytime BP.59 In a Cox model including both nighttime and daytime SBP, only nighttime BP was a significant predictor of CV mortality risk over 10.8 years of follow-up.59 Another recent study also documented the importance of nighttime BP levels and a riser pattern of nighttime BP, both of which were independently associated with the total CV event rate.60 In the J-HOP study, home sleep SBP values were correlated with several manifestations of CV target organ damage, including the left ventricular mass index, urinary albumin–creatinine ratio, arterial stiffness parameters, amino terminal pro B-type natriuretic peptide levels, and these associations persisted after adjustment for clinic SBP and morning and evening home SBP.22,24 Furthermore, the J-HOP Nocturnal BP study identified a significant increase in CV risk with each 10-mm Hg increase in nighttime home SBP.26 In addition, the CV event risk associated with masked nocturnal hypertension was nearly as high as that associated with sustained hypertension (Figure 4).52
Figure 4.
Risk of cardiovascular events based on type of hypertension (adapted, with permission, from Fujiwara et al.).52 Abbreviations: BP, blood pressure; CI, confidence interval; HR, hazard ratio.
Recent data highlight the importance of nocturnal hypertension measured using HBPM rather than ABPM. Data from the J-HOP study were used to compare the prognostic power of nocturnal hypertension detected by HBPM vs. ABPM for predicting future CV events.53 Home nighttime SBP was significantly higher than ambulatory nighttime SBP (123.0 ± 14.6 vs. 120.3 ± 14.4 mm Hg, P < 0.001). In addition, nocturnal hypertension detected using HBPM (home SBP >120 mm Hg) was significantly associated with an increased risk of future CV events, independent of office SBP (hazard ratio [95% confidence interval] for CAD + stroke, 1.78 [1.00–3.15] and for stroke only, 2.65 [1.14–6.20]), whereas no such association was seen for nocturnal hypertension defined and detected using ABPM (Figure 5).53
Figure 5.
Association between nocturnal hypertension defined using ambulatory (a) vs. home (b) blood pressure and cardiovascular event risk in the J-HOP study (reproduced, with permission, from Mokwatsi et al.).53
Home BP variability
There are a variety of ways that BP variability can be defined, including beat-by-beat, daily, seasonal, and long term. Morning, evening, and nocturnal hypertension, the morning BP surge and nocturnal dipping are all examples of circadian variation in BP. There is good agreement between HBPM and ABPM for detection of patients with a nondipping nocturnal BP profile.61 HBPM can also be used to detect long-term and seasonal variations in BP.19,62–65 Seasonal- and temperature-related variations in BP could become increasingly relevant in the current setting of increased climate change, and have the potential to change the epidemiology of hypertension.66
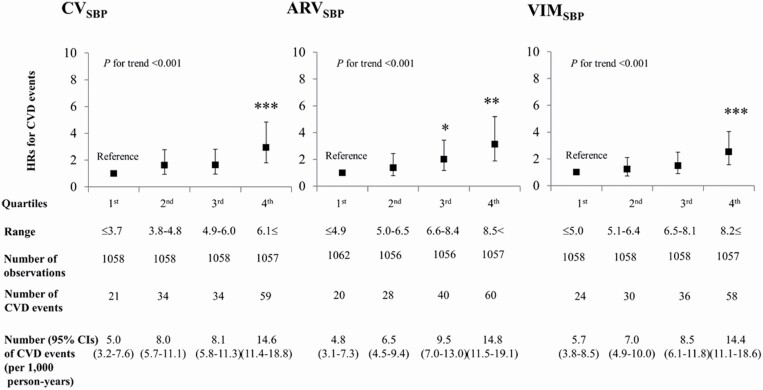
Variability in home BP has been shown to be predictive of both stroke and CV events,67,68 and is a key component of the systemic hemodynamic atherothrombotic syndrome.69 Even variability across just a few home BP measurements is able to predict the occurrence of total and nonfatal CV events as well as total mortality.68 Day-to-day variability in home BP also predicts hypertensive target organ damage.70–75 Using data from the J-HOP study, several measures of short-term BP variability were found to be significantly associated with CVD risk independently of home SBP, circulating B-type natriuretic peptide levels and the urinary albumin–creatinine ratio, with risk increasing as variability increased (Figure 6).76
Figure 6.
Cardiovascular disease risk by quartiles of home blood pressure variability (reproduced, with permission, from Hoshide et al.).76 Abbreviations: ARV, average real variability; CI, confidence interval; CV, coefficient of variation; CVD, cardiovascular disease; SBP, systolic blood pressure; VIM, variability independent of the mean. *P < 0.05 vs. reference group; **P < 0.01 vs. reference group; ***P < 0.001 vs. reference group.
