Abstract
Introduction.
The tobacco and nicotine market is diversifying. Implications for public health will depend on trends in use, including overall use, and who is using these products. This study examined differences over time (2017-2019), across countries (Canada, England, US), and by smoking and vaping, in use of other tobacco/nicotine products and overall use.
Methods.
Online repeat cross-sectional surveys of youth age 16–19 in Canada (N=11,714), England (N=11,170), US (N=11,838) in 2017, 2018, 2019. Past-30-day use of tobacco/nicotine products (any, cigarette, e-cigarette, other combusted [cigars/cigarillos/waterpipe], other non-combusted [smokeless tobacco/nicotine replacement therapies (NRT)) were examined by country, year, and, for other combusted/non-combusted, past-30-day cigarette smoking and vaping. Use of emerging products (IQOS, nicotine pouches) was explored in 2018-2019.
Results.
From 2017-2019, use of any product increased in Canada (17.1-23.2%, AOR=1.07[95% CI=1.04-1.09]) and the US (18.0-24.0%, AOR=1.06[1.04-1.09]) but not England (20.8-21.7%, AOR=1.01[0.99-1.03]). Use of other combusted products (cigars/cigarillos/waterpipe) showed little change (Canada: 8.1-7.8%; England: 6.3-7.3%; US: 8.6-8.5%; p≥.151). Use of other non-combusted products (smokeless/NRT) increased in all countries (Canada: 1.5-3.2%, AOR=1.02[1.01-1.02]; England: 1.4-2.6%, AOR=1.02[1.01-1.03]; US: 3.3-4.9%, AOR=1.02[1.01-1.02]). Vaping increased in all countries (Canada: 8.4-17.8%; England: 8.7-12.6%; US: 11.1-18.5%; all p<.001). Smokers and vapers reported greater use of other combusted and non-combusted products than those who neither smoked/vaped (p<.001). Emerging product use was rare (≤1.5%).
Discussion.
Youth past-30-day tobacco/nicotine use increased from 2017-2019 in Canada and the US, largely due to increases in vaping and other non-combusted products. ‘Other’ tobacco/nicotine products were used predominantly by youth who smoked cigarettes and/or vaped.
Keywords: Adolescent, Electronic Nicotine Delivery Systems, Nicotine, Prevalence, Smoking, Surveys and Questionnaires, Tobacco Products
There is a continuum of risk across different tobacco and nicotine products, with combusted tobacco being the most harmful to health [1] and non-combusted nicotine products such as nicotine replacement therapies (NRT) being the least harmful [2,3]. Non-combusted tobacco products, such as snus, fall in between because they contain tobacco, and hence some toxicants, but avoid combustion [2,4]. E-cigarettes are also less harmful than combusted tobacco products because they do not contain tobacco or involve combustion [5]. Two new categories of products have also emerged in recent years: heated tobacco products (HTPs), such as IQOS, and tobacco-free oral nicotine pouches, such as Zyn and On!.
The diverse range of tobacco and nicotine products available has important implications for public health. Public health could be markedly improved if less harmful products displace smoking and/or facilitate smoking cessation or reduction [1,6,7]. On the other hand, public health could be negatively impacted if the range of products available increases or sustains overall tobacco use, or if individuals who would not have otherwise smoked use other nicotine products [6,7]. Monitoring tobacco and nicotine use across the spectrum of products, including overall, and who is using them, is therefore crucial.
Monitoring use among youth is of particular importance because tobacco and nicotine use is largely initiated by the age of 18 [8,9], with transitions to daily use predominantly occurring in late adolescence and young adulthood [10-12]. This period is also characterized by substantial poly-tobacco/nicotine use [13-15].
Canada, England, and the United States (US) are three countries with similar historical trends in smoking at the population level [16], but notable differences in the use of and policies surrounding other tobacco and nicotine products. In England, snus (but not other smokeless tobacco products) has been prohibited since 1992 under the European Tobacco Products Directive [17,18]. By contrast, snus and other smokeless tobacco products are widely available, marketed, and advertised in the US [6,19]. Smokeless tobacco is also widely available in Canada but is more tightly regulated, particularly with respect to marketing and labelling [20]. E-cigarettes have been commercially available and marketed in England and the US for over a decade. No nicotine-containing e-cigarettes were approved for sale or promotion in Canada until May 2018, although they were widely available prior to this time due to a lack of enforcement [21,22]. HTPs are an emerging category: IQOS, the most widely available HTP globally [23,24], was introduced to England and Canada in 2016, and to the US in October 2019. Similarly, tobacco-free oral nicotine pouches (e.g., Zyn, On!), which are not marketed as stop-smoking aids, were commercially available for sale and use in England and the US in 2019 [25].
Tobacco and nicotine use among youth in Canada, England, and the US has diversified in parallel with the market. Combusted cigarette smoking has decreased among youth in all three countries over the past two decades [8,26-28] and in 2019 the prevalence of current cigarette smoking was 5% among youth age 15-19 in Canada [29], 8.7% among youth age 16-17 in England [30], and 5.8% among students age 14-18 in the US [31]. The use of e-cigarettes (vaping) has increased in the past decade, although to a larger extent in Canada and the US than England [5,26,27,32,33]; for example, between 2017 and 2019 past 30-day vaping among 16-19-year-olds increased from 8.4-17.8% in Canada, 11.1-18.5% in the US, and 8.7-12.6% in England [28]. Similarly, increases have been observed for past-week vaping [5,32] and vaping on at least 20 of the past 30 days [32,33]. In 2019, vaping was more prevalent than smoking among youth in Canada and the US, but less prevalent than smoking in England [32].
In Canada and the US, use of smokeless tobacco has remained stable over the past decade, with fewer than 10% of US youth reporting past 30-day use [26] and a fewer than 5% of Canadian youth reporting ever use [27]. There are no available estimates for smokeless tobacco use of which we are aware among youth in England.
To our knowledge, no published studies directly compare prevalence of use across the spectrum of tobacco and nicotine products among youth in these three countries (Canada, England, US) with differing markets. There is also little data on the prevalence of the emerging categories of nicotine pouches and HTPs; these are particularly important to monitor because of the growing number of nicotine products available, and because IQOS and Marlboro heatsticks (or HEETs) have recently been approved by the US Food and Drug Administration (FDA) for marketing as a modified risk tobacco product [34]. In addition, little is known about between-country differences in patterns of poly-tobacco use. Such research is important to understand which products youth use and in what combination, how use is changing over time with the evolving market, and how regulatory environments shape patterns of use.
This paper has two primary objectives. First, to examine changes over time (2017-2019) and differences between Canada, England, and the US in use of tobacco and nicotine products, and whether changes over time vary by country. Second, to examine associations between past 30-day smoking and past 30-day vaping and use of other combusted and non-combusted tobacco and nicotine products, and whether these associations vary between Canada, England, and the US.
