Abstract
Background
The LABBPS (Los Angeles Barbershop Blood Pressure Study) developed a new model of hypertension care for non‐Hispanic Black men that links health promotion by barbers to medication management by pharmacists. Barriers to scaling the model include inefficiencies that contribute to the cost of the intervention, most notably, pharmacist travel time. To address this, we tested whether virtual visits could be substituted for in‐person visits after blood pressure (BP) control was achieved.
Methods and Results
We enrolled 10 Black male patrons with systolic BP ≥140 mm Hg into a proof‐of‐concept study in which barbers promoted follow‐up with pharmacists who initially met each patron in the barbershop, where they prescribed BP medication under a collaborative practice agreement with the patrons' physician. Medications were titrated during bimonthly in‐person visits to achieve a BP goal of ≤130/80 mm Hg. Once BP goal was reached, visits were done by videoconference. Final BP and safety outcomes were assessed at 12 months. Nine patients completed the intervention. Baseline BP of 155±14/83.9±11 mm Hg decreased by −28.7±13/−8.9±15 mm Hg (P<0.0001). These data are statistically indistinguishable from prior LABBPS data (P=0.8 for change in systolic BP and diastolic BP). Hypertension control (≤130/80 mm Hg) was 67% (6 of 9), numerically greater than the 63% observed in LABBPS (P=not significant). As intended, the mean number of in‐person visits decreased from 11 in LABBPS to 6.6 visits over 12 months. No treatment‐related serious adverse events occurred.
Conclusions
Virtual visits represent a viable substitute for in‐person visits, both improving pharmacist efficiency and reducing cost while preserving intervention potency.
Registration
URL: https://www.clinicaltrials.gov; Unique identifier: NCT 03726710.
Keywords: ethnic groups, hypertension, telemedicine
Subject Categories: Hypertension, Race and Ethnicity, Health Services
The LABBPS (Los Angeles Barbershop Blood Pressure Study) demonstrated both efficacy and sustainability1 of a new model of hypertension care for non‐Hispanic Black men that links health promotion by barbers to medication management by specialty‐trained pharmacists. Although cost‐effective, inefficiencies, such as the significant time spent by pharmacists commuting between barbershops, are barriers to scaling the model for broad implementation. To address this, we tested whether virtual visits (ie, patient‐provider interaction using remote video/audio technology) could successfully replace in‐person visits after blood pressure (BP) control was achieved.
We enrolled self‐identified non‐Hispanic Black men, aged 35 to 79 years (n=10), into a single‐arm, proof‐of‐concept pilot study. All men were regular patrons of participating barbershops (≥1 haircut every 6 weeks for ≥6 months) and had systolic BP ≥140 mm Hg on 2 screening days at baseline. Men who planned to relocate or were on dialysis or chemotherapy were excluded. The study was approved by the institutional review board at Cedars‐Sinai, and all participants provided informed written consent. The data, analytical methods, and study materials will not be made available to other researchers for the purposes of reproducing the results or replicating the procedure.
Participants' barbers promoted follow‐up with a specialty‐trained pharmacist who initially met each patron in the barbershop for bimonthly in‐person visits, where they measured BP, encouraged lifestyle modifications, and prescribed BP medication under a collaborative practice agreement with the patrons' primary care provider. BP was measured using a validated oscillometric monitor, and the same automated protocol from LABBPS, which required 5 sequential readings; the average of the last 3 of 5 sequential readings was used for analyses.1 Plasma electrolytes and creatinine were monitored with a point‐of‐care device. Medications were titrated (according to the same algorithm used in LABBPS)1 to achieve a BP goal of ≤130/80 mm Hg. Once achieved, participants were transitioned to monthly virtual visits, connecting with the pharmacist via WebEx‐enabled computers linked to BP monitors, or through commercially available video‐phone platforms (ie, FaceTime) and stand‐alone BP monitors housed in the barbershops. Because the pharmacist was not present, barbers were trained in BP measurement technique and performed BP checks for virtual visits. During remote visits, pharmacists continued to promote lifestyle modifications and titrate medications, as necessary. Participants unable to reach goal BP within 6 months were transitioned back to usual care. The primary end point was the change in systolic BP from baseline to 12 months. Secondary end points included change in diastolic BP, BP control rate (at <140/90 and <130/80 mm Hg), and adverse events.
