Abstract
Purpose
Conventional CT technology yields only modest accuracy of coronary artery stenosis assessment in severely calcified lesions. Reported herein are this study's initial observations on the potential of ultra-high-resolution CT (UHR-CT) for evaluating severely calcified coronary arterial lesions.
Materials and Methods
Fifteen patients 45 years of age or older, with history of coronary artery disease, referred for invasive coronary angiography, were prospectively enrolled. Patients underwent UHR-CT within 30 days prior to cardiac catheterization. Image noise levels and diagnostic confidence (level 1–5) using UHR-CT were compared with reconstructed images simulating conventional CT technology. Stenosis assessment for the major coronary arteries and the left main coronary artery with UHR-CT and invasive angiography were compared. Results from clinically driven coronary CT using conventional technology were considered for comparison when available.
Results
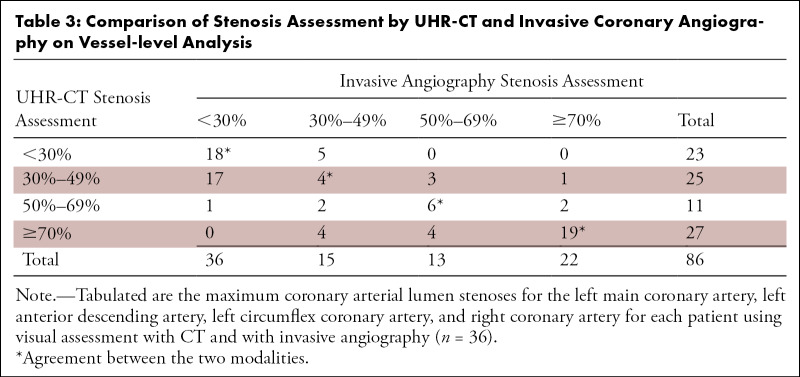
Mean patient age was 67 years (range, 53–79 years). Thirteen patients were men, nine had obesity. Radiation dose was 9.3 mSv owing to expanded x-ray exposure to accommodate research software application (70%–99% of R-R cycle). Overall image noise was considerably greater for UHR-CT (50.9 ± 7.8 [standard deviation]) versus conventional CT image reconstruction (19.5 ± 8.3, P < .01), yet diagnostic confidence scores for UHR-CT were high (4.3 ± 0.9). Average calcium score in patients without stents (n = 6) was 1205, and of 86 vessels evaluated, 22 had 70% or greater stenosis depicted with invasive angiography (26%). Stenosis comparison with invasive angiography yielded 86% (19 of 22) sensitivity and 88% (56 of 64) specificity (95% CI: 65%, 97%; and 77%, 95%, respectively).
Conclusion
Initial observations suggest UHR-CT may be effective in overcoming the limitation of conventional CT for accurately evaluating coronary artery stenoses in severely calcified vessels.
Keywords: CT-Angiography, Coronary Arteries, Arteriosclerosis
Clinical trial registration no. NCT04272060
See also commentary by Shanbhag and Chen in this issue.
© RSNA, 2021
Keywords: CT-Angiography, Coronary Arteries, Arteriosclerosis
Summary
This study's initial experience with coronary angiography using ultra-high-resolution CT in patients suspected of having coronary stenoses demonstrates promise for high diagnostic accuracy even in the setting of severe coronary calcification or prior stenting, representing a potentially substantial advance compared with conventional CT technology in this challenging patient population.
Key Points
■ Ultra-high-resolution CT (UHR-CT) is associated with greater image noise compared with conventional CT.
■ UHR-CT yields good diagnostic confidence in severely calcified coronary atherosclerotic disease.
■ UHR-CT may overcome the limitation of conventional CT for evaluating stenosis severity in severely calcified arteries.
Introduction
Coronary CT angiography (CTA) is evolving into an effective first-line imaging test in patients suspected of having coronary heart disease (CHD) (1–3). A remaining limitation, however, is CTA's reduced accuracy in detecting obstructive CHD in the setting of severe coronary artery calcification or coronary stenting (4–6). This limitation may be overcome with improved spatial resolution, which reduces the partial volume effect from high attenuation structures, such as calcium and metal (6–8). Ultra-high-resolution CT (UHR-CT) is now commercially available with 0.25-mm effective slice thickness, associated with 46-lp/cm resolution (9). Preliminary data in patients with coronary stents suggest potential utility of UHR-CT for improved stent analysis compared with conventional CT (7). No data are available on the potential value of UHR-CT in patients with severe coronary artery calcification. We are reporting our initial observations with UHR-CT in patients suspected of having severe CHD and high coronary calcium scores.