METHODS
The analysis plan was pre-registered on the Open Science Framework (available at osf.io/4nufm [35]).
Data source
Data were from the first three waves of the repeat cross-sectional International Tobacco Control Policy Evaluation Project (ITC) Youth Tobacco and Vaping Survey, conducted in Canada, England, and the US. A full description of the study methods can be found in the Technical Reports [36-38]. Briefly, online surveys were conducted in 2017 (July-August), 2018 (August-September), and 2019 (August-September). Respondents were recruited from the Nielsen Consumer Insights Global Panel and their partners’ panels. Eligible respondents included adolescents aged 16-19 at the time of recruitment. Nielsen also contacted panelists known to be parents; those who confirmed they had one or more children aged 16-19 living in their household were asked for permission for their son/daughter (whose birthday was next) to complete the survey. Respondents received remuneration according to their panel’s incentive structure (points-based/monetary rewards and/or prize draws). This study received ethics clearance through the University of Waterloo Research Ethics Committee (ORE#21847/31017) and the King’s College London Psychiatry, Nursing & Midwifery Research Ethics Subcommittee.
A total of n2017=13,468, n2018=13,427, and n2019=13,401 respondents completed the surveys, of whom n2017=12,128, n2018=11,753, and n2019=11,609 were retained in the cross-sectional samples. The following were excluded: respondents who failed data integrity checks (n2017=382; n2018=354; n2019=526), had missing or incomplete data on variables required for calculating weights or determining smoking or vaping status (n2017=958; n2018=158; n2019=194), were respondents recruited in a previous wave (n2018=1,115; n2019=1,023), or were outside the eligible age of recruitment (n2018=47; n2019=49).
Measures
Individual tobacco and nicotine product use
Measure wording [35-38] and coding methods [35] are publicly available online. Briefly, past 30-day use (yes, no) was assessed for “cigarette smoking,” “use of e-cigarettes/vaping,” “little cigars or cigarillos (plain or flavoured),” “cigars (not including little cigars or cigarillos, plain or flavoured),” “bidis (little cigarettes hand-rolled in leaves),” “a waterpipe to smoke shisha (herbal or tobacco),” “smokeless tobacco (chewing tobacco, pinch, snuff, or snus),” “nicotine patches, nicotine gum, nicotine lozenges, or other nicotine replacement therapies,” and, in 2019 only, “nicotine pouches WITHOUT tobacco (e.g., Zyn, On!, Velo)”. In 2018 and 2019 only, past 30-day use of IQOS (yes, no) was assessed by presenting respondents with an image of IQOS and heatsticks and subsequently asking ever-users: “When was the last time you used this product, even one or two puffs?”. The analytic sample excludes those who responded with ‘Don’t know’ or ‘Refused’ for past 30-day smoking or vaping. ‘Don’t know’ or ‘Refused’ responses for use of other tobacco and nicotine products were coded as missing.
Grouped tobacco and nicotine product use (outcome variables)
For the main analyses, product use was grouped into past 30-day use of: (i) Cigarettes (yes, no); (ii) E-cigarettes (yes, no); (iii) Other combusted tobacco products (yes [yes to a least one of: cigars, little cigars/cigarillos, bidis, waterpipe], no [all other respondents]); (iv) Other non-combusted tobacco or nicotine products (yes [yes to a least one of: smokeless tobacco or NRT], no [all other respondents]); (v) Any tobacco or nicotine product (yes [yes to a least one of: cigarettes, e-cigarettes, cigars, little cigars/cigarillos, bidis, waterpipe, smokeless tobacco, or NRT], no [all other respondents]). Use of nicotine pouches and IQOS were not included in these grouped outcome variables because they were not assessed at all survey years.
Tobacco/nicotine product tried first and use of nicotine in e-cigarettes
The tobacco/nicotine product tried first was also explored (additional to pre-registration [35]) by asking respondents who had ever tried e-cigarettes and either ever tried cigarettes or other products, “Which product did you try first?”, followed by the above list of products that they had reported trying. Respondents who reported trying only one product were classified as having used that product first. Respondents who reported trying cigarettes and other product(s) (except e-cigarettes) were not asked which product they used first, and thus not classifiable.
Use of nicotine in e-cigarettes was also explored (additional to pre-registration [35]) by asking respondents who had used an e-cigarette in the past 30 days “Do the e-cigarettes, cartridges, pods, or e-liquids you currently use contain nicotine? Yes; No; Some have nicotine, some do not; I don’t know if they contain nicotine or not; Refused.” Respondents who reported ‘Yes’ or ‘Some have nicotine, some do not’ were coded as using nicotine in e-cigarettes.
Country and year (independent variables)
Independent variables were country (Canada, England, US) and survey year (2017, 2018, 2019).
Covariates and sample characteristic variables
Covariates were age group (16-17, 18-19), sex (male, female), and race/ethnicity (white only, other, don’t know/refused).
Analyses
Sample weighting
Cross-sectional post-stratification sample weights were constructed for each country. In 2017, weights were calibrated to national population statistics for sex-by-age-by-region in Canada and England, and for sex-by-age-by-region-by-race in the US. For the years 2018 and 2019, a raking algorithm was applied to compute weights calibrated to sex-by-age-by-region in Canada and England and sex-by-age-by-region-by-race in the US; student status; school grades; and past 30-day smoking trend in Canada and the US. Target figures for student status and school grades were obtained from the 2017 weighted survey estimates, while the past 30-day smoking trend was obtained from the National Youth Tobacco Survey (US) and the Canadian Student Tobacco Alcohol and Drugs Survey (Canada). Weights were rescaled to the sample size within each country. See the Technical Reports for further details [36-38].
Descriptive analyses
Demographic covariates and cigarette smoking and vaping behaviours were examined in each country at each year among the full sample (N=35,490). The prevalence of past 30-day use of tobacco and nicotine products (individually and grouped) were then examined in each country at each year, and prevalence of past 30-day use of any ‘other’ combusted and ‘other’ non-combusted products were examined in each country by past 30-day cigarette smoking and vaping; for these prevalence estimates, missing data were excluded pairwise to enhance accuracy.
Regression modelling
Logistic regression models were used to address the study aims.
First, to examine changes in tobacco and nicotine product use over time and differences across countries, unadjusted and adjusted (for demographic covariates) logistic regression models were used to assess associations between each grouped outcome and country and survey year. Country and survey year were entered simultaneously into the adjusted regression models, and the results reported. Canada was treated as the reference category for ‘country’ because it had the lowest prevalence of any tobacco/nicotine product use in 2017. Next, a country-by-year interaction term was added to the adjusted models to examine whether changes over time in product use varied across countries. Where there was some evidence for an interaction (p<.05), they were further examined by calculating and comparing the adjusted average predicted probabilities of each outcome (i.e., prevalence of each outcome when adjusting for demographic covariates) for each time point within each country. For consistency, the adjusted average predicted probabilities of each outcome were also reported where interactions were not significant (p≥.05; additional to pre-registration [35]). The year 2017 was treated as the reference category when comparing the predicted probabilities within each country.