MANAGEMENT OF ANTIHYPERTENSIVE THERAPY
HBPM is a practical way to determine and monitor BP during the day-to-day management of hypertension, providing real-time information on antihypertensive treatment-related changes in BP. The ability of HBPM to provide repeated measures under standard conditions at specific times for an extended period of time makes it ideally suited for evaluating the efficacy of pharmacological antihypertensive therapy. Furthermore, using HBPM as part of the routine management of patients with hypertension might optimize reductions in BP, improve BP control, and reduce target organ damage and CVD risk. Another potential benefit of HBPM is that it facilitates education of patients about their disease, and its management and control, thus encouraging patient-centric care.77
BP reduction and control
Nocturnal home BP monitoring documented significant reductions in nighttime home SBP during treatment with angiotensin receptor blocker-based antihypertensive therapy in Japanese patients with nocturnal hypertension.30 HBPM also showed that morning home BP was significantly decreased in hypertensive patients during angiotensin receptor blocker-based therapy.42,78
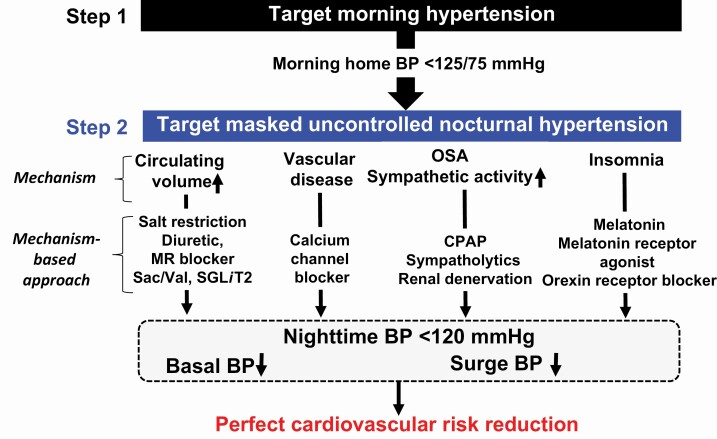
Data from several meta-analyses show that use of HBPM during antihypertensive therapy is associated with significant decreases in SBP and DBP compared with usual care,79–82 and with reductions in antihypertensive medication use and therapeutic inertia, defined as unchanged medication despite elevated BP.82 Thus, HBPM plays a central role in a stepwise, personalized, optimal 24-hour BP control approach to the management of hypertension (Figure 7).32
Figure 7.
Mechanism-based STEpwise-personalized 24-hour blood pressure control approach (STEP24) (adapted, with permission, from Kario).32 Abbreviations: BP, blood pressure; CPAP, continuous positive airway pressure; MR, mineralocorticoid receptor; OSA, obstructive sleep apnea; Sac/Val, sacubitril/valsartan; SGLT2i, sodium glucose cotransporter 2 inhibitor.
CV event risk
The association between HBPM parameters and risk of CVD events and mortality supports the use of this approach to monitoring BP and antihypertensive therapy in clinical practice.77 The Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP) trial was the first study to evaluate outcomes in patients with hypertension whose antihypertensive therapy was guided by self-measured home BP.48 The risk of CV death plus stroke and myocardial infarction (the primary endpoint) independently increased by 41% and 47% for each 1 SD increase in baseline and follow-up home SBP, respectively, irrespective of the antihypertensive used.48 This suggests that reducing home BP is an important goal in patients with hypertension. In the HOMED-BP study, the 5-year risk of primary endpoint events was ≤1% if the home SBP during treatment was ≤131.6 mm Hg,48 which indicates that the guideline targets for home BP should be sufficient to reduce CVD risk.
DIGITAL MANAGEMENT OF HYPERTENSION AND NEW DEVELOPMENTS
The usefulness of HBPM can be enhanced by the addition of telemonitoring, whereby patients receive feedback from healthcare professionals based on BP readings sent electronically.83 Incorporation of telemedicine approaches has been shown to significantly reduce both SBP and diastolic BP, and improve BP control, compared with usual care.84–87 In addition, telemedicine allows provision of effective healthcare services without close interaction, making it ideally suited to maintain effective disease management under pandemic or natural disaster conditions.83 A telemedicine-based strategy was successfully used to facilitate digital management of hypertension based on individual big data in the aftermath of the Great East Japan Earthquake in March 2011.88 A web-based HBPM system enabled effective monitoring and strict control of home BP and minimized seasonal variations in BP over the months and years after the earthquake.88 A comprehensive digital approach to the management of hypertension (the HERB system) is currently under evaluation in a randomized clinical study (the HERB-DH1 trial).89 Adults with essential hypertension are being managed using the HERB system and standard lifestyle interventions or lifestyle interventions alone. The HERB system app includes an algorithm designed to promote lifestyle modifications in conjunction with medically validated nonpharmacological interventions. The primary endpoint is the change in 24-hour SBP from baseline to 12 weeks and the results are expected in early 2021.89
Another promising strategy for HBPM is the use of wearable devices that allow cuff-less, noninvasive, beat-by-beat monitoring of BP. A number of these devices are currently in development by companies with a proven track record in the hypertension field. The development and use of wearable BP monitoring devices were recently reviewed in detail.90 Several wearable devices have been validated using currently accepted clinical standards91,92 and one has also shown good agreement with ABPM.93 These devices could also provide data on environmental conditions, and may also be useful for detecting arrhythmias, such as atrial fibrillation.94 Further research and developments in this area could improve the accessibility and acceptability of HBPM.