As shown in the Table, baseline characteristics of study participants and those in the original LABBPS were similar. After exclusion of one participant who declined to adhere to the study protocol, 9 participants completed the intervention. At 12 months, systolic BP decreased from 155±14 to 126±4 mm Hg (mean change, −28.7±13 mm Hg; P<0.0001), and diastolic BP decreased from 83.9±11 to 75±7.2 mm Hg (mean change, −8.9±15 mm Hg; P<0.0001). These new data are statistically indistinguishable from our previous LABBPS data for both the change in systolic BP and BP control rates. The change in diastolic BP at 12 months was less pronounced in our current study and may be attributable to a lower baseline diastolic BP. All participants achieved BP control at <140/90 and <135/85 mm Hg. Six participants (67%) achieved the guideline‐recommended BP goal of <130/80 mm Hg (see the Figure for individual patient data). The number of in‐person pharmacist visits per patron decreased from 11 in LABBPS to just 6.6 in the current study. No treatment‐related serious adverse events occurred. Cohort retention was 90%, which mirrors LABBPS' impressive retention rate.
Table 1.
Baseline Characteristics of Study Participants
| Characteristics | Virtual Visit‐Assisted Program (n=10) | LABBPS, Intervention Arm (n=139) |
|---|---|---|
| Age, mean±SD, y | 57.3±5.9 | 54.4±10.2 |
| Body mass index, mean±SD, kg/m2 * | 29.4±5.1 | 30.7±5.5 |
| Married or living with a partner, n (%) | 4 (40) | 64 (46.4) |
| Highest education, n (%) | ||
| Less than high school | 1 (10) | 6 (4.5) |
| High school graduate (includes equivalency) | 2 (20) | 30 (22.6) |
| Some college, or associate's degree | 5 (50) | 68 (51.1) |
| Bachelor's degree | 2 (20) | 22 (16.5) |
| Graduate or professional degree | 0 (0) | 7 (5.3) |
| Household income, % of the federal poverty level, n (%)† | ||
| <100% of federal poverty limit | 2 (20) | 41 (31.8) |
| 100%–300% of federal poverty limit | 4 (40) | 36 (27.9) |
| 301%–500% of federal poverty limit | 1 (10) | 26 (20.2) |
| >500% of federal poverty limit | 2 (20) | 26 (20.2) |
| Regular medical care provider, n (%) | 10 (100) | 106 (76.8) |
| Any health insurance, n (%) | 10 (100) | 118 (84.9) |
| Barbershop patronage | ||
| Duration of patronage, mean±SD, y | 13.4±9.6 | 10.4±9.9 |
| Time between visits, mean±SD, wk | 2.4±1.8 | 2.0±0.9 |
| Cardiac risk factors, n (%) | ||
| Current smoker | 2 (20) | 43 (31.4) |
| Diabetes mellitus | 5 (50) | 31 (22.3) |
| High cholesterol | 7 (70) | 49 (35.3) |
| Blood Pressure Data‡ |
Virtual Visit‐Assisted Program (n=9)§ |
LABBPS, Intervention Arm (n=139) |
|---|---|---|
| Systolic blood pressure, mean±SD, mm Hg | ||
| Baseline | 157.4±15 | 152.4±10.1 |
| 12 mo | 126.4±5.2 | 123.8±8.8 |
| Change | −28.7±13.4 | −28.6±12.7 |
| Diastolic blood pressure, mean±SD, mm Hg | ||
| Baseline | 85.2±11 | 91.9±11.3 |
| 12 mo | 75.0±7.2 | 74.1±8.2 |
| Change | −8.9±14.7 | −17.8±11.9* |
| Hypertension control rate after 12 mo, n (%) | ||
| Blood pressure <140/90 mm Hg | 9 (100) | 118 (94) |
| Blood pressure <135/85 mm Hg | 9 (100) | 110 (88) |
| Blood pressure <130/80 mm Hg | 6 (67) | 85 (68) |
LABBPS indicates Los Angeles Barbershop Blood Pressure Study.
The body mass index components (height and weight) were self‐reported.
One participant declined to answer. The 2015 US federal poverty guidelines are based on the total household income and family size; in 2015, the federal poverty threshold was $11 770 for a single person and $4160 for each additional person.
P values for all comparisons between telemedicine and LABBPS were >0.05, except where indicated *.
One participant was excluded from analysis because of noncompliance to the protocol.
Figure 1. Individual patient systolic blood pressure data from enrollment to study conclusion.