Second, to examine differences in the use of ‘other’ combusted and non-combusted tobacco and nicotine products by past 30-day cigarette smoking and past 30-day vaping, unadjusted and adjusted (for demographic covariates, country, and survey year) logistic regression models were used to assess associations between these two outcomes and past 30-day smoking and past 30-day vaping (entered simultaneously into the adjusted regression models), and past 30-day smoking/vaping (entered separately into the adjusted regression models). Smoking-by-country and, separately, vaping-by-country interaction terms were then subsequently added to the adjusted models to examine whether associations with smoking and vaping varied across countries. Interactions were examined using the same method as described above.
Third, as a post-hoc analysis that was not pre-registered [35], a combined past 30-day cigarette smoking/vaping variable was generated to explore use of ‘other’ combusted and non-combusted tobacco and nicotine products by: neither past 30-day smoking nor vaping, past 30-day smoking only, past 30-day vaping only, both past 30-day smoking and vaping (mutually exclusive categories). Associations between this smoking/vaping variable, and country interactions, and use of ‘other’ combusted and non-combusted tobacco and nicotine products were explored using the same method as described above.
Stata v15 was used for descriptive analyses and regression modelling using survey commands.
Missing data in the regression models
Data were excluded listwise for all regression models (resulting in N=32,525) for three reasons: 1) to make comparisons consistent through ensuring samples were the same; 2) because data were only missing on outcomes [39]; and, 3) sample size, and hence power, was large [40]. Respondents who were excluded from the regression models were less likely to be white and more likely to be age 18-19, male, smokers, and vapers than those who were retained in the models (Table A3, Appendix).
RESULTS
Sample characteristics
Table 1 shows the characteristics of the weighted cross-sectional samples in each country at each year.
Table 1.
Sample characteristics by year and country. N=35,490.
| CANADA |
ENGLAND |
US |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 2017 (n=4038) |
2018 (n=3845) |
2019 (n=4135) |
2017 (n=3995) |
2018 (n=3874) |
2019 (n=3493) |
2017 (n=4095) |
2018 (n=4034) |
2019 (n=3981) |
|
| AGE GROUP | |||||||||
| 16-17 | 48.0 (1566) | 47.7 (1427) | 47.4 (1738) | 48.6 (1584) | 48.4 (1149) | 48.7 (1497) | 50.3 (1772) | 49.6 (2011) | 49.6 (1657) |
| 18-19 | 52.0 (2420) | 52.3 (2289) | 52.6 (2274) | 51.4 (2357) | 51.6 (2658) | 51.3 (1925) | 49.7 (2246) | 50.4 (1937) | 50.4 (2215) |
| SEX | |||||||||
| Male | 51.3 (1388) | 51.0 (1706) | 51.2 (1495) | 51.2 (1674) | 51.0 (1362) | 51.2 (1205) | 51.0 (1584) | 51.0 (1407) | 51.1 (1195) |
| Female | 48.7 (2598) | 49.0 (2010) | 48.8 (2517) | 48.8 (2267) | 49.0 (2445) | 48.8 (2217) | 49.0 (2434) | 49.0 (2541) | 48.9 (2677) |
| RACE/ETHNICITY | |||||||||
| White (only) | 58.4 (2143) | 47.5 (1774) | 54.1 (2190) | 79.4 (3090) | 77.6 (2862) | 76.1 (2572) | 73.6 (2641) | 73.7 (2451) | 73.8 (2127) |
| Other | 39.8 (1768) | 45.6 (1672) | 43.1 (1706) | 19.5 (811) | 21.3 (902) | 22.6 (801) | 26.0 (1355) | 25.6 (1464) | 25.7 (1712) |
| Don’t know/refused | 1.8 (75) | 7.0 (270) | 2.8 (116) | 1.1 (40) | 1.2 (43) | 1.2 (49) | 0.5 (22) | 0.7 (33) | 0.5 (33) |
| CIGARETTE SMOKING 1 | |||||||||
| Ever | 31.9 (1209) | 31.0 (1424) | 31.1 (1505) | 40.4 (1655) | 40.1 (1598) | 38.2 (1396) | 32.3 (1341) | 32.4 (1272) | 33.5 (1539) |
| Past 12 months | 20.5 (767) | 19.6 (966) | 19.6 (1007) | 29.4 (1222) | 29.6 (1184) | 26.8 (1003) | 20.5 (836) | 20.7 (811) | 18.4 (956) |
| Past week | 7.6 (266) | 7.6 (450) | 7.0 (424) | 9.8 (404) | 11.5 (430) | 10.2 (411) | 8.5 (333) | 8.3 (317) | 5.8 (402) |
| Smoked ≥20 of the past 30 days | 4.3 (139) | 4.1 (239) | 2.9 (184) | 4.3 (180) | 5.8 (204) | 4.7 (195) | 3.7 (145) | 3.9 (147) | 2.5 (185) |
| VAPING 1 | |||||||||
| Ever | 29.3 (1136) | 33.2 (1445) | 40.6 (1917) | 33.7 (1344) | 33.1 (1292) | 36.1 (1346) | 31.3 (1336) | 33.1 (1354) | 43.6 (1902) |
| Past 12 months | 21.0 (799) | 25.4 (1124) | 34.1 (1623) | 24.1 (954) | 24.0 (900) | 27.1 (1007) | 23.7 (991) | 27.1 (1092) | 35.4 (1574) |
| Past week | 5.2 (173) | 7.5 (353) | 12.3 (627) | 4.6 (179) | 4.6 (155) | 6.9 (251) | 6.4 (257) | 10.3 (396) | 12.6 (616) |
| Vaped ≥20 of the past 30 days | 1.8 (55) | 2.4 (108) | 5.7 (292) | 1.5 (55) | 2.0 (63) | 2.7 (90) | 2.2 (81) | 3.8 (145) | 6.7 (299) |
Data are weighted % (unweighted n).
Categories are not mutually exclusive.
Prevalence of past 30-day use of tobacco and nicotine products
Figure 1 shows the prevalence of past 30-day use of tobacco and nicotine products in each country at each year. As reported previously [36-38], the most commonly used product in the past 30 days was e-cigarettes in Canada and the US, and cigarettes in England. Past 30-day use of bidis, nicotine pouches, and IQOS were low in all three countries (≤1.7%) and past 30-day use of smokeless tobacco was also low in Canada and England (≤2.0%).
Figure 1. Prevalence of past 30-day use of tobacco and nicotine products in Canada, England, and the US in 2017, 2018, and 2019. Data are weighted.