The data provided by HBPM and other wearable hypertension monitoring devices could help inform artificial intelligence strategies to improve the diagnosis and treatment of hypertension. Several studies have investigated these approaches. One machine learning model based on data from 18,258 individuals was able to predict the development of hypertension in a general population.95 Another artificial intelligence-based prediction model based on time-series BP data and related contextual information used multi-input multi-output deep neural networks to predict both mean BP and BP variability.96 These approaches could identify patients at risk of developing hypertension, and then help predict BP values and variability to allow the most appropriate therapeutic strategy for each patient.
PERSPECTIVES
HBPM is an important and practical tool for the out-of-office measurement of BP. When performed according to current guidelines and using a validated device, it provides similar data to ABPM but is more widely available and convenient for patients. The introduction of wearable HBPM devices into clinical practice would be expected to make HBPM accessible to a larger number of patients, with the potential to replace ABPM as the out-of-office BP monitoring tool of choice. In addition, devices and systems with additional features such as nocturnal home BP monitoring, and monitoring of temperature and environmental factors alongside home BP, will facilitate a more comprehensive approach to the diagnosis and treatment of hypertension, and evaluation of CV risk. However, it is also important to note that current use and awareness of HBPM varies between regions and countries, and between specialists and general practitioners.97 There are also a number of challenges that need to be overcome to facilitate the widespread implementation of an HBPM-based approach to hypertension management. These include a lack of awareness about the clinical value of HBPM, insufficient knowledge about HBPM best practices, and a lack of resources (both time and equipment).97 Nevertheless, a substantial body of evidence for the prognostic value of home BP measurements highlight the importance of this approach to the management of CV risk factors in patients with hypertension. HBPM can play a key role in anticipation medicine strategies designed to identify increasing risk and predict the onset of CV events based on a series of data collected over time, allowing proactive interventions to reduce risk and eliminate events. Current developments and future advances in HBPM technologies, along with targeted training and education to support their use, will see HBPM continue to feature as an essential component of the continuum of care for hypertension, including diagnosis and both short- and long-term monitoring of the response to antihypertensive therapy.
ACKNOWLEDGMENTS
Medical writing assistance was provided by Nicola Ryan, independent medical writer, funded by Jichi Medical University.
DISCLOSURE
K. Kario has received research grants from Omron Healthcare and A&D.
REFERENCES
- 1. Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, O’Brien E, Ohkubo T, Padfield P, Palatini P, Pickering TG, Redon J, Revera M, Ruilope LM, Shennan A, Staessen JA, Tisler A, Waeber B, Zanchetti A, Mancia G; ESH Working Group on Blood Pressure Monitoring . European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens 2010; 24:779–785. [DOI] [PubMed] [Google Scholar]
- 2. Kario K. Home blood pressure-guided anticipation management of hypertension: effective to the gap between the guidelines and the individualized medicine. Curr Hypertens Rev 2019; 15:2–6. [DOI] [PubMed] [Google Scholar]
- 3. Kario K, Thijs L, Staessen JA. Blood pressure measurement and treatment decisions. Circ Res 2019; 124:990–1008. [DOI] [PubMed] [Google Scholar]
- 4. Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y; European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability . European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 2014; 32:1359–1366. [DOI] [PubMed] [Google Scholar]
- 5. Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, Myers MG, Ogedegbe G, Schwartz JE, Townsend RR, Urbina EM, Viera AJ, White WB, Wright JT Jr. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 2019; 73:e35–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kario K, Shimbo D, Hoshide S, Wang JG, Asayama K, Ohkubo T, Imai Y, McManus RJ, Kollias A, Niiranen TJ, Parati G, Williams B, Weber MA, Vongpatanasin W, Muntner P, Stergiou GS. Emergence of home blood pressure-guided management of hypertension based on global evidence. Hypertension 2019; 74:229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, Ito M, Ito S, Iwashima Y, Kai H, Kamide K, Kanno Y, Kashihara N, Kawano Y, Kikuchi T, Kitamura K, Kitazono T, Kohara K, Kudo M, Kumagai H, Matsumura K, Matsuura H, Miura K, Mukoyama M, Nakamura S, Ohkubo T, Ohya Y, Okura T, Rakugi H, Saitoh S, Shibata H, Shimosawa T, Suzuki H, Takahashi S, Tamura K, Tomiyama H, Tsuchihashi T, Ueda S, Uehara Y, Urata H, Hirawa N. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res 2019; 42:1235–1481. [DOI] [PubMed] [Google Scholar]