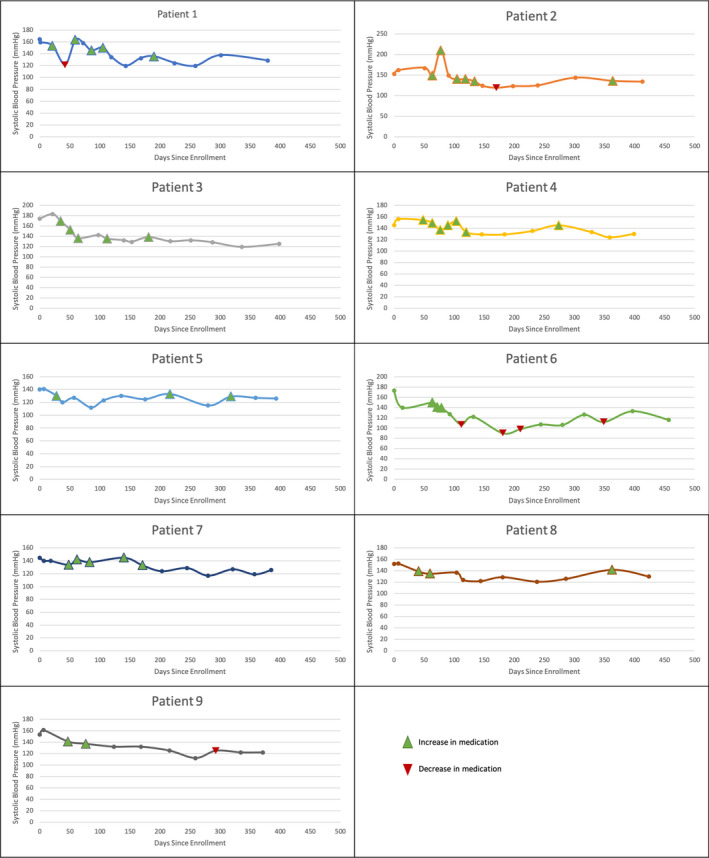
Green triangles indicate medication intensification, red triangles indicate medication de‐escalation, and absence of both indicates no medication change was made during the visit.
Despite steady gains in hypertension awareness and treatment, traditional clinic‐based models of hypertension management continue to deliver unsatisfactory overall BP control rates,2 particularly among Black individuals, who are disproportionally burdened by hypertension‐related morbidity and mortality.3 The community‐based model of hypertension care for Black men developed in LABBPS represents a novel approach to address this disparity, but widespread adoption of such a program is limited by intervention cost and logistical inefficiencies. Telemedicine has proven successful in pharmacist‐led trials involving both Black and non‐Black individuals with hypertension4 and has been widely adopted in the COVID‐19 era to protect both patients and providers.5 The rapidly evolving technology also helps address barriers to care that have traditionally contributed to healthcare disparities (ie, access to care attributable to distance, cost of travel, lost wages, and childcare). Herein, we demonstrate that virtual visits represent a viable substitute for in‐person visits, improving pharmacists' efficiency and reducing costs, while preserving intervention efficacy. These findings provide promising feasibility data for future broad‐scale implementation efforts and the development of cost‐effective barbershop and other community‐based hypertension management programs. Ongoing research is required to determine which aspects of the LABBPS were considered most essential by both participants and providers to further tailor the model into the most cost‐effective and scalable version for broad implementation. Future research directed at the development and implementation of community‐based programs is needed to address persistent health disparities among medically underserved populations.
Sources of Funding
This work was supported by the Medtronic Foundation.
Disclosures
None.
Acknowledgments
The authors thank the barbers for their participation and barbershop owners for allowing us to conduct the study in their shops. Finally, we wish to dedicate this article to Ronald G. Victor, MD, the study's architect and our beloved colleague, mentor, and friend.
(J Am Heart Assoc. 2021;10:e020796. DOI: 10.1161/JAHA.120.020796.)
For Sources of Funding and Disclosures, see page 4.
REFERENCES
- 1.Victor RG, Blyler CA, Li N, Lynch K, Moy NB, Rashid M, Chang LC, Handler J, Brettler J, Rader F, et al. Sustainability of blood pressure reduction in black barbershops. Circulation. 2019;139:10–19. DOI: 10.1161/CIRCULATIONAHA.118.038165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whelton PK. The elusiveness of population‐wide high blood pressure control. Annu Rev Public Health. 2015;36:109–130. DOI: 10.1146/annurev-publhealth-031914-122949. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Health Statistics (NCHS) . Centers for Disease Control and Prevention (CDC). National Health and Nutrition Examination Survey Data (NHANES). Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2013–2016. [Google Scholar]
- 4.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310:46–56. DOI: 10.1001/jama.2013.6549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorodeski EZ, Goyal P, Cox ZL, Thibodeau JT, Reay RE, Rasmusson K, Rogers JG, Starling RC. Virtual visits for care of patients with heart failure in the era of COVID‐19: a statement from the Heart Failure Society of America. J Card Fail. 2020;26:448–456. DOI: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]