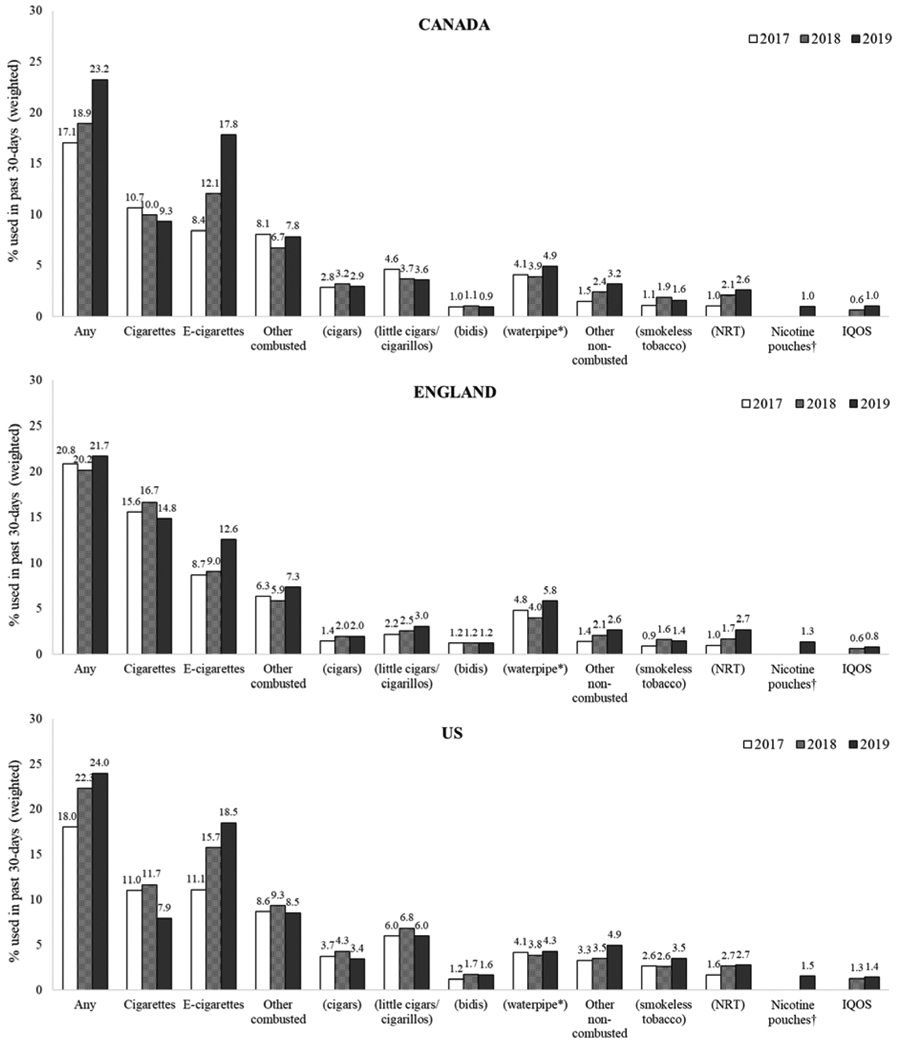
Sample sizes vary for each product due to pair wise deletion of ‘Don’t know’ and ‘Refused’ responses (see Appendix Table A1). *Included herbal or tobacco, †Without tobacco. NRT=Nicotine Replacement Therapy.
Past-30-day use of nicotine pouches was not assessed in 2017 or 2018.
Past-30-day use of IQOS was not assessed at 2017.
Tobacco/nicotine product tried first and use of nicotine in e-cigarettes
Among respondents who had ever tried cigarettes, e-cigarettes, or other products (n=17,747), 42.4% had tried cigarettes first, 34.8% had tried e-cigarettes first, 10.6% had tried other products first, and 12.2% refused, did not know, or were unclassifiable. Among respondents who had vaped in the past 30 days (n=3,401), 82.8% vaped nicotine.
Changes over time and across countries tobacco and nicotine product use
Table 2 shows estimates from logistic regression models assessing the associations between past 30-day use of tobacco and nicotine products and year and country, adjusting for demographic covariates. Findings were similar in unadjusted models (Table A4).
Table 2.
Adjusted associations between past 30-day use of tobacco and nicotine products and: country, year, past 30-day cigarette smoking, past 30-day vaping, and past 30-day cigarette smoking/vaping. N=32,525.
| Past 30-day use of |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Any1 |
Cigarettes (smoking) |
E-cigarettes (vaping) |
Other combusted2 |
Other non-combusted3 |
||||||
| AOR (95% CI) | p | AOR (95% CI) | p | AOR (95% CI) | p | AOR (95% CI) | p | AOR (95% CI) | p | |
| COUNTRY 4 | ||||||||||
| Canada (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| England | 1.02 (0.95-1.10) | .624 | 1.58 (1.44-1.73) | <.001 | 0.72 (0.65-0.79) | <.001 | 0.88 (0.78-0.99) | .036 | 0.85 (0.69-1.04) | .119 |
| US | 1.06 (0.98-1.14) | .129 | 0.99 (0.90-1.10) | .898 | 1.18 (1.08-1.29) | <.001 | 1.23 (1.10-1.37) | <.001 | 1.68 (1.41-2.01) | <.001 |
| YEAR 4 | ||||||||||
| 2017 (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 2018 | 1.14 (1.06-1.23) | .001 | 1.00 (0.91-1.09) | .982 | 1.37 (1.25-1.52) | <.001 | 0.95 (0.85-1.06) | .344 | 1.30 (1.07-1.58) | .009 |
| 2019 | 1.31 (1.22-1.41) | <.001 | 0.83 (0.76-0.91) | <.001 | 1.92 (1.75-2.11) | <.001 | 1.02 (0.92-1.14) | .677 | 1.78 (1.47-2.16) | <.001 |
| PAST 30-DAY CIGARETTE SMOKING 5 | ||||||||||
| No (ref) | - | - | - | - | 1.00 | 1.00 | ||||
| Yes | - | - | - | - | 8.16 (7.21-9.23) | <.001 | 8.84 (7.20-10.85) | <.001 | ||
| PAST 30-DAY VAPING 5 | ||||||||||
| No (ref) | - | - | - | - | 1.00 | 1.00 | ||||
| Yes | - | - | - | - | 5.73 (5.06-6.48) | <.001 | 4.58 (3.73-5.62) | <.001 | ||
| PAST 30-DAY CIGARETTE SMOKING/VAPING 6 | ||||||||||
| Neither (ref) | - | - | - | - | 1.00 | 1.00 | ||||
| Cigarettes only | - | - | - | - | 13.93 (12.07-16.08) | <.001 | 15.13 (11.70-19.56) | <.001 | ||
| E-cigarettes only | - | - | - | - | 9.89 (8.52-11.47) | <.001 | 8.35 (6.29-11.08) | <.001 | ||
| Both | - | - | - | - | 40.62 (35.34-46.69) | <.001 | 43.12 (34.38-54.08) | <.001 | ||
Associations in bold indicate where p<.01.
