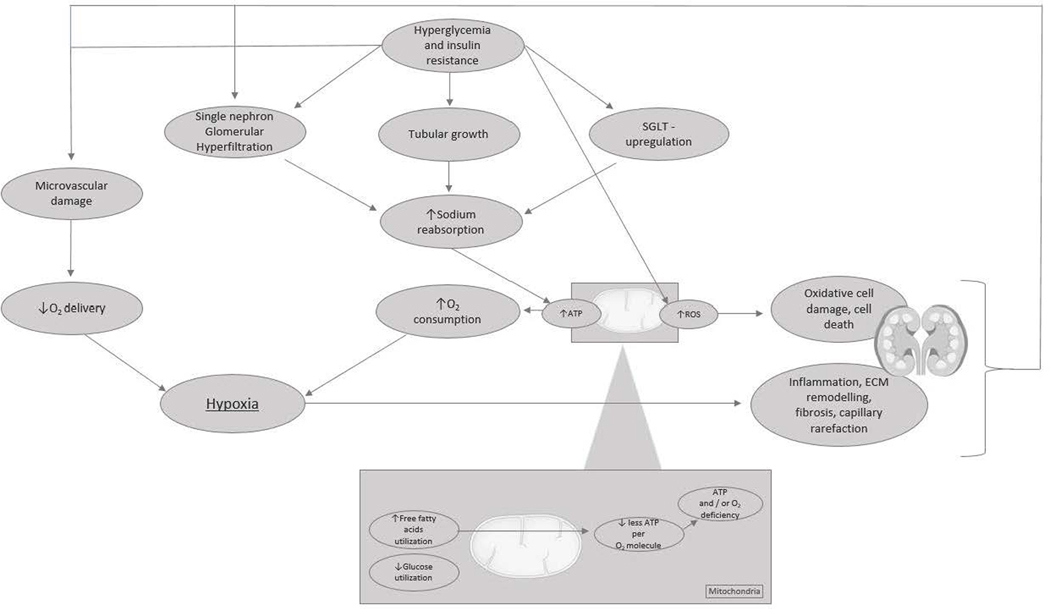
Figure 2. The vicious cycle of renal tissue deterioration after hyperglycemia-induced renal hypoxia.
Chronic hyperglycemia following insulin resistance is perceived to induce (single-nephron) hyperfiltration, tubular growth, and upregulation of sodium–glucose cotransporters. All adaptations lead to an increase in sodium reabsorption, which increases adenosine triphosphate (ATP) demand and oxygen (O2) consumption. Diversely, hyperglycemia causes microvascular damage, resulting in a decrease in renal perfusion and O2 delivery, and a metabolic shift in energy substrate use from glucose oxidation toward the less efficient oxidation of free fatty acids, which results in less generation of ATP per O2 molecule. The net effect of increased ATP demand and decreased ATP generation is an ATP deficit and renal tissue hypoxia. Hypoxia triggers inflammation, extracellular matrix (ECM) remodeling, capillary rarefaction, and fibrosis. In addition, hyperglycemia leads to oxidative cell damage directly because of the increased formation of reactive oxygen species (ROS) as a byproduct of the electron transport chain. The deterioration of renal tissue initiates a vicious cycle of hypoxic injury, glomerular loss, and progressive nephropathy.