To the Editor—We read with interest the article by Chow et al1 describing the outcomes of rostered routine testing (RRT) of healthcare workers (HCWs) in a tertiary-care hospital with robust infection prevention measures during an ongoing hospital outbreak of coronavirus disease 2019 (COVID-19). Despite the presence of a large hospital cluster, extensive RRT of asymptomatic HCWs did not detect covert infection.1 Given the low risk of healthcare-associated transmission on the background of robust infection prevention and the low incidence of asymptomatic severe acute respiratory coronavirus virus 2 (SARS-CoV-2) infection among HCWs,2 routine surveillance of asymptomatic HCWs is not recommended as a primary infection prevention strategy.3 Similarly, the value of systematic screening of all asymptomatic inpatients for SARS-CoV-2 has been questioned, given low detection rates.4 However, there may still be potential for spillover of infections into the healthcare system during ongoing community outbreaks of COVID-19. We describe our institution’s experience with RRT of HCWs and systematic screening of all inpatients for SARS-CoV-2 during a large COVID-19 outbreak in the immediately adjacent community.
In Singapore, a Southeast Asian city-state, healthcare-associated transmission of COVID-19 was initially limited due to comprehensive infection prevention measures instituted early in the pandemic.5–7 At our institution, the largest hospital campus in Singapore, with close to 13,000 HCWs, COVID-19 rates among HCWs have been kept low to date (17 of 13,066, 0.13%) and have reflected community acquisition rather than nosocomial spread.8 Over a 6-month period from January to June 2020, while ≥1,500 cases of COVID-19 were managed in our institution, <5% of cases were initially detected outside the isolation ward, mitigating potential nosocomial transmission.8,9 However, with the emergence of more highly transmissible variant strains, a large hospital cluster attributed to the B.1.617.2 variant strain was reported at the end of April 2021; providing the impetus for Singapore’s Ministry of Health to institute RRT for all HCWs in acute-care hospitals.1 Previously, SARS-CoV-2 testing was made available at our institution’s staff clinic to all symptomatic HCWs and high-risk asymptomatic healthcare contacts. RRT via polymerase-chain-reaction (PCR) testing of respiratory samples was conducted every 2 weeks for vaccinated staff and weekly for nonvaccinated staff. No additional covert infections were detected at our institution during the first round of RRT. COVID-19 vaccination uptake at our institution was high; 89.6% of staff had received 2 doses by the end of April 2021.
On June 10, 2021, an epidemiologically unlinked case of COVID-19 infection at a wet market <1 km from our hospital campus was first detected via community-based surveillance. This case turned out to be the index case of a large community cluster linked to ongoing transmission in the Bukit Merah housing estate surrounding our hospital campus. Over a 6-week period from June 10, 2021, to July 23, 2021, 132 cases in 5 community clusters were detected from community surveillance conducted in the Bukit Merah housing estate (Fig. 1a and b).9 Given the close proximity of this community outbreak to our hospital campus, spillover of undetected infection was an immediate concern. Of 13,066 staff 1,350 (10.3%) stayed within a 1.5-km radius of the cluster epicenter (Fig. 1a) and the community clusters fell within our hospital’s catchment area, meaning that patients in these neighborhoods with heightened community transmission would be conveyed to our hospital if they required acute medical care. In addition to staff RRT, from June 19, 2021, onward, universal screening of all inpatients was instituted, with patients tested for SARS-CoV-2 via PCR testing of respiratory samples, on admission and every 7 days subsequently.
Fig. 1.
