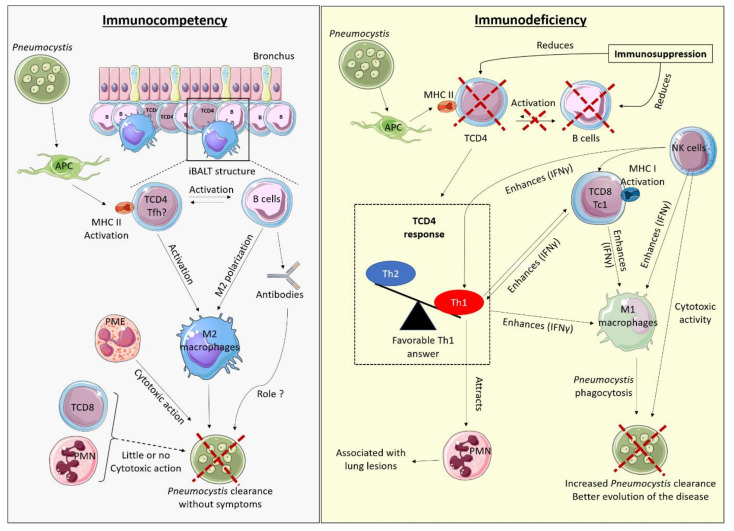
Figure 1.
Hypothetical model of the host immune responses during Pneumocystis infection in the immunocompetent and immunosuppressed host. APC: Antigen Presenting Cells, iBALT: induced-Bronchus Associated Lymphoid Tissue, Tfh: T follicular helper, PMN: Polymorphonuclear neutrophils, PME: Polymorphonuclear eosinophils, MHC: Major Histocompatibility Complex. The red cross represents a reduction of the covered element. In an immunocompetent host (left), Pneumocystis is recognised by APC which activate the TCD4 response, in turn activating B cells (BL), all gathered within structures of germinal centres around the bronchus: induced Bronchus Associated Lymphoid Tissue (iBALT). TCD4 inside those iBALT structures could be T follicular helper cells (Tfh). The joint action of LBs and TCD4 activates macrophages with a preferential M2 polarisation that can then phagocytose Pneumocystis, with or without opsonisation (via antibodies). TCD8 and PMN have little or no action in this context, while eosinophils could intervene through their cytotoxic action on Pneumocystis. This immune response allows clearance of the fungus without respiratory symptoms. In an immunocompromised host (right), in the absence of TCD4 and/or BL populations, the immune response is not properly activated. When TCD4 response is oriented toward a predominant Th1 response, PCP outcome is favourable, with enhanced clearance of the fungus by stimulation of M1 macrophages, through cytokines production, mostly IFNγ. Similarly, TCD8 differentiated into cytotoxic Tc1 and NK cells may participate in the stimulation of macrophages towards M1 polarisation, through their IFNγ secretion. NK cells could also directly eliminate Pneumocystis by their cytotoxic activity on the fungus. M1 activated macrophages can in turn phagocyte Pneumocystis. The pro-inflammatory profile would allow better elimination of the fungus but can induce potential lesions of the lung tissue, associated with significant PMN influx.