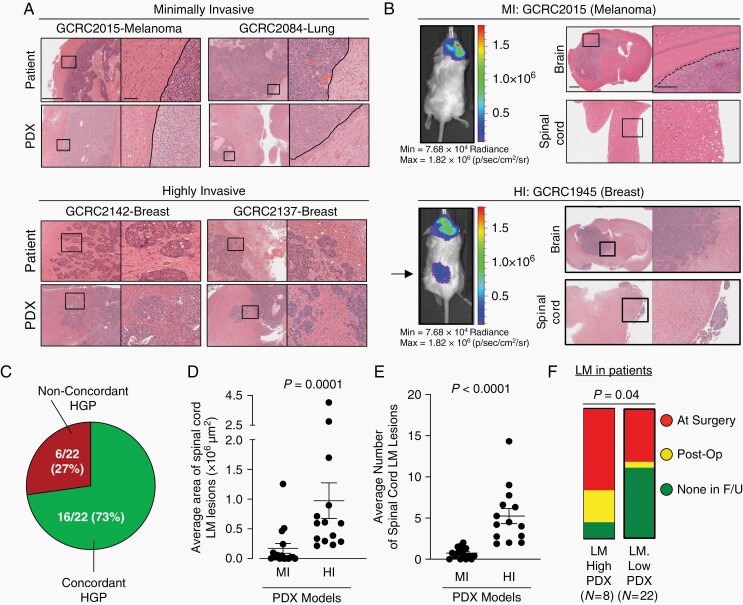
Fig. 3.
PDX models of brain metastasis retain invasion pattern from patient of origin and are associated with patterns of leptomeningeal dissemination. A, Examples of margins from MI (top) and HI (bottom) PDX models of brain metastasis with matched patient specimens demonstrating the same invasion pattern. Scale bars: 1 mm (low magnification), 100 µm (high magnification). B, Representative images of PDX models with MI invasion pattern (top) remaining localized in the brain parenchyma while those with HI invasion pattern (bottom) are more likely to develop leptomeningeal metastases surrounding the brain and spinal cord, shown by both IVIS (left; arrow points to spinal cord leptomeningeal metastases) and histology (right). Scale bars: 1 mm, 500 µm. C, Ratio of invasion pattern concordance between patient and matched PDX models D, Quantification of leptomeningeal metastases area (µm2 per mouse spinal cord) and E, number of lesions, between MI (n = 16) and HI (n = 14) independent brain metastasis PDX models. For each PDX model, 1 H&E-stained slide from 3 to 5 mice were assessed and averaged for analysis. Statistical analyses were performed using a two-sided Mann-Whitney test. F, High- and low-LM-forming PDXs with associated patient information on the development of radiographically confirmed LM. Patients from whom LM-high-forming PDXs were established were more likely to have or develop LM than patients from whom LM-low-forming PDXs were established (Pearson’s Chi-Square 4.2236, P = .04). LM-high-forming PDXs are defined as those models that develop of an average equal to or greater than 4 distinct spinal cord LM lesions with a cancer cell area of >250 00 00 µm2 per mouse H&E-stained spinal cord analyzed. Abbreviations: HI, highly invasive; MI, minimally invasive; LM, leptomeningeal metastases; PDX, patient-derived xenografts.