- 8. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, Wainford RD, Williams B, Schutte AE. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension 2020; 75:1334–1357. [DOI] [PubMed] [Google Scholar]
- 9. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018; 71:2199–2269.29146533 [Google Scholar]
- 10. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group . 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018; 39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 11. Joint Committee for Guideline Revision. 2018 Chinese guidelines for prevention and treatment of hypertension—a report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol 2019; 16:182–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chiang CE, Wang TD, Ueng KC, Lin TH, Yeh HI, Chen CY, Wu YJ, Tsai WC, Chao TH, Chen CH, Chu PH, Chao CL, Liu PY, Sung SH, Cheng HM, Wang KL, Li YH, Chiang FT, Chen JH, Chen WJ, Yeh SJ, Lin SJ. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc 2015; 78:1–47. [DOI] [PubMed] [Google Scholar]
- 13. Lee HY, Shin J, Kim GH, Park S, Ihm SH, Kim HC, Kim KI, Kim JH, Lee JH, Park JM, Pyun WB, Chae SC. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens 2019; 25:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kario K, Park S, Chia YC, Sukonthasarn A, Turana Y, Shin J, Chen CH, Buranakitjaroen P, Divinagracia R, Nailes J, Hoshide S, Siddique S, Sison J, Soenarta AA, Sogunuru GP, Tay JC, Teo BW, Zhang YQ, Van Minh H, Tomitani N, Kabutoya T, Verma N, Wang TD, Wang JG. 2020 Consensus summary on the management of hypertension in Asia from the HOPE Asia Network. J Clin Hypertens (Greenwich) 2020; 22:351–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kario K, Tomitani N, Buranakitjaroen P, Chia YC, Park S, Chen CH, Divinagracia R, Shin J, Siddique S, Sison J, Ann Soenarta A, Sogunuru GP, Tay JC, Turana Y, Zhang Y, Nailes J, Wanthong S, Hoshide S, Matsushita N, Kanegae H, Wang JG; HOPE Asia Network . Home blood pressure control status in 2017–2018 for hypertension specialist centers in Asia: results of the Asia BP@Home study. J Clin Hypertens (Greenwich) 2018; 20:1686–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Park S, Buranakitjaroen P, Chen CH, Chia YC, Divinagracia R, Hoshide S, Shin J, Siddique S, Sison J, Soenarta AA, Sogunuru GP, Tay JC, Turana Y, Wang JG, Zhang Y, Kario K; HOPE Asia Network . Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network. J Hum Hypertens 2018; 32:249–258. [DOI] [PubMed] [Google Scholar]
- 17. Wang JG, Bu PL, Chen LY, Chen X, Chen YY, Cheng WL, Chu SL, Cui ZQ, Dai QY, Feng YQ, Jiang XJ, Jiang YN, Li WH, Li Y, Li Y, Lin JX, Liu J, Mu JJ, Peng YX, Song L, Sun NL, Wang Y, Xi Y, Xie LD, Xue H, Yu J, Yu W, Zhang YQ, Zhu ZM. 2019 Chinese Hypertension League guidelines on home blood pressure monitoring. J Clin Hypertens (Greenwich) 2020; 22:378–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kario K, Park S, Buranakitjaroen P, Chia YC, Chen CH, Divinagracia R, Hoshide S, Shin J, Siddique S, Sison J, Soenarta AA, Sogunuru GP, Tay JC, Turana Y, Wong L, Zhang Y, Wang JG. Guidance on home blood pressure monitoring: a statement of the HOPE Asia Network. J Clin Hypertens (Greenwich) 2018; 20:456–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Narita K, Hoshide S, Fujiwara T, Kanegae H, Kario K. Seasonal variation of home blood pressure and its association with target organ damage: the J-HOP Study (Japan Morning Surge-Home Blood Pressure). Am J Hypertens 2020; 33:620–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tomitani N, Kanegae H, Suzuki Y, Kuwabara M, Kario K. Stress-induced blood pressure elevation self-measured by a wearable watch-type device. Am J Hypertens 2021; 34: 377–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hoshide S, Kario K, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, Matsui Y, Nakamura A, Fukutomi M, Eguchi K, Ishikawa J; J-HOP Study Group . Association of morning and evening blood pressure at home with asymptomatic organ damage in the J-HOP Study. Am J Hypertens 2014; 27:939–947. [DOI] [PubMed] [Google Scholar]
- 22. Ishikawa J, Hoshide S, Eguchi K, Ishikawa S, Shimada K, Kario K; Japan Morning Surge-Home Blood Pressure Study Investigators Group . Nighttime home blood pressure and the risk of hypertensive target organ damage. Hypertension 2012; 60:921–928. [DOI] [PubMed] [Google Scholar]
- 23. Ishikawa J, Shimizu M, Sugiyama Edison E, Yano Y, Hoshide S, Eguchi K, Kario K; J-TOP (Japan Morning Surge-Target Organ Protection) Study Investigators Group . Assessment of the reductions in night-time blood pressure and dipping induced by antihypertensive medication using a home blood pressure monitor. J Hypertens 2014; 32:82–89. [DOI] [PubMed] [Google Scholar]
