Abstract
A viral spread occurrence such as the SARS-CoV-2 pandemic has prompted the evaluation of different disinfectants suitable for a wide range of environmental matrices. Chlorine dioxide (ClO2) represents one of the most-used virucidal agents in different settings effective against both enveloped and nonenveloped viruses. This narrative synthesis is focused on the effectiveness of ClO2 applied in healthcare and community settings in order to eliminate respiratory transmitted, enteric, and bloodborne viruses. Influenza viruses were reduced by 99.9% by 0.5–1.0 mg/L of ClO2 in less than 5 min. Higher concentration (20 mg/L) eliminated SARS-CoV-2 from sewage. ClO2 concentrations from 0.2 to 1.0 mg/L ensured at least a 99% viral reduction of AD40, HAV, Coxsackie B5 virus, and other enteric viruses in less than 30 min. Considering bloodborne viruses, 30 mg/L of ClO2 can eliminate them in 5 min. Bloodborne viruses (HIV-1, HCV, and HBV) may be completely eliminated from medical devices and human fluids after a treatment with 30 mg/L of ClO2 for 30 min. In conclusion, ClO2 is a versatile virucidal agent suitable for different environmental matrices.
Keywords: chlorine dioxide, SARS-CoV-2, enteric viruses, bloodborne viruses
1. Introduction
Disinfection treatments in healthcare and community settings are aimed at achieving microbiological compliance for environmental matrices (drinking water, air, and surfaces). Disinfection is the final treatment after cleaning, which acts on the residual microbiological component, ensuring the absence of pathogens. Among the several chemical biocides, chlorine compounds such as chlorine dioxide, sodium hypochlorite, and chloramines are usually recognized as useful in reducing the infection risk related to environmental matrices in healthcare facilities [1].
The use of gaseous chlorine dioxide as a disinfection agent for drinking water has been increasing in recent years. It is an unstable gas produced on-site by mechanical generators using acid-based or electrolytic methods [1], and it is usually used for water treatment at a concentration between 0.1 and 5.0 mg/L.
It is used as an oxidant agent [2] decomposing the biofilm inside pipes and tanks [3], and it can react only by oxidation with a low trihalomethanes (THM) formation in water. In fact, it has an oxidizing effect on organic components originating from mainly oxidized byproducts and a small amount of chloro-organic compounds, while chlorine reacts with various substances via oxidation and electrophilic substitution [4]. Chlorine dioxide (ClO2) is more biocidal than both chlorine and chloramines, but it generates organoleptic defects in the water after treatment [5]. Actually, in comparison to chlorine, ClO2 reduces the generation of toxic halogenated disinfection byproducts, but ClO2 disadvantages are the formation of the organic halides chlorite/chlorate and the production of tastes and odors at concentrations of 0.5 mg/L [6].
Since 1940, data have been published demonstrating the chlorine dioxide action on bacteria, viruses, biofilms, protozoa, and algae [7]. In case of viruses, the inactivation mechanism differs from that of bacteria or other cells. The inactivation time of a virus is probably much shorter than that of a bacterium under the same conditions. ClO2 gas does not necessarily penetrate viruses to inactivate them. ClO2 reacts with one or more of the cysteine, tyrosine, and tryptophan amino acid residues of the spike proteins located on the enveloped viral surface. In the case of nonenveloped viruses, ClO2 acts on the viral genome [8,9,10].
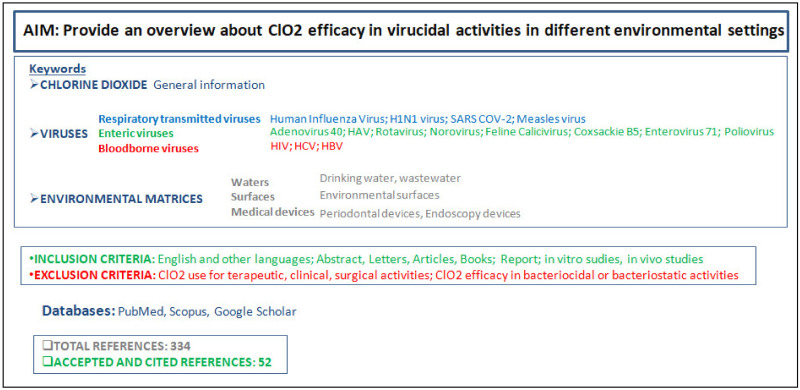
The aim of this narrative review is the evaluation of the main studies performed on ClO2 activity on respiratory transmitted, enteric, and bloodborne viruses.
We provide an overview of the ClO2 features, usage settings, and its virucidal spectrum. The cited viruses were chosen on the basis of the available data and the references provided by some databases (PubMed, Scopus, and Google Scholar).
A scientific study design with the research details is provided in Figure 1.
Figure 1.
Study design representation: aim, keywords, inclusion and exclusion criteria, and references.