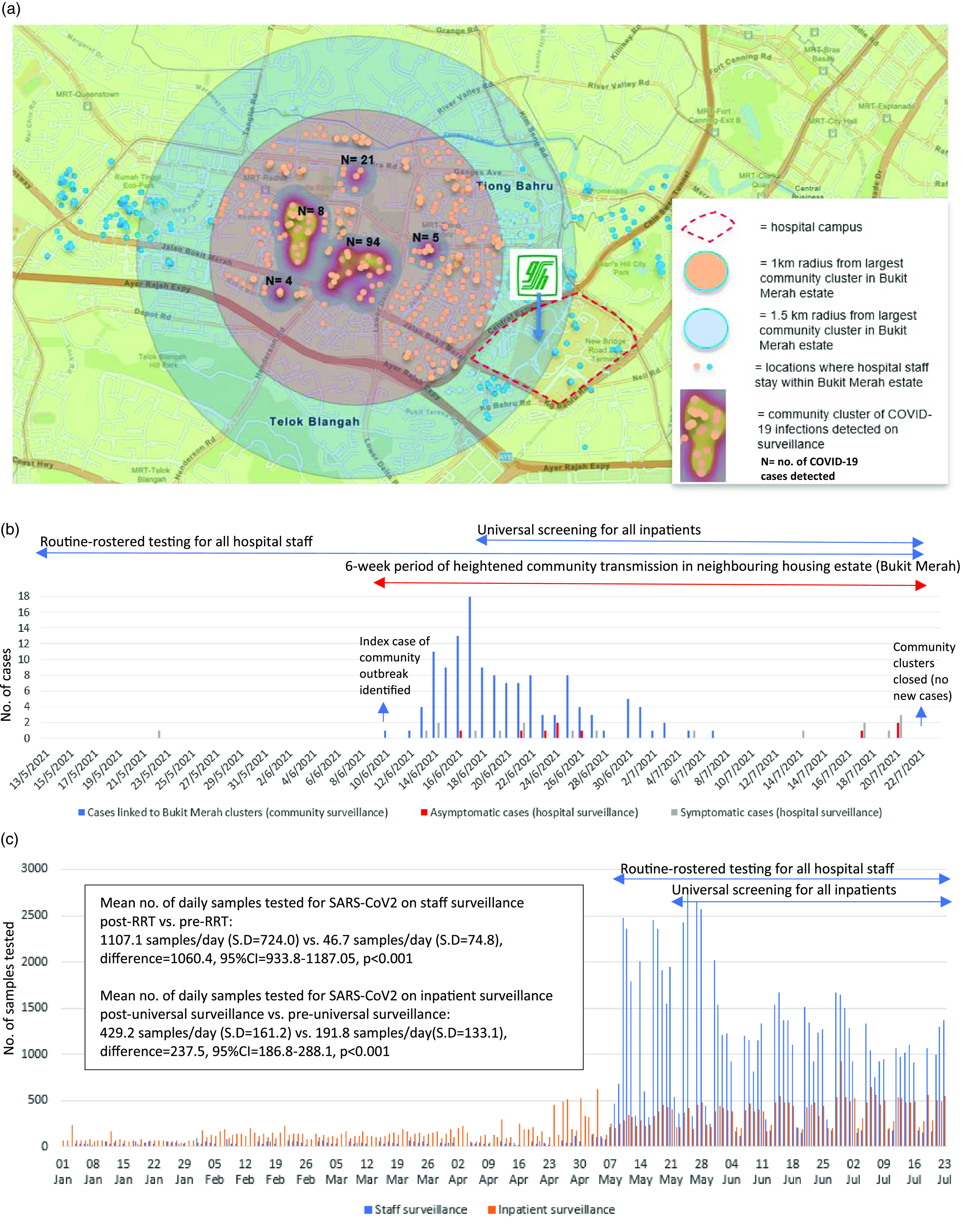
a: Map of community clusters in proximity to the hospital campus of a large Singaporean tertiary hospital. b: Timeline of COVID-19 outbreak in neighbouring community, and detection of COVID-19 cases amongst staff and patients through hospital surveillance. c: Volume of SARS-CoV-2 testing (PCR) for staff and patients at a large Singaporean tertiary hospital.