- 24. Kario K, Hoshide S, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, Yano Y, Eguchi K, Matsui Y, Shimizu M, Ishikawa J, Ishikawa S; J-HOP study group . Sleep blood pressure self-measured at home as a novel determinant of organ damage: Japan Morning Surge Home Blood Pressure (J-HOP) Study. J Clin Hypertens (Greenwich) 2015; 17:340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kario K, Hoshide S, Shimizu M, Yano Y, Eguchi K, Ishikawa J, Ishikawa S, Shimada K. Effect of dosing time of angiotensin II receptor blockade titrated by self-measured blood pressure recordings on cardiorenal protection in hypertensives: the Japan Morning Surge-Target Organ Protection (J-TOP) study. J Hypertens 2010; 28:1574–1583. [DOI] [PubMed] [Google Scholar]
- 26. Kario K, Kanegae H, Tomitani N, Okawara Y, Fujiwara T, Yano Y, Hoshide S. Nighttime blood pressure measured by home blood pressure monitoring as an independent predictor of cardiovascular events in general practice. Hypertension 2019; 73:1240–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kollias A, Andreadis E, Agaliotis G, Kolyvas GN, Achimastos A, Stergiou GS. The optimal night-time home blood pressure monitoring schedule: agreement with ambulatory blood pressure and association with organ damage. J Hypertens 2018; 36:243–249. [DOI] [PubMed] [Google Scholar]
- 28. Fujiwara T, Nishizawa M, Hoshide S, Kanegae H, Kario K. Comparison of different schedules of nocturnal home blood pressure measurement using an information/communication technology-based device in hypertensive patients. J Clin Hypertens (Greenwich) 2018; 20:1633–1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fujiwara T, Tomitani N, Kanegae H, Kario K. Comparative effects of valsartan plus either cilnidipine or hydrochlorothiazide on home morning blood pressure surge evaluated by information and communication technology-based nocturnal home blood pressure monitoring. J Clin Hypertens (Greenwich) 2018; 20:159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kario K, Tomitani N, Kanegae H, Ishii H, Uchiyama K, Yamagiwa K, Shiraiwa T, Katsuya T, Yoshida T, Kanda K, Hasegawa S, Hoshide S. Comparative effects of an angiotensin II receptor blocker (ARB)/diuretic vs. ARB/calcium-channel blocker combination on uncontrolled nocturnal hypertension evaluated by information and communication technology-based nocturnal home blood pressure monitoring—the NOCTURNE Study. Circ J 2017; 81:948–957. [DOI] [PubMed] [Google Scholar]
- 31. Kario K. Evidence and perspectives on the 24-hour management of hypertension: hemodynamic biomarker-initiated ‘anticipation medicine’ for zero cardiovascular event. Prog Cardiovasc Dis 2016; 59:262–281. [DOI] [PubMed] [Google Scholar]
- 32. Kario K. Nocturnal hypertension: new technology and evidence. Hypertension 2018; 71:997–1009. [DOI] [PubMed] [Google Scholar]
- 33. Kario K, Tomitani N, Kanegae H, Yasui N, Nagai R, Harada H. The further development of out-of-office BP monitoring: Japan’s ImPACT Program Project’s achievements, impact, and direction. J Clin Hypertens (Greenwich) 2019; 21:344–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kario K. Essential Manual on Perfect 24-Hour Blood Pressure Management from Morning to Nocturnal Hypertension: Up-to-Date for Anticipation Medicine. Wiley Publishing: Japan, 2018. [Google Scholar]
- 35. Shimbo D, Pickering TG, Spruill TM, Abraham D, Schwartz JE, Gerin W. Relative utility of home, ambulatory, and office blood pressures in the prediction of end-organ damage. Am J Hypertens 2007; 20:476–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tsunoda S, Kawano Y, Horio T, Okuda N, Takishita S. Relationship between home blood pressure and longitudinal changes in target organ damage in treated hypertensive patients. Hypertens Res 2002; 25:167–173. [DOI] [PubMed] [Google Scholar]
- 37. Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion JM. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA 2004; 291:1342–1349. [DOI] [PubMed] [Google Scholar]
- 38. Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens 2005; 19:801–807. [DOI] [PubMed] [Google Scholar]
- 39. Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension 2010; 55:1346–1351. [DOI] [PubMed] [Google Scholar]
- 40. Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16:971–975. [DOI] [PubMed] [Google Scholar]
- 41. Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens 2012; 30:1289–1299. [DOI] [PubMed] [Google Scholar]
- 42. Kario K, Saito I, Kushiro T, Teramukai S, Ishikawa Y, Mori Y, Kobayashi F, Shimada K. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension 2014; 64:989–996. [DOI] [PubMed] [Google Scholar]
- 43. Kario K, Saito I, Kushiro T, Teramukai S, Tomono Y, Okuda Y, Shimada K. Morning home blood pressure is a strong predictor of coronary artery disease: the HONEST Study. J Am Coll Cardiol 2016; 67:1519–1527. [DOI] [PubMed] [Google Scholar]