1.1. Virucidal Activity of ClO2
There are many studies on the virucidal activity of ClO2, involving both nonenveloped and enveloped viruses. Enveloped viruses are different from nonenveloped ones due to the presence of a lipid bilayer membrane outside the viral protein capsid, which contains proteins or glycoproteins. The presence of different functional groups on the outer surface of enveloped viruses impacts their survival in different environments [11,12]. A lot of factors have also been found to have a great impact on virus inactivation rates, such as the ClO2 dosage, time, pH, and temperature [13].
Sanekata suggested that enveloped viruses are inactivated more easily than nonenveloped viruses when exposed to 1.0 mg/L of ClO2 [14]. The disinfectant action on the enveloped proteins cause a failure of the viral attachment to the host cell, and so, the failure of cell invasion and infection [15]. About that, some authors carried out a study showing that ClO2 inactivates the virus thanks to its reaction with amino acids like cysteine and tryptophan [16]. Noss et Haunchman found that the site of the disinfectant action is a viral protein component; inactivating the coat viral protein inhibits the virus’s ability to attack the host cells [10].
These statements were supported by Olivieri et al., who showed that the viral proteins and lipids were sufficiently altered by ClO2 during a disinfection treatment [17]. Both the human and animal cells are not free from the ClO2 effects, but the damage was not comparable to that on microorganisms for several reasons. Not only are the mammalian cell sizes much larger and a greater disinfectant exposure is needed, but these cells have protection systems such as glutathione and further proteins [1,18].
1.2. ClO2 Activity on Respiratory Transmitted Viruses
Sanekata et al. evaluated the antiviral activity of ClO2 and sodium hypochlorite against human influenza virus (IFV). ClO2 reduced influenza viruses by 99.9% at 1.0 ppm for 15 s, while the same antiviral activity was obtained for sodium hypochlorite at 100 ppm for 15 s [14].
Lenes studied the ClO2 action on the H1N1 virus. Tests were performed with contact times of 5 min and a residual ClO2 value of 0.5 mg/L. After the treatment, the H1N1 virus was not detected in any of the samples. The H1N1 virus is effectively inactivated by chlorine dioxide [19].
Ogata found that ClO2 antimicrobial activity is based on protein denaturation through amino acid residue oxidative modification. In particular, tyrosine and tryptophan residues in the hemagglutinin protein constitute an important active-site pocket for viral infectivity. ClO2 causes a functional modification of these amino acids with a loss of infectivity. Ogata demonstrated that ClO2 reacts with the tryptophan 153 residue, inactivating the hemagglutinin function [20,21,22].
Kalay-Kullay assessed that ClO2 action on amino acid residues could also be the mechanism for the antiviral activity on SARS-CoV. Spike proteins contain tyrosine, tryptophan, and cysteine residues with which the disinfectant can easily react in an aqueous solution with rapid virus inactivation [9]. Carducci et al. reported that SARS-CoV seeds in 100 mL of domestic sewage may be completely inactivated with a disinfection with 20 mg/L of ClO2 for 30 min [23]. Additionally, Wang performed a similar study with comparable results (10 mg/L of ClO2 for 10 min and 40 mg/L of ClO2 for 5 min, with total viral inactivation) [24].
New epidemiological approaches have been investigated in order to define wastewater surveillance, aimed at determining the spread, persistence, and detection of SARS-CoV-2 or other viruses in communities during their most critical epidemiological occurrences.
ClO2 in the most-used and effective method for the abatement of viral loads in these types of waters. It can inactivate SARS-CoVs completely after 30 min of exposure time and at a concentration of 40 mg/L [25].
The same result was not obtained after a sewage treatment with other disinfectants, especially if they were not chlorine-based.
Wastewater-based epidemiology is a new approach for monitoring viral pathogens spreading (SARS-CoV-2) in different contexts and countries. It is a valuable early warning system. It is a helpful alternative surveillance tool to subside the public health response, containing and measuring different infectious risk levels, mostly for poor sanitation settings [26].
Moreover, against the Measles virus, the ClO2 antiviral activity of 99.99% of the viral load was obtained at 10 mg/L for 30 s or at 100 mg/L for 15 s [14,27].
The principal tests performed on the respiratory transmitted viruses are summarized in Table 1.
Table 1.
Literature data on the reduction of respiratory transmitted viruses following chlorine dioxide treatments at different times and concentrations.
| Chlorine Dioxide Concentration |
Exposure Time | Viral Reduction | Author and Year |
|---|---|---|---|
| 1 mg/L | 15 s | Human influenza virus (99.9%) | Sanekata 2010 |
| 0.5 mg/L | 5 min | H1N1 virus (99.9%) | Lénès 2010 |
| 20 mg/L in sewage | 30 min | SARS-CoV-2 (99.99%) | Carducci 2020 |
| 10 mg/L 100 mg/L |
30 s 15 s |
Measles virus (99.99%) | Sanekata 2010 |
1.3. ClO2 Activity on Enteric Viruses
The viral inactivation by ClO2 was studied by Thurston-Enriquez et al. on Adenovirus type 40 (AD40). The tests were performed in various conditions, such as different pH values (8 and 6) and temperatures values (15 °C and 5 °C). The ClO2 doses ranged from 0.67 to 1.28 mg/L.
