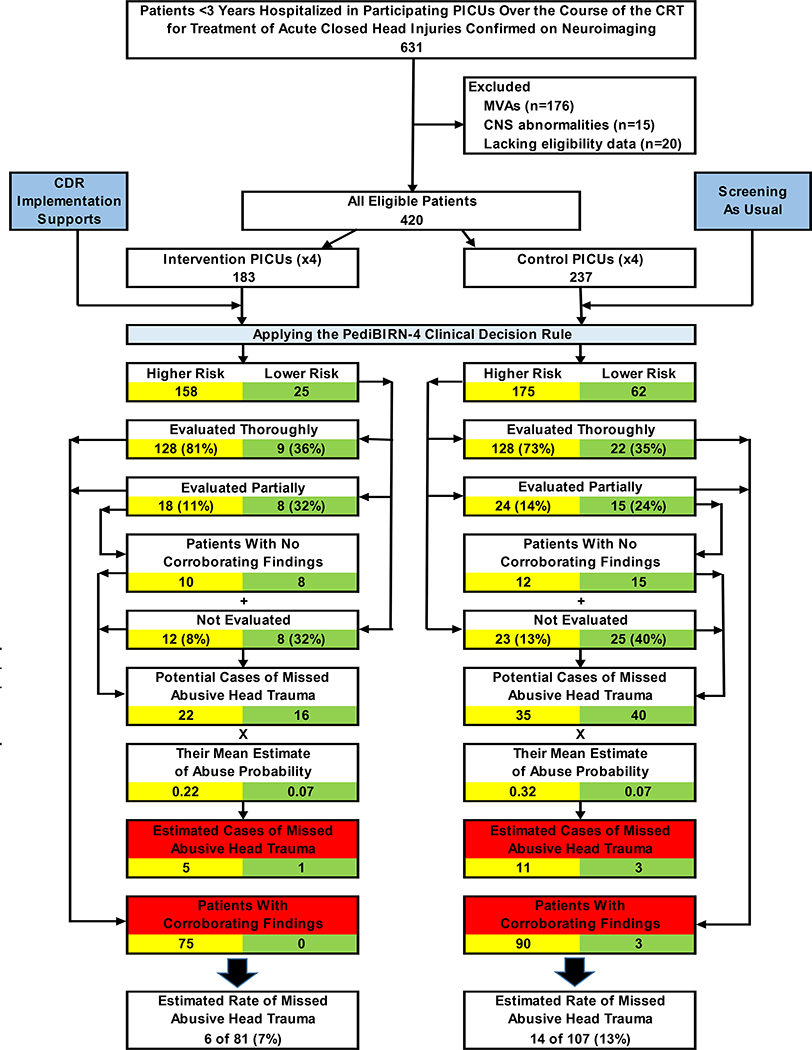
Figure 1. Patient attrition and the impacts of abusive head trauma screening and evaluation practices at intervention vs. control sites over the course of the CRT.
Of the 631 acutely head-injured patients under 3 years of age hospitalized in a participating PICU over the course of the 32-month CRT, 211 (33%) were excluded from study participation. 183 (44%) of the remaining 420 eligible patients were admitted to an intervention PICU, where clinicians were encouraged to apply the PediBIRN-4 CDR as an abusive head trauma screening tool. The remaining 237 patients (56%) were hospitalized in a control PICU, where providers practiced abusive head trauma screening as usual. The yellow boxes track abusive head trauma screening and evaluation practices—and relevant clinical impacts of those practices—in patients the CDR categorized as higher risk. Green boxes track the equivalent practices and outcomes in the remaining lower risk patients. Red boxes highlight corroborated cases of abusive head trauma and estimates of missed abusive head trauma in higher vs. lower risk patients in each arm of the CRT.
Abbreviations: CDR=clinical decision rule, CNS=central nervous system, CRT=cluster randomized trial, PediBIRN=pediatric brain injury research network, PICU=pediatric intensive care unit, MVA=motor vehicle accident