During the 6-week outbreak period, 7 HCWs and 20 inpatients at our institution tested positive for SARS-CoV-2. Among these 27 positive cases, 14 (51.8%) were linked epidemiologically to the Bukit Merah community clusters and were attributed to the B.1.617.2 variant. Most cases identified by hospital surveillance (4 of 7 HCWs, 11 of 20 inpatients) stayed within 1.5 km of the cluster epicenter; 4 (57%) of the 7 HCWs and 5 (25%) of the 20 inpatient cases were asymptomatic at time of diagnosis. Contact tracing for the 7 HCW cases identified 37 additional staff as having significant unprotected contact requiring quarantine; none subsequently tested positive. In comparison, prior to RRT, 14 cases of COVID-19 were detected among HCWs at our institution over a 4-month period (January–April 2020); 76 staff were identified as having significant unprotected contact, and a COVID-19 cluster was subsequently detected in HCWs sharing a common office space.5
Before institution of universal patient surveillance, patients detected outside the isolation ward over a 6-month period (January–June 2020) spent an average of 16.5 hours (N = 32; SD, 9.76) in the general ward prior to isolation, with 68 inpatient close contacts identified; 1 inpatient’s close contact subsequently tested positive within the incubation period.8,9 During the universal surveillance period, asymptomatic inpatients spent an average of 2 hours (N = 5; SD, 1.87) prior to isolation, a difference that was statistically significant (−14.6; 95% CI, −23.5 to −5.6; P = .002). In total, 26 inpatient close contacts were identified and placed under quarantine; none tested positive.
In conclusion, institution of RRT for all HCWs as well as universal screening for COVID-19 in all inpatients during a 6-week period of increased transmission in the surrounding community detected additional asymptomatic cases among HCWs and inpatients. Although the yield of testing was not high, earlier detection of asymptomatic inpatient cases allowed for faster isolation, limiting potential exposure. No clusters of COVID-19 infections were seeded among staff or patients during a period of heightened risk. Although RRT and universal screening for all inpatients is resource intensive (Fig. 1c), there may be a role for such measures during increased community transmission, given that healthcare institutions are inextricably intertwined with their neighboring communities.
Acknowledgments
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.
References
- 1.Chow A, Guo H, Kyaw WM, Li AL, Lim RHF, Ang B. Rostered routine testing for severe acute respiratory coronavirus virus 2 (SARS-CoV-2) infection among healthcare personnel–Is there a role in a tertiary-care hospital with enhanced infection prevention and control measures and robust sickness-surveillance systems? Infect Control Hosp Epidemiol 2021:1–2. [DOI] [PMC free article] [PubMed]
- 2.Roberts SC, Peaper DR, Thorne CD, et al. Mass severe acute respiratory coronavirus 2 (SARS-CoV-2) testing of asymptomatic healthcare personnel. Infect Control Hosp Epidemiol 2021;42:625–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shenoy ES, Weber DJ.Routine surveillance of asymptomatic healthcare personnel for severe acute respiratory coronavirus virus 2 (SARS-CoV-2): not a prevention strategy. Infect Control Hosp Epidemiol 2021;42:592–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stadler RN, Maurer L, Aguilar-Bultet L, et al. Systematic screening on admission for SARS-CoV-2 to detect asymptomatic infections. Antimicrob Resist Infect Control 2021;10:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wee LE, Sim XYJ, Conceicao EP, et al. Containment of COVID-19 cases among healthcare workers: the role of surveillance, early detection, and outbreak management. Infect Control Hosp Epidemiol 2020;41:765–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wee LE, Hsieh JYC, Phua GC, et al. Respiratory surveillance wards as a strategy to reduce nosocomial transmission of COVID-19 through early detection: the experience of a tertiary-care hospital in Singapore. Infect Control Hosp Epidemiol 2020;41:820–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Htun HL, Lim DW, Kyaw WM, et al. Responding to the COVID-19 outbreak in Singapore: staff protection and staff temperature and sickness surveillance systems. Clin Infect Dis 2020;71:1947–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wee LE, Venkatachalam I, Sim XYJ, et al. Containment of COVID-19 and reduction in healthcare-associated respiratory viral infections through a multi-tiered infection control strategy. Infect Dis Health 2021;26:123–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wee LEI, Sim XYJ, Conceicao EP, et al. Containing COVID-19 outside the isolation ward: the impact of an infection control bundle on environmental contamination and transmission in a cohorted general ward. Am J Infect Control 2020;48:1056–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Community Surveillance Testing at Bukit Merah View. 2021. Singapore Ministry of Health website. https://www.moh.gov.sg/news-highlights/details/community-surveillance-testing-at-bukit-merah-view_19Jun2021. Accessed July 25, 2021.