The rate of AD40 inactivation was higher at pH 8 and/or a temperature of 15 °C than at pH 6 and/or a temperature of 5 °C. The ClO2 efficacy increased at higher experimental temperatures and pH levels.
The concentration of ClO2 multiplied by the contact time with the virus needed for a 4-log inactivation (Ct99.99%) for AD40 at 5 °C was 1.28 and 0.67 mg/L × min at pH 6 and 8, respectively. The Ct99.99% values for AD40 were about two times higher at pH 6 than at pH 8 [6].
A Chinese research group tested the dioxide chlorine action on the Human Hepatitis A Virus (HAV) at a concentration of 5 mg/L. After 60 min, they observed that the infectivity was not completely eliminated yet. Increasing the concentration to 7.5 mg/L, HAV was completely inactivated after 10 min. The action mechanism was found in the viral genome damage and/or viral proteins destruction. Li et al. assessed that the disinfectant damaged the 5′-nontranslated region (5′NTR) of the genome, blocking its replication and reacting with the viral proteins, stopping the interactions with the host cells [15]. The Department of Public Health of Parma reported a faster inactivation of HAV (only 30 s at a 0.8-mg/L concentration and 5 min at 0.4 mg/L) [15,28].
Li et al. revealed that ClO2 reduced the HAV infectivity through 5′-NCR damage [29]. Simonet et al. reported similar findings as that of Li et al. for Poliovirus-1 (PV-1), whereby the 5′-NCR and 3′-NCR of the PV1 genome appeared to be the most sensitive to the ClO2 treatment [30].
Several studies have been performed on the ClO2 actions against enterovirus such as the poliovirus, norovirus, and coxsackievirus. Brigano et al. [31] promoted a theory based on the thermodynamic analysis asserting that ClO2 inactivates viruses through the denaturation of protein coatings. Although ClO2 reacts with coated proteins, changing the pH value (pH 6), the critical target appears to be the viral RNA. Alvarez and O’Brien [32] observed that the poliovirus inactivation at pH 10.0 was faster than at pH 6.0 [33,34].
A possible explication may be related to the alkaline disinfectant dissociation in chlorite (ClO2−) and chlorate (ClO3−). Berman et al. observed the same effect for the Rotavirus. They compared the inactivation obtained by chlorine, ClO2, and monochloramine at 5 °C at pH 6 and 10 on a purified preparation of single virions with 0.5 mg/L of disinfectant. At pH 6, more than 4 log (99.99%) of the single virions were inactivated in less than 15 s with chlorine and monochloramine. With ClO2, this effect was observed at pH 10 [13].
For Poliovirus, Tenno Fujioka and Loh indicated that ClO2 damages the RNA, separating the RNA from the viral capsid at pH 10 but not at pH 6. Virion is converted into an empty capsid, suggesting that the loss of infectivity is due to a slight structural modification of the capsid [35]. The antiviral activity against Norovirus was tested by Sanekata using feline calicivirus (FCV). An initial antiviral effect was obtained with 1 ppm of ClO2 for 180 s, but the antiviral activity against >99.99% of the virus was obtained with 10 ppm of ClO2 for 15 s [14].
In a study conducted by Alvarez, FCV was completely eliminated in 30 min by ClO2 at a concentration of 0.2 mg/L, and Coxsackie B5 showed a similar behavior, being completely inactivated in 4 min with 0.4 mg/L of ClO2 and after 30 min at a 0.2 mg/L concentration [32].
Thurston-Enriquez et al. observed that the total inactivation could be achieved when Enterovirus 71 (EV71) was treated with a concentration of 0.5 mg/L ClO2 for over 30 min, 1.5 mg/L ClO2 for 25 min, or 2.0 mg/L ClO2 for 15 min. The inactivation was more effective at pH 8.2 than at pH 5.6 with 4.92 mg/L of ClO2 for 1 min. Considering the temperature parameter, the inactivation was faster at 36 °C than at 4 °C or 20 °C. The ClO2 efficacy for EV71 was pH and temperature-dependent. Similarly, the inactivation of AD40 and FCV by ClO2 was reported to be higher at 15 °C than at 5 °C [6]. Jin et al. evaluated the ClO2 effect on EV71 infectivity and the genomic integrity. With 13.51 mg/L of ClO2 for 1 min, the 5′-NCR was not amplified by RT-PCR, and the viral infectivity disappeared.
Harakeh tested the ClO2 effect on three viruses: Human rotavirus, Coxsackievirus B5, and Poliovirus 1. The three enteroviruses were tested at pH 7.2 and 15 °C. Coxsackievirus B5 was the most resistant, with 17.25 ppm needed, whereas 15 ppm of free residual ClO2 was required for a complete inactivation (99.99%) in 5 min [36].