Materials and Methods
Patient Population
This is a prospective, single-center diagnostic accuracy study that was approved by our local institutional review board in Baltimore at Johns Hopkins University. The study was registered at ClinicalTrials.gov, with the registration number NCT04272060, where the study protocol can be accessed. This investigation was supported by a research grant from Canon Medical Systems. The sponsor had no influence on study design, execution, or interpretation. The authors had exclusive control of the data and information provided in this article.
Consecutive patients were enrolled between November 2019 and May 2020 (halted March until November 2020 because of the COVID-19 pandemic). Written informed consent was obtained from all participants, as approved by the institutional review board of Johns Hopkins University. Health Insurance Portability and Accountability Act compliance was observed throughout the study duration. Participants were eligible for recruitment if they were 45 to 85 years of age, referred to the Johns Hopkins Hospital for invasive angiography with suspicion of obstructive CHD, and had at least one of the following: (a) severe CHD (≥ 50% stenosis) at prior coronary CTA or invasive coronary angiography, (b) previous coronary stent placement, or (c) a markedly elevated coronary calcium score (> 400). Coronary CTA was performed at least 48 hours but not more than 30 days prior to invasive coronary angiography. Exclusion criteria included prior cardiac surgery, acute coronary syndrome, chronic kidney disease with estimated glomerular filtration rate less than 60 mL/min, moderate or severe aortic stenosis, New York Heart Association class III or IV heart failure, allergy to iodinated contrast media, prior organ transplantation, permanent atrial fibrillation, or known advanced atrioventricular block without a pacemaker. Images acquired in participants with conventional CTA within 30 days prior to enrollment were included for additional, qualitative comparison with UHR-CT.
Coronary CTA Scanning Protocol
Sinus rhythm was confirmed by electrocardiogram prior to CTA. If the presenting heart rate was greater than or equal to 60 beats per minute, 50 mg of metoprolol and 15 mg of ivabradine were administered. Sublingual nitroglycerin (0.4–0.8 mg) was administered unless systolic blood pressure was less than 100 mm Hg. All CT scanning for the primary analysis was performed using UHR-CT (Aquilion Precision; Canon Medical Systems). In the absence of a history of coronary stenting, a calcium score was obtained using standard 120-kV acquisition and 3-mm slice thickness. For coronary CTA, helical scans were acquired with prospectively electrocardiographically triggered exposure from 70% to 99% of the R-R interval, with 120-kV tube voltage and weight-adapted tube current, 0.35-second gantry rotation, and 160 × 0.25 mm collimation. A widened exposure window was chosen to allow the possibility of executing advanced image analysis, for example, blood flow estimations, which, however, occurred at the burden of increased radiation dose. Contrast medium containing 350 mg/mL of iodine (Omnipaque 350; GE Healthcare) was administered using a triphasic injection protocol (contrast medium followed by a 30/70 split of contrast medium and saline, followed by a saline flush), with injection rates of 5–7 mL/sec and computer-assisted bolus tracking, for a total of 80–100 mL (mean, 97 mL) of contrast medium. Dose-length product (DLP) was recorded for each participant. To estimate effective radiation dose, we used the recommended formula by the International Commission of Radiological Protection of multiplying the DLP with a k factor of 0.014 (10). We recognize that there is conceptual evidence to increase the k factor for cardiac CT, but a consensus paper by major societies on its value has not been published (11).
CTA Image Reconstruction and Interpretation
CT images were reconstructed using a vendor-specific algorithm (AIDR-3D) with a sharp kernel (FC05) and transmitted to a designated workstation (Vitrea; Vital Images) for viewing using a 1024 × 1024 matrix. Slice increment for imaging reconstruction was 0.125 mm. Nine studies were available for comparison of UHR-CT to conventional CT image characteristics. For this purpose, raw image data were sent to the vendor for image reconstruction using conventional CT technology (0.5-mm slice thickness with 0.25-mm overlap, 512 × 512 matrix) but otherwise identical reconstruction parameters, including convolution kernel, field of view, and iterative reconstruction settings. UHR-CT images were evaluated by a level III certified expert reader with 15 years of reading experience (A.A.Z.) blinded to invasive angiography results. A second reader (S.P.W.) provided blinded assessment for reader agreement evaluation. CT calcium scoring was performed using the Agatston method (12). For coronary CTA, the left main coronary artery and the three major coronary arteries were visually graded for stenoses categorized as minimal (1%–29%), mild (30%–49%), moderate (50%–69%), or severe (≥ 70%). They were further characterized in a binary fashion as severe or nonsevere, with severe stenosis defined as 70% or greater. Image noise, perivascular fat signal, and contrast opacification were analyzed in the ascending aorta for the overall study image quality and also in the most proximal calcium-free region of the three coronary arteries using 20-mm2 or larger regions of interest. Signal-to-noise ratio (SNR) was calculated as signal (in Hounsfield units)/noise (in Hounsfield units). Contrast-to-noise ratio (CNR) was calculated as (mean vessel lumen signal – mean perivascular fat signal [in Hounsfield units])/vessel-specific noise (in Hounsfield units). Image quality was graded on a scale of 1–5, with 5 defined as excellent image quality with minimal artifact, not affecting diagnosis; 4—mild artifact but diagnostic confidence maintained; 3—moderate artifact with little diagnostic doubt; 2—substantial artifact with diagnostic uncertainty, correlative imaging essential; 1—study uninterpretable owing to artifact. Any artifact limiting interpretability resulted in a lower score. Similarly, a diagnostic confidence level was graded from 1 to 5, with 5 indicating high confidence.