- 44. Asayama K, Thijs L, Brguljan-Hitij J, Niiranen TJ, Hozawa A, Boggia J, Aparicio LS, Hara A, Johansson JK, Ohkubo T, Tzourio C, Stergiou GS, Sandoya E, Tsuji I, Jula AM, Imai Y, Staessen JA; International Database of Home Blood Pressure in Relation to Cardiovascular Outcome (IDHOCO) investigators . Risk stratification by self-measured home blood pressure across categories of conventional blood pressure: a participant-level meta-analysis. PLoS Med 2014; 11:e1001591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Okumiya K, Matsubayashi K, Wada T, Fujisawa M, Osaki Y, Doi Y, Yasuda N, Ozawa T. A U-shaped association between home systolic blood pressure and four-year mortality in community-dwelling older men. J Am Geriatr Soc 1999; 47:1415–1421. [DOI] [PubMed] [Google Scholar]
- 46. Asayama K, Ohkubo T, Kikuya M, Metoki H, Hoshi H, Hashimoto J, Totsune K, Satoh H, Imai Y. Prediction of stroke by self-measurement of blood pressure at home versus casual screening blood pressure measurement in relation to the Joint National Committee 7 classification: the Ohasama study. Stroke 2004; 35:2356–2361. [DOI] [PubMed] [Google Scholar]
- 47. Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, Mancia G. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation 2005; 111:1777–1783. [DOI] [PubMed] [Google Scholar]
- 48. Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, Thijs L, Staessen JA, Imai Y; Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP) . Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res 2012; 35:1102–1110.22895063 [Google Scholar]
- 49. Tientcheu D, Ayers C, Das SR, McGuire DK, de Lemos JA, Khera A, Kaplan N, Victor R, Vongpatanasin W. Target organ complications and cardiovascular events associated with masked hypertension and white-coat hypertension: analysis from the Dallas Heart Study. J Am Coll Cardiol 2015; 66:2159–2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, Matsui Y, Nakamura A, Fukutomi M, Eguchi K, Ishikawa J, Kario K; J-HOP Study Group . Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: the Japan Morning Surge-Home Blood Pressure Study. Hypertension 2016; 68:54–61. [DOI] [PubMed] [Google Scholar]
- 51. Ntineri A, Kalogeropoulos PG, Kyriakoulis KG, Aissopou EK, Thomopoulou G, Kollias A, Stergiou GS. Prognostic value of average home blood pressure and variability: 19-year follow-up of the Didima study. J Hypertens 2018; 36:69–76. [DOI] [PubMed] [Google Scholar]
- 52. Fujiwara T, Hoshide S, Kanegae H, Kario K. Cardiovascular event risks associated with masked nocturnal hypertension defined by home blood pressure monitoring in the J-HOP nocturnal blood pressure study. Hypertension 2020; 76:259–266. [DOI] [PubMed] [Google Scholar]
- 53. Mokwatsi GG, Hoshide S, Kanegae H, Fujiwara T, Negishi K, Schutte AE, Kario K. Direct comparison of home versus ambulatory defined nocturnal hypertension for predicting cardiovascular events: the Japan Morning Surge-Home Blood Pressure (J-HOP) Study. Hypertension 2020; 76:554–561. [DOI] [PubMed] [Google Scholar]
- 54. Zhang DY, Guo QH, An DW, Li Y, Wang JG. A comparative meta-analysis of prospective observational studies on masked hypertension and masked uncontrolled hypertension defined by ambulatory and home blood pressure. J Hypertens 2019; 37:1775–1785. [DOI] [PubMed] [Google Scholar]
- 55. Guo QH, Cheng YB, Zhang DY, Wang Y, Huang QF, Sheng CS, Xu TY, Li Y, Wang JG. Comparison between home and ambulatory morning blood pressure and morning hypertension in their reproducibility and associations with vascular injury. Hypertension 2019; 74:137–144. [DOI] [PubMed] [Google Scholar]
- 56. Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension 2011; 57:3–10. [DOI] [PubMed] [Google Scholar]
- 57. Asayama K, Fujiwara T, Hoshide S, Ohkubo T, Kario K, Stergiou GS, Parati G, White WB, Weber MA, Imai Y; International Expert Group of Nocturnal Home Blood Pressure . Nocturnal blood pressure measured by home devices: evidence and perspective for clinical application. J Hypertens 2019; 37:905–916. [DOI] [PubMed] [Google Scholar]
- 58. Kollias A, Ntineri A, Stergiou GS. Association of night-time home blood pressure with night-time ambulatory blood pressure and target-organ damage: a systematic review and meta-analysis. J Hypertens 2017; 35:442–452. [DOI] [PubMed] [Google Scholar]
- 59. Kikuya M, Ohkubo T, Asayama K, Metoki H, Obara T, Saito S, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality: the Ohasama study. Hypertension 2005; 45:240–245. [DOI] [PubMed] [Google Scholar]
- 60. Kario K, Hoshide S, Mizuno H, Kabutoya T, Nishizawa M, Yoshida T, Abe H, Katsuya T, Fujita Y, Okazaki O, Yano Y, Tomitani N, Kanegae H; JAMP Study Group . Nighttime blood pressure phenotype and cardiovascular prognosis: practitioner-based nationwide JAMP Study. Circulation 2020; 142:1810–1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Stergiou GS, Nasothimiou EG, Destounis A, Poulidakis E, Evagelou I, Tzamouranis D. Assessment of the diurnal blood pressure profile and detection of non-dippers based on home or ambulatory monitoring. Am J Hypertens 2012; 25:974–978. [DOI] [PubMed] [Google Scholar]