The Poliovirus 1 genome was not affected after the treatment with 0.5 mg/L of ClO2 for 120 min. This was confirmed by Tenno et al., who observed that nearly all the Poliovirus 1 genome remained infectious after exposure to 0.2 mg/L of ClO2 for 30 min. The ClO2 dose relationship was clearly demonstrated by exposing the genome to a higher concentration of ClO2 (5 mg/L) for 30 min, which resulted in a significant degradation of the viral RNA.
Tachikawa et al. asserted that ClO2 in drinking water may reduce a 4-log Poliovirus load in 2.5 min at 20 °C and pH 7 [37,38,39].
The significant reduction of enteric virus outbreaks in developed countries is partly due to the ClO2 efficacy in waters and wastewaters; this is also true for the most resistant viruses, such as Poliovirus and other Picornaviridae.
The principal tests performed on the enteric viruses are summarized in Table 2.
Table 2.
Literature data on the reduction of enteric viruses following chlorine dioxide treatments at different times and concentrations.
| Chlorine Dioxide Concentration |
Exposure Time | Viral Reduction | Author and Year |
|---|---|---|---|
| 0.67 mg/L (pH 8) 1.28 mg/L (pH 6) |
1 min | Adenovirus type 40 (4 log) | Thurston-Enriquez 2005 |
| 7.5 mg/L | 10 min | Human Hepatitis A Virus (100%, total genomic damage) | Li 2004 |
| 0.8 mg/L | 0.5 min | Human Hepatitis A Virus (99%) | Zoni 2007 |
| 0.4 mg/L | 5 min | Human Hepatitis A Virus (99%) | Zoni 2007 |
| 0.5 mg/L | 15 s | Rotavirus (4log) | Berman 1984 |
| 1 mg/L 10 mg/L |
3 min 15 s |
Norovirus (99.99%) Norovirus (99.99%) |
Sanekata 2010 |
| 0.2 mg/L | 30 min | Feline Calicivirus (99.99%) | Zoni 2007 |
| 0.4 mg/L | 4 min | Coxsackie B5 virus (99.99%) | Zoni 2007 |
| 0.5 mg/L | 30 min | Enterovirus 71 (99.99%) | Thurston-Enriquez 2005 |
| 0.5 mg/L | 30 min | Poliovirus 1 (RNA damage) | Simonet 2005 |
| 1 mg/L | 2.5 min | Poliovirus (4 log) | Tachikawa 1993 |
1.4. ClO2 Activity on Bloodborne Viruses
Farr et al. tested the ClO2 activity in Human immunodeficiency virus type 1 (HIV-1) inactivation. The virus was treated by adding 100 µL of ClO2 to 0.9 mL of HIV-1 stock for a final concentration of 30 ppm. The preparation was incubated at 25 °C for 5 min. To test the effect in human blood, 100 µL of ClO2 and 250 µL of human whole blood were added to 650 µL of HIV-1 stock in order to achieve viral inactivation. In the presence of medical supplies (plastic and paper materials), the virus was inactivated by adding 100 µL of ClO2 to 0.9 mL of HIV-1 stock. The results showed a viral reduction of 5.25 log. In the presence of blood or medical devices, the HIV-1 reduction was higher than 4 log [40].
A group of Japanese researchers carried out a study on HCV-positive (human hepatitis C) periodontitis patients in order to evaluate the viral elimination on the ultrasonic cleaning device after a treatment with ClO2.
After the periodontal activity, the instrument was disinfected with 0.02% ClO2 for 10 min. The total absence of HCV genomic units was assessed in a RT-PCR test directly performed on the devices [41]. Another study about the surgical instruments was performed by Isomoto et al. on endoscope disinfection after procedures on HCV-positive patients. The devices were reprocessed with 30 mg/L of ClO2 for 5 min. HCV genomic units were not detected in the RT-PCR test after the treatment [42].
Aseptrol®, containing a noncorrosive formula of ClO2, may eliminate the Hepatitis B virus (HBV) genome if it is used at 24 mg/L for 5 min on environmental surfaces [43].
The principal tests performed on the enteric viruses are summarized in Table 3.
Table 3.