Data are weighted.
At least one of: cigarettes, e-cigarettes, cigars, little cigars/cigarillos, bidis, waterpipe, smokeless tobacco, NRT.
At least one of: cigars, little cigars/cigarillos, bidis, waterpipe.
At least one of: smokeless tobacco, nicotine replacement therapy (NRT).
From pre-registered model assessing associations between outcomes and: demographic covariates (age group, sex, race/ethnicity), country, and year.
From pre-registered model assessing associations between outcomes and: demographic covariates (age group, sex, race/ethnicity), country, year, past-30-day cigarette smoking, and past-30-day vaping.
From exploratory model assessing associations between outcomes and: demographic covariates (age group, sex, race/ethnicity), country, year, and past-30-day cigarette smoking/vaping.
Differences between countries and over time in past 30-day smoking and vaping have been reported on previously [32,41,42], so only the findings for other combusted, other non-combusted, and any tobacco and nicotine product use are discussed here.
Any product
Past 30-day use of any tobacco or nicotine product increased overall between 2017 and 2019 such that, compared to 2017, respondents had 1.31 times the odds of using any product in 2019 (p<.001; Table 2). There was little evidence for differences between countries (Table 2). There was an interaction between year and country (F(4,32521)=5.52, p<.001), such that use increased between 2017 and 2019 in Canada (AOR=1.07 [1.04-1.09], p<.001) and the US (AOR=1.06 [1.04-1.09], p<.001) but not England (AOR=1.01 [0.994-1.03], p=.179). See Figure 1 for unadjusted patterns of use across countries and over time, and Table A5 for all adjusted comparisons.
‘Other’ combusted
Past 30-day use of ‘other’ combusted tobacco products was more prevalent in the US than in Canada and England (p<.001), but there was little evidence of overall change from 2017 to 2019 (Table 2). There was little evidence of an interaction between year and country (F(4,32521)=2.26, p=.060), such that trends between 2017 and 2019 were similar in all three countries (Canada: AOR=1.00 [0.98-1.01], p=.521; US: AOR=1.01 [1.00-1.02], p=.151; England: AOR=1.00 [0.99-1.01], p=.971) (Figure 1, Table A5).
‘Other’ non-combusted
Past 30-day use of ‘other’ non-combusted tobacco or nicotine products was more prevalent in the US than in Canada and England, and increased between 2017 and 2019 (Table 2). There was little evidence of an interaction between year and country (F(4,32521)=0.98, p=.417) such that trends between 2017 and 2019 were similar in all three countries (Canada: AOR=1.02 [1.01-1.02], p<.001; US: AOR=1.02 [1.01-1.02], p<.001; England: AOR=1.02 [1.01-1.03], p<.001) (Figure 1, Table A5).
Associations between use of ‘other’ combusted and non-combusted tobacco and nicotine products and smoking and vaping, by country
Table 2 shows estimates from the logistic regression models assessing the associations between past 30-day use of ‘other’ combusted and non-combusted tobacco and nicotine products and past 30-day cigarette smoking, and past 30-day vaping, adjusting for year, country, and demographic covariates. Findings were similar in unadjusted models (Table A4).
‘Other’ combusted
Overall, past 30-day use of ‘other’ combusted tobacco products was more prevalent among youth who had smoked cigarettes in the past 30 days (Table 2). Specifically, cigarette smokers had 8.16 times the odds of using other combusted tobacco products than non-smokers of cigarettes (p<.001; Table 2). There was strong evidence of an interaction between country and smoking (F(2,32523)=14.34, p<.001), such that the differences in prevalence between smokers and non-smokers were greater in Canada (AOR=1.26 [1.22-1.29], p<.001) and the US (AOR=1.29 [1.25-1.33], p=<.001) than England (AOR=1.15 [1.13-1.18], p<.001).
See Figure 2 for unadjusted patterns of use across countries, and Table A6 for all adjusted comparisons.
Figure 2. Prevalence of past 30-day use of other combusted and other non-combusted tobacco and nicotine products in Canada, England, and the US by past 30-day cigarette smoking, past 30-day vaping, and past 30-day cigarette smoking/vaping. N=32,525.
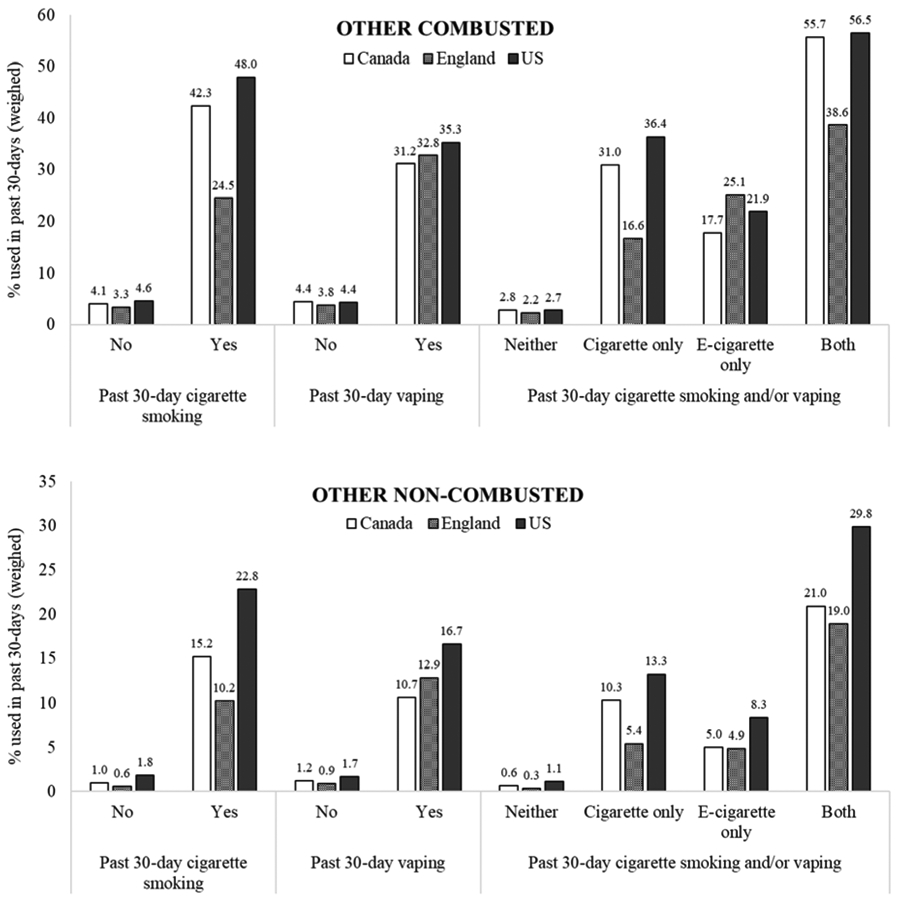
% are derived from weighted data. N are derived from unweighted data.