- 62. Imai Y, Munakata M, Tsuji I, Ohkubo T, Satoh H, Yoshino H, Watanabe N, Nishiyama A, Onodera N, Kato J, Sekino M, Aihara A, Kasai Y, Abe K. Seasonal variation in blood pressure in normotensive women studied by home measurements. Clin Sci (Lond) 1996; 90:55–60. [DOI] [PubMed] [Google Scholar]
- 63. Hanazawa T, Asayama K, Watabe D, Tanabe A, Satoh M, Inoue R, Hara A, Obara T, Kikuya M, Nomura K, Metoki H, Imai Y, Ohkubo T. Association between amplitude of seasonal variation in self-measured home blood pressure and cardiovascular outcomes: HOMED-BP (Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure) Study. J Am Heart Assoc 2018; 7:e008509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Umishio W, Ikaga T, Kario K, Fujino Y, Hoshi T, Ando S, Suzuki M, Yoshimura T, Yoshino H, Murakami S; SWH Survey Group . Cross-sectional analysis of the relationship between home blood pressure and indoor temperature in winter: a nationwide smart wellness housing survey in Japan. Hypertension 2019; 74:756–766. [DOI] [PubMed] [Google Scholar]
- 65. Umishio W, Ikaga T, Kario K, Fujino Y, Hoshi T, Ando S, Suzuki M, Yoshimura T, Yoshino H, Murakami S; Smart Wellness Housing survey group . Intervention study of the effect of insulation retrofitting on home blood pressure in winter: a nationwide Smart Wellness Housing survey. J Hypertens 2020; 38:2510–2518. [DOI] [PubMed] [Google Scholar]
- 66. Park S, Kario K, Chia YC, Turana Y, Chen CH, Buranakitjaroen P, Nailes J, Hoshide S, Siddique S, Sison J, Soenarta AA, Sogunuru GP, Tay JC, Teo BW, Zhang YQ, Shin J, Van Minh H, Tomitani N, Kabutoya T, Sukonthasarn A, Verma N, Wang TD, Wang JG; HOPE Asia Network . The influence of the ambient temperature on blood pressure and how it will affect the epidemiology of hypertension in Asia. J Clin Hypertens (Greenwich) 2020; 22:438–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kikuya M, Ohkubo T, Metoki H, Asayama K, Hara A, Obara T, Inoue R, Hoshi H, Hashimoto J, Totsune K, Satoh H, Imai Y. Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension 2008; 52:1045–1050. [DOI] [PubMed] [Google Scholar]
- 68. Johansson JK, Niiranen TJ, Puukka PJ, Jula AM. Prognostic value of the variability in home-measured blood pressure and heart rate: the Finn-Home Study. Hypertension 2012; 59:212–218. [DOI] [PubMed] [Google Scholar]
- 69. Kario K, Chirinos JA, Townsend RR, Weber MA, Scuteri A, Avolio A, Hoshide S, Kabutoya T, Tomiyama H, Node K, Ohishi M, Ito S, Kishi T, Rakugi H, Li Y, Chen CH, Park JB, Wang JG. Systemic hemodynamic atherothrombotic syndrome (SHATS)—coupling vascular disease and blood pressure variability: proposed concept from pulse of Asia. Prog Cardiovasc Dis 2020; 63:22–32. [DOI] [PubMed] [Google Scholar]
- 70. Ushigome E, Fukui M, Hamaguchi M, Senmaru T, Sakabe K, Tanaka M, Yamazaki M, Hasegawa G, Nakamura N. The coefficient variation of home blood pressure is a novel factor associated with macroalbuminuria in type 2 diabetes mellitus. Hypertens Res 2011; 34:1271–1275. [DOI] [PubMed] [Google Scholar]
- 71. Matsui Y, Ishikawa J, Eguchi K, Shibasaki S, Shimada K, Kario K. Maximum value of home blood pressure: a novel indicator of target organ damage in hypertension. Hypertension 2011; 57:1087–1093. [DOI] [PubMed] [Google Scholar]
- 72. Godai K, Kabayama M, Gondo Y, Yasumoto S, Sekiguchi T, Noma T, Tanaka K, Kiyoshige E, Akagi Y, Sugimoto K, Akasaka H, Takami Y, Takeya Y, Yamamoto K, Arai Y, Masui Y, Ishizaki T, Ikebe K, Satoh M, Asayama K, Ohkubo T, Rakugi H, Kamide K; SONIC study group . Day-to-day blood pressure variability is associated with lower cognitive performance among the Japanese community-dwelling oldest-old population: the SONIC study. Hypertens Res 2020; 43:404–411. [DOI] [PubMed] [Google Scholar]
- 73. Ishiyama Y, Hoshide S, Kanegae H, Kario K. Increased arterial stiffness amplifies the association between home blood pressure variability and cardiac overload: the J-HOP Study. Hypertension 2020; 75:1600–1606. [DOI] [PubMed] [Google Scholar]
- 74. Kitagawa N, Ushigome E, Matsumoto S, Oyabu C, Ushigome H, Yokota I, Asano M, Tanaka M, Yamazaki M, Fukui M. Prognostic significance of home pulse pressure for progression of diabetic nephropathy: KAMOGAWA-HBP Study. Hypertens Res 2018; 41:363–371. [DOI] [PubMed] [Google Scholar]
- 75. Suzuki D, Hoshide S, Kario K. Associations between day-by-day home blood pressure variability and renal function and albuminuria in patients with and without diabetes. Am J Hypertens 2020; 33:860–868. [DOI] [PubMed] [Google Scholar]
- 76. Hoshide S, Yano Y, Mizuno H, Kanegae H, Kario K. Day-by-day variability of home blood pressure and incident cardiovascular disease in clinical practice: the J-HOP Study (Japan Morning Surge-Home Blood Pressure). Hypertension 2018; 71:177–184. [DOI] [PubMed] [Google Scholar]