Literature data on the reduction of bloodborne viruses following chlorine dioxide treatments at different times and concentrations.
| Chlorine Dioxide Concentration | Exposure Time | Viral Reduction | Author and Year |
|---|---|---|---|
| 30 mg/L (in blood sample) | 5 min | Human Immunodeficiency Virus type 1 (4 log) | Farr 1993 |
| 0.02% 30 mg/L |
10 min 5 min |
Hepatitis C Virus (periodontal device) (99.99%) Hepatitis C Virus (endoscopy device) (99.99%) |
Watamoto 2013 Isomoto 1998 |
| 24 mg/L (Aseptrol®) | 5 min | Hepatitis B Virus (99.99%) | Ebonwu 2010 |
2. Conclusions
Chlorine dioxide has been widely applied in environmental matrix disinfections, mostly for waters and wastewaters. In healthcare settings, disinfection procedures have to ensure viral inactivation in order to prevent outbreaks and epidemic occurrences. The use of ClO2 is the final step in a virucidal agent [44]. In 2018, the United Stated Environmental Protection Agency (USEPA) [45] cited adenoviruses, caliciviruses, enteroviruses, and hepatitis A virus as microbiological drinking water contaminants that may be disseminated through aquatic environments. The evaluation of the efficacy of alternative disinfectants such as ClO2 is important to perform in order to eliminate these virus species from drinking water. There have been many studies reporting virucidal activity against waterborne and nonwaterborne viruses, including nonenveloped viruses (e.g., adenoviruses and enteroviruses) and enveloped viruses (e.g., influenza viruses).
Considering enteric viruses, ClO2 concentrations ranging from 0.2 to 1.0 mg/L ensure at least a 99% viral reduction of AD40, HAV, Coxsackie B5 virus, Norovirus, Rotavirus, Feline Calicivirus, and EV71 in less than 30 min. Moreover, ClO2 is the most-used disinfectant for drinking water treatment, and its efficacy may be achieved by the routine of continuous water chlorination, as described elsewhere (0.2 mg/L of chlorine dioxide) [46,47].
Similar results have been obtained for respiratory transmitted virus elimination. In particular, 0.5–1.0 mg/L of ClO2 for less than 5 min can reduce influenza viruses by 99.9% (the H1N1 virus included). Sewage and wastewaters may be treated with 20 mg/L of ClO2 in order to obtain a total SARS-CoV-2 elimination. At last, considering bloodborne viruses, 30 mg/L of ClO2 eliminates, in 5 min, HIV-1 in human organic fluids (blood) or medical supplies. HCV may be eliminated from medical devices after an application of 30 mg/L of ClO2 for 10 min. This narrative synthesis highlights the need for disinfection procedures with ClO2 applied to different matrices. The versatility of ClO2 is widely known for disinfection procedures in large and populated indoor environments, such as hospitals and generic healthcare facilities. Moreover, considering the high vulnerability of infected patients hosted in infectious disease wards and intensive care units, the application of ClO2 may be the solution for routine disinfection protocols in order to minimize the risk of viral agent transmissions (respiratory transmitted, enteric, or bloodborne viruses) and nosocomial and community infections [48,49]. The international recommendations published for SARS-CoV-2 prevention in hospital settings described the importance of environmental sanitization using only biocides tested for virucidal activity, as required by UNI EN 14476:2019 [50]. The Italian Institute of Health included ClO2 as a possible disinfectant for hospital sanitization in rooms having a high infectious risk [51].
This narrative synthesis aimed to highlight the versatility and suitability of ClO2 in different settings (mostly for waters) and against different viral agents.
It may be clear that ClO2 is not a therapeutic product. It cannot be used for healing human or animal tissues, with the exception of skin and mucosa antisepsis.
In conclusion, ClO2 is one of the most-used biocides for different environmental settings. It is a recognized versatile virucidal agent, and its efficacy is dose-dependent. It may be used as a high-, intermediate-, or low-level agent [48,52], in accordance with the suitable disinfection grade needed in different situations.
Author Contributions