Other combusted: At least one of: cigars, little cigars/cigarillos, bidis, waterpipe.
Other non-combusted: At least one of: smokeless tobacco, nicotine replacement therapy (NRT).
Analyses for combined past 30-day cigarette smoking/vaping (final panel) were not pre-registered and are hence exploratory.
Overall, past 30-day use of ‘other’ combusted products was more prevalent among youth who had vaped in the past 30 days (Table 2). There was little evidence of an interaction between country and past 30-day vaping (F(2,32523)=0.70, p=.498), such that patterns were similar across all three countries (Canada: AOR=1.16 [1.13-1.18], p<.001; England: AOR=1.13 [1.10-1.15], p<.001; US: AOR=1.20 [1.17-1.23], p<.001) (Figure 2, Table A6).
Post-hoc analyses using the combined smoking/vaping variable indicated that use of ‘other’ combusted products was highest overall among past 30-day cigarette smokers and vapers, followed by smokers-only, vapers-only, and lowest among neither smokers/vapers (Table 2), although there was strong evidence that patterns differed across countries (F(6,32519)=8.85, p<.001; Figure 2). In Canada and the US, compared with youth who had neither smoked nor vaped, use of ‘other’ combusted products was more strongly associated with smoking only (Canada: AOR=1.31 [1.26-1.36], p<.001; US: AOR=1.40 [1.34-1.47], p<.001) than vaping only (Canada: AOR=1.16 [1.13-1.19], p<.001; US: AOR=1.22 [1.18-1.26], p<.001), while the reverse was true in England (smoking only vs. neither: AOR=1.18 [1.15-1.21], p<.001; vaping only vs. neither: AOR=1.25 [1.20-1.30], p<.001) (Figure 2, Table A6).
‘Other’ non-combusted
Overall, past 30-day use of ‘other’ non-combusted tobacco or nicotine products was more prevalent among youth who had smoked cigarettes in the past 30 days and youth who had vaped in the past 30 days (Table 2). Post-hoc analyses indicated use was highest among youth who had both smoked and vaped, followed by youth who had only smoked, only vaped, and lowest among those who used neither (Table 2). There was little evidence of interactions between country and smoking (F(2,32523)=1.22, p=.295), vaping (F(2,32523)=1.49, p=.226), or combined smoking/vaping (F(6,32519)=1.39, p=.214), indicating patterns were similar across countries (Figure 2, Table A6).
DISCUSSION
Findings suggest that young people age 16-19 in England, Canada, and the US use a range of tobacco and nicotine products. E-cigarettes were the most commonly used product in the past 30 days in Canada and the US, while cigarettes were most common in England. Between 2017 and 2019, there was an increase in overall use of nicotine and tobacco products in the past 30 days only in Canada and the US, which appeared to be driven by increases in use of e-cigarettes and other non-combusted products (smokeless tobacco and NRT). Use of nicotine pouches and IQOS was negligible in all three countries. Poly-tobacco/nicotine product use was common, with most youth who used other combusted or non-combusted products in the past 30 days also being past 30-day cigarette smokers and/or vapers.
There were several between-country differences in product use, largely consistent with recent and historical research. As reported previously from this dataset [32], England continues to have lower prevalence of vaping compared with Canada and the US. At the time of this study, in England e-cigarettes were subject to greater marketing restrictions than Canada and the US, and nicotine concentration was limited to a maximum of 20mg/ml [18]. Consistent with previous US [26] and Canadian [27] data and the prohibition of snus in England [17,18], prevalence of other non-combusted tobacco products – namely smokeless tobacco – was highest in the US compared with England and Canada. Use of other combusted tobacco products (cigars, cigarillos, bidis, waterpipe) was also higher in the US than Canada and England. Despite these differences for individual product types, there was little evidence to suggest that overall use of nicotine/tobacco products differed across countries; higher prevalence of cigarette smoking in England may offset higher prevalence of other product use in the US and Canada.
Product use also differed over time. Overall tobacco/nicotine use increased between 2017 and 2019 in the US and Canada, but not England, and this appears to be driven by increases in vaping and use of non-combusted products. Increases in youth vaping and smokeless tobacco use in the US and Canada are consistent with previous work [26,27,32,33,43] and with the approval of nicotine-containing e-cigarettes in Canada in 2018 [21] (although they were widely available beforehand [20]). Further, youth use of e-cigarettes and smokeless tobacco – two products that are subject to greater restrictions in England than Canada and the US [18] – remained relatively stable in England.
The impact of the overall increase in tobacco/nicotine product use on public health is unclear. On one hand, cigarette smoking has continued to decline, and vaping and use of non-combustibles have lower relative risk [2,3,5]; therefore, the harm-weighted impact on public health may be minimal or even positive. On the other, increases in overall tobacco/nicotine use among youth are concerning, because this is inconsistent with the idea that less harmful products are completely substituting or displacing cigarette smoking, and because smoking has been declining prior to the introduction of emerging products [8,26,27]. Longer-term trends of these emerging products (including more frequent use), associated harms, and influence on youth combustible tobacco use also remain to be seen. In particular, it remains to be seen whether the increase in frequent vaping among youth in the US and Canada [32] will be sustained over time.
Poly-tobacco/nicotine product use was common among youth who used other combusted and non-combusted products in the past 30 days, consistent with previous research from the US [15,43,44] and Canada [45]. Use of these products was highest among concurrent cigarette smokers and vapers, suggesting that youth who use these other products may have broad risk-taking profiles that predispose them to experiment with multiple tobacco/nicotine products. Importantly, use of other combusted and non-combusted products was rare among youth who had not smoked cigarettes or vaped in the past 30 days, and most had tried smoking cigarettes first.
Importantly, patterns of poly-tobacco/nicotine use varied between the three countries. In Canada and the US, use of other combusted and non-combusted products in the past 30 days was more common among cigarette smokers than vapers, although this was not the case in England. This may be because of the different profiles of smokers and vapers in the three countries [32]; future research is required to explore those youth who use multiple tobacco/nicotine products across countries to help understand why these differences emerge.
Limitations and strengths
This study has several limitations. First, in regression analyses we excluded respondents who refused to answer or did not know their use of ‘other’ tobacco and nicotine products. These individuals were more likely to be past 30-day cigarette smokers, vapers, and differed on key sociodemographic variables, potentially biasing the findings. Despite this, findings are in line with previous studies using the full sample [32]. Second, past 30-day product use cannot be generalised to regular or long-term use, which is of primary concern to public health. Measures of more frequent or long-term use of cigars, cigarillos, bidis, waterpipe, smokeless tobacco, or NRT were not available in this survey. Third, we classified e-cigarettes as a nicotine product, although e-cigarettes do not always contain nicotine. Fourth, we were unable to adjust for socio-economic status (SES; a key risk factor for smoking [46]) in our analyses because this was not consistently measured across survey years. However, the sample weights accounted for student status and school grades, and education is often used as an SES indicator [47]. Fifth, while data for Canada and the US were weighted to reflect known trends in smoking, data for England were not, due to lack of national estimates for smoking status among this age group. However, both weighted and unweighted estimates were similar to national benchmark surveys in each country [36-38]. A key strength of this study was the large sample, which allowed for assessment of different user status groups and interactions with country.