- 77. Breaux-Shropshire TL, Judd E, Vucovich LA, Shropshire TS, Singh S. Does home blood pressure monitoring improve patient outcomes? A systematic review comparing home and ambulatory blood pressure monitoring on blood pressure control and patient outcomes. Integr Blood Press Control 2015; 8:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Matsui Y, Eguchi K, O’Rourke MF, Ishikawa J, Miyashita H, Shimada K, Kario K. Differential effects between a calcium channel blocker and a diuretic when used in combination with angiotensin II receptor blocker on central aortic pressure in hypertensive patients. Hypertension 2009; 54:716–723. [DOI] [PubMed] [Google Scholar]
- 79. Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ 2004; 329:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010;CD005182. [DOI] [PubMed] [Google Scholar]
- 81. Bray EP, Holder R, Mant J, McManus RJ. Does self-monitoring reduce blood pressure? Meta-analysis with meta-regression of randomized controlled trials. Ann Med 2010; 42:371–386. [DOI] [PubMed] [Google Scholar]
- 82. Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension 2011; 57:29–38. [DOI] [PubMed] [Google Scholar]
- 83. Omboni S, McManus RJ, Bosworth HB, Chappell LC, Green BB, Kario K, Logan AG, Magid DJ, Mckinstry B, Margolis KL, Parati G, Wakefield BJ. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: an International Expert Position Paper. Hypertension 2020; 76:1368–1383. [DOI] [PubMed] [Google Scholar]
- 84. McLean G, Band R, Saunderson K, Hanlon P, Murray E, Little P, McManus RJ, Yardley L, Mair FS; DIPSS Co-Investigators . Digital interventions to promote self-management in adults with hypertension systematic review and meta-analysis. J Hypertens 2016; 34:600–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Milani RV, Lavie CJ, Bober RM, Milani AR, Ventura HO. Improving hypertension control and patient engagement using digital tools. Am J Med 2017; 130:14–20. [DOI] [PubMed] [Google Scholar]
- 86. McManus RJ, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, Kaambwa B, Banting M, Bryan S, Little P, Williams B, Hobbs FD. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet 2010; 376:163–172. [DOI] [PubMed] [Google Scholar]
- 87. Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, O’Connor PJ, Pritchard RA, Sekenski JL, Sperl-Hillen JM, Trower NK. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013; 310:46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Nishizawa M, Hoshide S, Okawara Y, Matsuo T, Kario K. Strict blood pressure control achieved using an ICT-based home blood pressure monitoring system in a catastrophically damaged area after a disaster. J Clin Hypertens (Greenwich) 2017; 19:26–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Kario K, Nomura A, Harada N, Tanigawa T, So R, Nakagawa K, Suzuki S, Okura A, Hida E, Satake K. A multicenter clinical trial to assess the efficacy of the digital therapeutics for essential hypertension: rationale and design of the HERB-DH1 trial. J Clin Hypertens (Greenwich) 2020; 22:1713–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Kario K. Management of hypertension in the digital era: small wearable monitoring devices for remote blood pressure monitoring. Hypertension 2020; 76:640–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of a wrist-type home nocturnal blood pressure monitor in the sitting and supine position according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-9600T. J Clin Hypertens (Greenwich) 2019; 21:463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of two watch-type wearable blood pressure monitors according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J Clin Hypertens (Greenwich) 2019; 21:853–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Kario K, Shimbo D, Tomitani N, Kanegae H, Schwartz JE, Williams B. The first study comparing a wearable watch-type blood pressure monitor with a conventional ambulatory blood pressure monitor on in-office and out-of-office settings. J Clin Hypertens (Greenwich) 2020; 22:135–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Kabutoya T, Takahashi S, Watanabe T, Imai Y, Uemoto K, Yasui N, Kario K. Diagnostic accuracy of an algorithm for detecting atrial fibrillation in a wrist-type pulse wave monitor. J Clin Hypertens (Greenwich) 2019; 21:1393–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Kanegae H, Suzuki K, Fukatani K, Ito T, Harada N, Kario K. Highly precise risk prediction model for new-onset hypertension using artificial intelligence techniques. J Clin Hypertens (Greenwich) 2020; 22:445–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Koshimizu H, Kojima R, Kario K, Okuno Y. Prediction of blood pressure variability using deep neural networks. Int J Med Inform 2020; 136:104067. [DOI] [PubMed] [Google Scholar]
- 97. Wang JG, Bunyi ML, Chia YC, Kario K, Ohkubo T, Park S, Sukonthasarn A, Tay JC, Turana Y, Verma N, Wang TD, Imai Y. Insights on home blood pressure monitoring in Asia: expert perspectives from 10 countries/regions. J Clin Hypertens (Greenwich) 2021; 23: 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]