A.B., G.P. and G.B.M.F. conceptualized the narrative synthesis. M.T., F.B. and B.T. wrote the original draft. A.L.C. and B.C. revised the draft. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are openly available.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ma J.-W., Huang B.-S., Hsu C.-W., Peng C.-W., Cheng M.-L., Kao J.-Y., Way T.-D., Yin H.-C., Wang S.-S. Efficacy and Safety Evaluation of a Chlorine Dioxide Solution. Int. J. Environ. Res. Public Heal. 2017;14:329. doi: 10.3390/ijerph14030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Symons J.M., Stevens A., Clark R.M., Geldreich E.E., Love O.T., Jr., DeMarco J. Treatment tecniques for controlling trihalomethanes in drinking water. Cincinnati EPA. 1981;1:10–22. [Google Scholar]
- 3.Michael G.E., Miday R.K., Bercz J.P., Miller R.G., Greathouse D.G., Kraemer D.F., Lucas J.B. Chlorine Dioxide Water Disinfection: A Prospective Epidemiology Study. Arch. Environ. Health Int. J. 1981;36:20–27. doi: 10.1080/00039896.1981.10667601. [DOI] [PubMed] [Google Scholar]
- 4.WHO . The World Health Report 2002. World Health Organization; Geneva, Switzerland: 2002. Quantifying selected major risks to health. [Google Scholar]
- 5.Ngwenya N., Ncube E.J., Parsons J. Recent Advances in Drinking Water Disinfection: Successes and Challenges No Title. Rev. Environ. Contam. Toxicol. 2013;22:111–170. doi: 10.1007/978-1-4614-4717-7_4. [DOI] [PubMed] [Google Scholar]
- 6.Thurston-Enriquez J.A., Haas C.N., Jacangelo J., Gerba C.P. Inactivation of enteric adenovirus and feline calicivirus by ozone. Water Res. 2005;39:3650–3656. doi: 10.1016/j.watres.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Aieta E.M., Berg J.D. A review of chlorine dioxide in drinking water treatment. J. Am. Water Work. Assoc. 1986;78:62–72. doi: 10.1002/j.1551-8833.1986.tb05766.x. [DOI] [Google Scholar]
- 8.Noszticzius Z., Wittmann M., Kály-Kullai K., Beregvári Z., Kiss I., Rosivall L., Szegedi J. Chlorine Dioxide Is a Size-Selective Antimicrobial Agent. PLoS ONE. 2013;8:e79157. doi: 10.1371/journal.pone.0079157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kály-Kullai K., Wittmann M., Noszticzius Z., Rosivall L. Can chlorine dioxide prevent the spreading of coronavirus or other viral infections? Medical hypotheses. Physiol. Int. 2020;107:1–11. doi: 10.1556/2060.2020.00015. [DOI] [PubMed] [Google Scholar]
- 10.Noss C.I., Hauchman F.S., Olivieri V.P. Chlorine dioxide reactivity with proteins. Water Res. 1986;20:351–356. doi: 10.1016/0043-1354(86)90083-7. [DOI] [Google Scholar]
- 11.Arbely E., Granot Z., Kass I., Orly A.J., Arkin I. A Trimerizing GxxxG Motif Is Uniquely Inserted in the Severe Acute Respiratory Syndrome (SARS) Coronavirus Spike Protein Transmembrane Domain†. Biochemistry. 2006;45:11349–11356. doi: 10.1021/bi060953v. [DOI] [PubMed] [Google Scholar]
- 12.Shigematsu S., Dublineau A., Sawoo O., Batéjat C., Matsuyama T., Leclercq I., Manuguerra J.-C. Influenza A virus survival in water is influenced by the origin species of the host cell. Influenza Respir. Viruses. 2013;8:123–130. doi: 10.1111/irv.12179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berman D., Hoff J.C. Inactivation of simian rotavirus SA11 by chlorine, chlorine dioxide, and monochloramine. Appl. Environ. Microbiol. 1984;48:317–323. doi: 10.1128/aem.48.2.317-323.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanekata T., Fukuda T., Miura T., Morino H., Lee C., Maeda K., Araki K., Otake T., Kawahata T., Shibata T. Evaluation of the antiviral activity of chlorine dioxide and sodium hypochlorite against feline calicivirus, human influenza virus, measles virus, canine distemper virus, human herpesvirus, human adenovirus, canine adenovirus and canine parvovirus. Biocontrol Sci. 2010;15:45–49. doi: 10.4265/bio.15.45. [DOI] [PubMed] [Google Scholar]
- 15.Li J.W., Xin Z.T., Wang X.W., Zheng J.L., Chao F.H. Mechanisms of inactivation of hepatitis A virus in water by chlorine dioxide. Water Res. 2004;38:1514–1519. doi: 10.1016/j.watres.2003.12.021. [DOI] [PubMed] [Google Scholar]
- 16.Jolley R.L., Brungs W.A., Cotruvo J.A., Cumming R.B., Mattice J.S., Jacobs V.A. Proceedings of the Water Chlorination: Environmental Impact and Health Effects. Chemistry and Water Treatment; Pacific Grove, CA, USA: 1983. Nucleic Acids and Proteins. [Google Scholar]
- 17.Jolley R.L., Davis W.P., Katz S., Roberts M.H., Bull R.J. Water chlorination: Chemistry, environmental impact and health effects; Proceedings of the Fifth Conference on Water Chlorination: Environmental Impact and Health Effects; Williamsburg, VA, USA. 3–8 June 1984. [Google Scholar]
- 18.Palcsó B., Moldován Z., Süvegh K., Herczegh A., Zelkó R. Chlorine dioxide-loaded poly (acrylic acid) gels for prolonged antimicrobial effect. Mater. Sci. Eng. C. 2019;98:782–788. doi: 10.1016/j.msec.2019.01.043. [DOI] [PubMed] [Google Scholar]