Conclusions
Use of tobacco and nicotine products is diversifying among youth in Canada, England, and the US. Past 30-day use of tobacco and nicotine products increased between 2017 and 2019 in Canada and the US, and this appeared to be driven by increases in use of e-cigarettes and other non-combusted products. Use of ‘other’ combusted (cigars, cigarillos, bidis, waterpipe) and non-combusted (smokeless tobacco, NRT) products was most prevalent in the US, consistent with historical trends and availability. Use of these ‘other’ products was largely restricted to youth who had smoked cigarettes and/or vaped in the past 30 days.
Supplementary Material
IMPLICATIONS AND CONTRIBUTION.
Youth use of tobacco/nicotine products is diversifying. Past-30-day use of any product increased from 2017-2019 in Canada and the US, attributable largely to increases in e-cigarettes and other non-combusted products (smokeless tobacco/NRT). Other combusted (cigars/cigarillos/waterpipe) and non-combusted products were predominantly used by smokers and/or vapers. IQOS and nicotine pouch use were rare.
Acknowledgments
Funding. This work was supported by a P01 Grant (1P01CA200512-01) from the US National Institutes of Health. Additional support was provided by a Canadian Institutes of Health Research (CIHR)–Public Health Agency of Canada (PHAC) Applied Public Health Research Chair (DH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests. DH has served as a paid expert witness in legal challenges against tobacco companies. KAE, JLR & VLR have no potential conflicts of interest to disclose.
REFERENCES
- 1.Cummings KM, Ballin S, Sweanor D. The past is not the future in tobacco control. Preventive Medicine. 2020:106183. doi: 10.1016/j.ypmed.2020.106183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benowitz NL. Emerging nicotine delivery products. Implications for public health. Ann Am Thorac Soc. 2014;11(2):231–235. doi: 10.1513/AnnalsATS.201312-433PS. [DOI] [PubMed] [Google Scholar]
- 3.McNeill A, Munafo MR. Reducing harm from tobacco use. J Psychopharmacol. 2013;27(1):13–18. doi: 10.1177/0269881112458731. [DOI] [PubMed] [Google Scholar]
- 4.Levy DT, Mumford EA, Cummings KM, Gilpin EA, Giovino G, Hyland A, Sweanor D, Warner KE. The Relative Risks of a Low-Nitrosamine Smokeless Tobacco Product Compared with Smoking Cigarettes: Estimates of a Panel of Experts. Cancer Epidemiol Biomarkers Prev. 2004. doi. [PubMed] [Google Scholar]
- 5.McNeill A, Brose LS, Calder R, Bauld L, Robson D. Vaping in England: an evidence update including mental health and pregnancy, March 2020: A report commissioned by Public Health England. 2020. https://www.gov.uk/government/publications/vaping-in-england-evidence-update-march-2020.
- 6.Levy DT, Mays D, Boyle RG, Tam J, Chaloupka FJ. The Effect of Tobacco Control Policies on US Smokeless Tobacco Use: A Structured Review. Nicotine Tob Res. 2017;20(1):3–11. doi: 10.1093/ntr/ntw291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy DT, Cummings KM, Villanti AC, Niaura R, Abrams DB, Fong GT, Borland R. A framework for evaluating the public health impact of e-cigarettes and other vaporized nicotine products. Addiction. 2017; 112(1):8–17. doi: 10.1111/add.13394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services. The health consequences of smoking - 50 years of progress: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf. [Google Scholar]
- 9.Office for National Statistics. General Lifestyle Survey 2008: Smoking and drinking among adults. 2010. www.ons.gov.uk/ons/rel/ghs/general-lifestyle-survey/2008-report/smoking-and-drinking-among-adults--2008.pdf.
- 10.Hammond D Smoking behaviour among young adults: beyond youth prevention. Tob Control. 2005;14(3):181–185. doi: 10.1136/tc.2004.009621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cantrell J, Bennett M, Mowery P, Xiao H, Rath J, Hair E, Vallone D. Patterns in first and daily cigarette initiation among youth and young adults from 2002 to 2015. PloS One. 2018; 13(8). doi: 10.1371/journal.pone.0200827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sussman S, Arnett JJ. Emerging Adulthood:Developmental Period Facilitative of the Addictions. Evaluation & the Health Professions. 2014;37(2):147–155. doi: 10.1177/0163278714521812. [DOI] [PubMed] [Google Scholar]
- 13.Niaura R, Rich I, Johnson AL, Villanti AC, Romberg AR, Hair EC, Vallone DM, Abrams DB. Young Adult Tobacco and E-cigarette Use Transitions: Examining Stability using Multi-State Modeling. Nicotine and Tobacco Research. 2019. doi: 10.1093/ntr/ntz030. [DOI] [PubMed] [Google Scholar]
- 14.Loukas A, Marti CN, Perry CL. Trajectories of Tobacco and Nicotine Use Across Young Adulthood, Texas, 2014-2017. Am J Public Health. 2019;109(3):465–471. doi: 10.2105/ajph.2018.304850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor KA, Sharma E, Edwards KC, Halenar MJ, Kissin W, Kasza KA, Day H, Anic G, Gardner LD, Hammad HT, Hull LC, Bansal-Travers M, Limpert J, Borek N, Kimmel HL, Compton WM, Hyland A, Stanton C. Longitudinal pathways of exclusive and polytobacco cigarette use among youth, young adults and adults in the USA: findings from the PATH Study Waves 1-3 (2013-2016). Tob Control. 2020;29(Suppl 3):s139–s146. doi: 10.1136/tobaccocontrol-2020-055630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organisation. WHO global report on trends in prevalence of tobacco smoking 2000–2025, secondedition.2018. [Google Scholar]
- 17.The European Parliament and the Council of the European Union. Council Directive 89/622/EEC of 13 November 1989 on the approximation of the laws, regulations and administrative provisions of the Member States concerning the labelling of tobacco products and the prohibition of the marketing of certain types of tobacco for oral use. 1989. doi.
- 18.The European Parliament and the Council of the European Union. Directive 2014/40/EU of the European Parliament and of the Council. In. Official Journal of the European Union,2014. doi. [Google Scholar]
- 19.Federal Trade Commission. Federal Trade Commission Smokeless Tobacco Report for 2018. 2018. https://www.ftc.gov/reports/federal-trade-commission-cigarette-report-2018-smokeless-tobacco-report-2018.
- 20.Government of Canada. Tobacco and Vaping Products Act. 2018; https://laws-lois.justice.gc.ca/eng/acts/T-11.5/.