- 19.Lénès D., Deboosere N., Ménard-Szczebara F., Jossent J., Alexandre V., Machinal C., Vialette M. Assessment of the removal and inactivation of influenza viruses H5N1 and H1N1 by drinking water treatment. Water Res. 2010;44:2473–2486. doi: 10.1016/j.watres.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 20.Ogata N., Shibata T. Protective effect of low-concentration chlorine dioxide gas against influenza A virus infection. J. Gen. Virol. 2008;89:60–67. doi: 10.1099/vir.0.83393-0. [DOI] [PubMed] [Google Scholar]
- 21.Lentz M.R., Webster R.G., Air G. Site-directed mutation of the active site of influenza neuraminidase and implications for the catalytic mechanism. Biochemistry. 1987;26:5351–5358. doi: 10.1021/bi00391a020. [DOI] [PubMed] [Google Scholar]
- 22.Ogata N. Inactivation of influenza virus haemagglutinin by chlorine dioxide: Oxidation of the conserved tryptophan 153 residue in the receptor-binding site. J. Gen. Virol. 2012;93:2558–2563. doi: 10.1099/vir.0.044263-0. [DOI] [PubMed] [Google Scholar]
- 23.Carducci A., Federigi I., Liu D., Thompson J.R., Verani M. Making Waves: Coronavirus detection, presence and persistence in the water environment: State of the art and knowledge needs for public health. Water Res. 2020;179:115907. doi: 10.1016/j.watres.2020.115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang X.-W., Li J.-S., Jin M., Zhen B., Kong Q.-X., Song N., Xiao W.-J., Yin J., Wei W., Wang G.-J., et al. Study on the resistance of severe acute respiratory syndrome-associated coronavirus. J. Virol. Methods. 2005;126:171–177. doi: 10.1016/j.jviromet.2005.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh S., Kumar V., Kapoor D., Dhanjal D.S., Bhatia D., Jan S., Singh N., Romero R., Ramamurthy P.C., Singh J. Detection and disinfection of COVID-19 virus in wastewater. Environ. Chem. Lett. 2021;19:1917–1933. doi: 10.1007/s10311-021-01202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aguiar-Oliveira M.d.L., Campos A., Matos A.R., Rigotto C., Sotero-Martins A., Teixeira P.F.P., Siqueira M.M. Wastewater-Based Epidemiology (WBE) and Viral Detection in Polluted Surface Water: A Valuable Tool for COVID-19 Surveillance—A Brief Review. Int. J. Environ. Res. Public Health. 2020;17:9251. doi: 10.3390/ijerph17249251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deborde M., von Gunten U. Reactions of chlorine with inorganic and organic compounds during water treatment-Kinetics and mechanisms: A critical review. Water Res. 2008;42:13–51. doi: 10.1016/j.watres.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 28.Zoni R., Zanelli R., Riboldi E., Bigliardi L., Sansebastiano G. Investigation on virucidal activity of chlorine dioxide. experimental data on feline calicivirus, HAV and Coxsackie B5. J. Prev. Med. Hyg. 2007;48:91–95. [PubMed] [Google Scholar]
- 29.Xin Z.T., Liu C., Dong B., Gao Y.P., Shao N.S., Liu W., Zhang J., Dong J., Ling S.G., Xue Y.N. A subtractive fluorescence-activated cellsorting strategy to identify mimotopes of HBV-preS protein from bacterially displayed peptide library. J. Immunol. Methods. 2004;293:13–21. doi: 10.1016/j.jim.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Simonet J., Gantzer C. Degradation of the Poliovirus 1 genome by chlorine dioxide. J. Appl. Microbiol. 2006;100:862–870. doi: 10.1111/j.1365-2672.2005.02850.x. [DOI] [PubMed] [Google Scholar]
- 31.Brigano F.A., Scarpino P.V., Cronier S., Zink M.L. Effects of particulates on inactivation of enteroviruses in water by chlorine dioxide. In: Venosa A.D., editor. Progress in Wastewater Disinfection Technology. Environmental Protection Agency; Cincinnati, OH, USA: 1979. pp. 86–92. Publication no. EPA-600/9-79-018. [Google Scholar]
- 32.Alvarez M.E., O’Brien R.T. Mechanisms of inactivation of poliovirus by chlorine dioxide and iodine. Appl. Environ. Microbiol. 1982;44:1064–1071. doi: 10.1128/aem.44.5.1064-1071.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zierler S. Drinking Water and Reproductive Health. Epidemiology. 1992;3:77–78. doi: 10.1097/00001648-199203000-00001. [DOI] [PubMed] [Google Scholar]
- 34.Granstrom M.L. Efficiency of Chlorine Dioxide. Microbiology. 1965;13:5. doi: 10.1128/am.13.5.776-780.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tenno K.M., Fujioka R.S., Loh P.C. The mechanism of poliovirus inactivation by hypochlorous acid. In: Jolley R., Brungs W.A., Cumming R.B., editors. Proceedings of the 3rd Conference on Water Chlorination: Environmental Impact and Health Effects; Colorado Springs, CO, USA. 28 October–2 November 1979; Lansing, MI, USA: Ann Arbor Science Publishers; 1980. pp. 665–675. [Google Scholar]
- 36.Harakeh S. The behavior of viruses on disinfection by chlorine dioxide and other disinfectants in effluent. FEMS Microbiol. Lett. 1987;44:335–341. doi: 10.1111/j.1574-6968.1987.tb02311.x. [DOI] [Google Scholar]
- 37.Jolley R.L. Water Chlorination: Environmental Impact and Health Effects; Proceedings of the 3rd Conference on Water Chlorination: Environmental Impact and Health Effects; Colorado Springs, CO, USA. 28 October–2 November 1979; Lansing, MI, USA: Ann Arbor Science Publishers; 1980. [Google Scholar]
- 38.Simonet J., Gantzer C. Inactivation of Poliovirus 1 and F-Specific RNA Phages and Degradation of Their Genomes by UV Irradiation at 254 Nanometers. Appl. Environ. Microbiol. 2006;72:7671–7677. doi: 10.1128/AEM.01106-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tachikawa M., Saita K., Tezuka M., Sawamura R. Inactivation of poliovirus with chlorine dioxide. Eisei Kagaku. 1993;39:572–576. doi: 10.1248/jhs1956.39.6_572. [DOI] [Google Scholar]
- 40.Farr R.W., Walton C. Inactivation of Human Immunodeficiency Virus by a Medical Waste Disposal Process Using Chlorine Dioxide. Infect. Control. Hosp. Epidemiol. 1993;14:527–529. doi: 10.2307/30166592. [DOI] [PubMed] [Google Scholar]
- 41.Watamoto T., Egusa H., Sawase T., Yatani H. Clinical evaluation of chlorine dioxide for disinfection of dental instruments. Int. J. Prosthodont. 2013;26:541–544. doi: 10.11607/ijp.3465. [DOI] [PubMed] [Google Scholar]
- 42.Isomoto H., Urata M., Kawazoe K., Matsuda J., Nishi Y., Wada A., Ohnita K., Hirakata Y., Matsuo N., Inoue K., et al. Endoscope disinfection using chlorine dioxide in an automated washer-disinfector. J. Hosp. Infect. 2006;63:298–305. doi: 10.1016/j.jhin.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 43.Ebonwu J.I. Master’s Thesis. Faculty of Health Sciences; University of the Witwatersrand, Johannesburg, South Africa: 2010. Antimicrobial Effect of Slow Release Chlorine Dioxide Disinfectant, in Comparison with Sodium Dichloroisocyanurate. [Google Scholar]
- 44.Ge Y., Zhang X., Shu L., Yang X. Kinetics and Mechanisms of Virus Inactivation by Chlorine Dioxide in Water Treatment: A Review. Bull. Environ. Contam. Toxicol. 2021;106:560–567. doi: 10.1007/s00128-021-03137-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.US EPA Contaminant Candidate List (CCL) and Regulatory Determination. [(accessed on 30 March 2018)];2018 Available online: https//www.epa.gov/ccl/microbialcontaminantsccl-4.
- 46.Totaro M., De Vita E., Giorgi S., Profeti S., Porretta A., Gallo A., Frendo L., Casini B., Valentini P., Privitera G., et al. Comparison of Anolyte and Chlorine Dioxide for a Continuous Hot Water Disinfection in Nursing Home: A Two Years Legionnaires’ Disease Prevention. J. Water Resour. Prot. 2019;11:233–243. doi: 10.4236/jwarp.2019.113014. [DOI] [Google Scholar]
- 47.Ljujic B., Sundac L. Council Directive 98/83/EC of 3 November 1998 on the quality of water intended for human consumption. Voda Sanitarna Tehnika. 1998;41:32–54. doi: 10.1017/cbo9780511610851.055. [DOI] [Google Scholar]
- 48.Lu M.-C., Chen P.-L., Huang D.-J., Liang C.-K., Hsu C.-S., Liu W.-T. Disinfection efficiency of hospital infectious disease wards with chlorine dioxide and hypochlorous acid. Aerobiologia. 2020;37:29–38. doi: 10.1007/s10453-020-09670-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abreu A.C., Tavares R.R., Borges A., Mergulhão F., Simões M. Current and emergent strategies for disinfection of hospital environments. J. Antimicrob. Chemother. 2013;68:2718–2732. doi: 10.1093/jac/dkt281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.British Standards Institution Chemical disinfectants and antiseptics—Quantitative suspension test for the evaluation of bactericidal activity in the medical area—Test method and requirements (phase 2, step 1) [(accessed on 1 October 2012)];Eur. Comm. Stand. 2012 3 Available online: https://shop.bsigroup.com/ProductDetail/?pid=000000000030318657. [Google Scholar]
- 51.Gruppo di lavoro ISS Biocidi COVID-19 . Raccomandazioni ad Interim sui Disinfettanti Nell’Attuale Emergenza COVID-19: Presidi Medico Chirurgici e Biocidi. Superior Institute of Health; Rome, Italy: 2020. Rapporto ISS COVID-19 n. 19/2020 Rev. [Google Scholar]
- 52.Block S.S. Disinfection, Sterilization, and Preservation. 5th ed. Limpicott Williams & Wilkins; Gainesville, FL, USA: 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are openly available.