- 21.Hammond D, White CM, Czoli CD, Martin CL, Magennis P, Shiplo S. Retail availability and marketing of electronic cigarettes in Canada. Canadian Journal of Public Health. 2015;106(6):e408–412. doi: 10.17269/cjph.106.5105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Health Canada. Vaping products. 2019; https://www.canada.ca/en/health-canada/news/2019/12/backgrounder-regulation-of-vaping-products-in-canada.html.Accessed 12th November 2018, 2018.
- 23.Philip Morris International. Philip Morris International 2018 Annual Report. 2018. https://philipmorrisinternational.gcs-web.com/static-files/824f3f55-f97f-4f8f-bcb8-d00aa4dc65b1.
- 24.World Health Organisation. Heated tobacco Products Information Sheet. 2020.
- 25.British American Tobacco. Discover modern oral products. 2020; https://www.bat-science.com/groupms/sites/BAT_B9JBW3.nsf/vwPagesWebLive/DOBBZD34.
- 26.Wang TW, Gentzke A, Sharapova S, Cullen KA, Ambrose BK, Jamal A. Tobacco Product Use Among Middle and High School Students - United States, 2011-2017. MMWR Morb Mortal Wkly Rep. 2018;67(22):629–633. doi: 10.15585/mmwr.mm6722a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reid JL, Hammond D, Tariq U, Burkhalter R, Rynard VL, Douglas O. Tobacco Use in Canada: Patterns and Trends, 2019Edition.Waterloo, ON: Propel Centre for Population Health Impact, University of Waterloo. 2019. https://uwaterloo.ca/tobacco-use-canada/tobacco-use-canada-patterns-and-trends. [Google Scholar]
- 28.Action on Smoking and Health. Young people and smoking. 2019.
- 29.Health Canada. Canadian Tobacco and Nicotine Survey (CTNS): summary of results for 2019. 2020; https://www.canada.ca/en/health-canada/services/canadian-tobacco-nicotine-survey/2019-summary.html.
- 30.West R, Kale D, Kock L, Brown J. Top-line findings on smoking in England from the Smoking Toolkit Study. 2021; http://www.smokinginengland.info/latest-statistics/.
- 31.Wang TW, Gentzke AS, Creamer MR, Cullen KA, Holder-Hayes E, Sawdey MD, Anic GM, Portnoy DB, Hu S, Homa DM, Jamal A, Neff LJ. Tobacco Product Use and Associated Factors Among Middle and High School Students - United States, 2019. MMWR: Surveillance Summaries. 2019;68(12):1–22. doi: 10.15585/mmwr.ss6812a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hammond D, Rynard VL, Reid JL. Changes in Prevalence of Vaping Among Youths in the United States, Canada, and England from 2017 to 2019. JAMA Pediatrics. 2020;174(8):797–800. doi: 10.1001/jamapediatrics.2020.0901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farsalinos K, Barbouni A, Niaura R. Changes from 2017 to 2018 in e-cigarette use and in ever marijuana use with e-cigarettes among US adolescents: analysis of the National Youth Tobacco Survey. Addiction. 2020. doi: 10.1111/add.15162. [DOI] [PubMed] [Google Scholar]
- 34.Food and Drug Administration. Philip Morris Products S.A. Modified Risk Tobacco Product (MRTP) Modified Risk Order 2020. https://www.fda.gov/tobacco-products/advertising-and-promotion/philip-morris-products-sa-modified-risk-tobacco-product-mrtp-applications#E.
- 35.East K, Reid JL, Rynard V, Hammond D. Prevalence and trends of tobacco and nicotine product use among youth in Canada, the US, and England from 2017-2019. Open Science Framework,. 2020. doi: 10.17605/OSF.IO/4NUFM. [DOI] [Google Scholar]
- 36.Hammond D, Reid JL, White CM, Boudreau C. ITC Youth Tobacco and E-cigarette Survey: Technical report - Wave 1 (2017): Version 2.0 2019; http://davidhammond.ca/wp-content/uploads/2019/12/ITC_P3-Youth_Wave1_TechnicalReport_v2_2019.pdf.
- 37.Hammond D, Reid JL, Rynard VL, Boudreau C. ITC Youth Tobacco And Vaping Survey: Technical Report – Wave 2 (2018). 2020; http://davidhammond.ca/wp-content/uploads/2020/05/2018_P01P3_W2_Technical-Report_updated202005.pdf.
- 38.Hammond D, Reid JL, Rynard VL, Burkhalter R. ITC Youth Tobacco and E-cigarette Survey: Technical report - Wave 3 (2019). 2020; http://davidhammond.ca/wp-content/uploads/2020/05/2019_P01P3_W3_Technical-Report_updated202005.pdf.
- 39.Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials - a practical guide with flowcharts. BMC Med Res Methodol. 2017;17(1): 162. doi: 10.1186/s12874-017-0442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Allison PD. Missing Data. In: Quantitative Applications in the Social Sciences. Vol 136. SAGE Publications, Inc; 2001. [Google Scholar]
- 41.Hammond D, Reid JL, Rynard VL, Fong GT, Cummings KM, McNeill A, Hitchman S, Thrasher JF, Goniewicz M, Bansal-Travers M, O'Connor R, Levy D, Borland R, White CM. Prevalence of vaping and smoking among adolescents in Canada, England, and the United States: Repeat national cross sectional surveys. British Medical Journal. 2019;365(l2219). doi: 10.1136/bmj.l2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hammond D, Reid JL, Rynard VL, Fong GT, Cummings KM, McNeill A, Hitchman S, Thrasher JF, Goniewicz M, Bansal-Travers M, O'Connor R, Levy D, Borland R, White CM. Correction: Prevalence of vaping and smoking among adolescents in Canada, England, and the United States: Repeat national cross sectional surveys. British Medical Journal. 2020;370(m2579). doi: 10.1136/bmj.m2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nasim A, Khader Y, Blank MD, Cobb CO, Eissenberg T. Trends in alternative tobacco use among light, moderate, and heavy smokers in adolescence, 1999-2009. Addict Behav. 2012;37(7):866–870. doi: 10.1016/j.addbeh.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.El-Toukhy S, Choi K. A Risk-Continuum Categorization of Product Use Among US Youth Tobacco Users. Nicotine Tob Res. 2016;18(7):1596–1605. doi: 10.1093/ntr/ntw008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Milicic S, Kennedy RD, Burkhalter R. Canadian Youth Smokeless Tobacco Use – Flavored Product Regulation Insights. Tobacco Regulatory Science. 2018;4(3):88–95. doi: 10.18001/trs.4.3.8. [DOI] [Google Scholar]
- 46.Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M. Socioeconomic status and smoking: A review. Annals of the New York Academy of Sciences. 2012;1248:107–123. doi: 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- 47.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60(1):7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