Data from conventional coronary CTA were used for qualitative comparison if these were performed for clinical purposes within 30 days of study enrollment.
Invasive Coronary Angiography Protocol and Analysis
Cardiac catheterization and invasive coronary angiography were performed according to the local clinical protocol. Intracoronary nitroglycerin was administered routinely prior to imaging. Results on coronary stenosis assessment were obtained from the clinical reports and used for comparison with UHR-CT. All readers were blinded to the results from UHR-CT.
Statistical Analysis
All statistical analyses were performed using Stata, version 15.1. Mean and standard deviation are presented for continuous data, and frequency and percent are presented for categorical data. The primary analysis performed was diagnostic accuracy using test sensitivity and specificity, defined as the ratios of true-positive results to the sum of true-positive and false-negative results and true-negative results to the sum of true-negative and false-positive results, respectively. Diagnostic accuracy was assessed on a vessel-level analysis. The highest-grade segmental stenosis represented the vessel-level stenosis. Vessels were defined as the left main coronary artery, left anterior descending artery, left circumflex coronary artery, and right coronary artery (10). SNRs and CNRs of the UHR-CT and conventional-resolution CT were compared via paired t testing. Agreement among readers for angiographic stenosis assessment was evaluated using Cohen κ testing.
Results
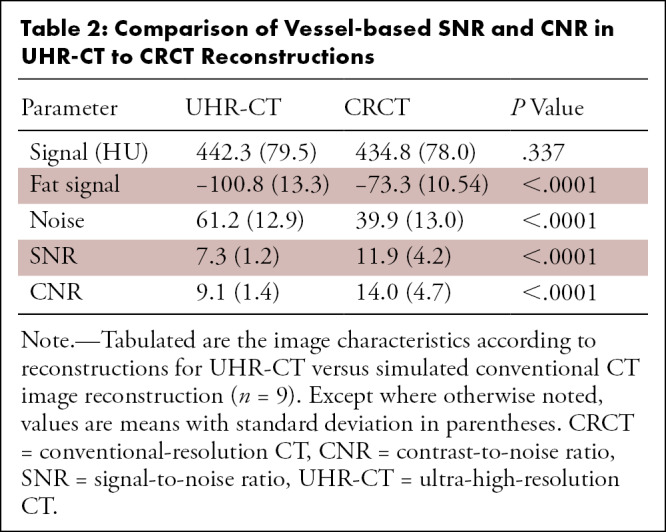
Fifteen participants were enrolled between November of 2019 and May of 2021, with an 8-month interruption due to the COVID-19 pandemic. Table 1 lists the characteristics of our study population. The patients enrolled were primarily men (13 of 15) with a mean age of 67 years ± 7. Average patient weight was 91.3 kg (range, 50–120 kg), and seven patients had obesity as defined by a body mass index of 30 kg/m2 or higher. Eight patients had prior stent placement (total of 20 stents). In patients without stents, the mean calcium score was 1205 (range, 249–2780). All UHR-CT studies were acquired using prospective scan triggering using a 70%–99% exposure window, except for in one participant who had a premature ectopic beat during image acquisition that resulted in mode switch to full R-R imaging for part of the scan. All studies were deemed interpretable, though the calcium score for the one patient with ectopic beats during image acquisition could not be completed. The overall image quality of coronary UHR-CT angiography was very good, with an average score of 4.1 ± 0.8 (range, 3–5) despite relatively low CNR and high image noise (Table 2). Diagnostic confidence score ranged between 3 and 5, with an average score of 4.3 ± 0.9. Interreader agreement was 83.8% for detecting 70% or greater stenoses on a vessel-level assessment (κ = 0.59, P < .0001). There were significantly higher noise levels in UHR-CT as compared with conventional-resolution CT and, consequently, lower SNR and CNR (Table 2). Interreader reliability for vessel-based signal intensity measurement was available for nine studies, yielding an intraclass correlation coefficient of 0.875 (95% CI: 0.74, 0.94).
Table 1:
Patient Characteristics
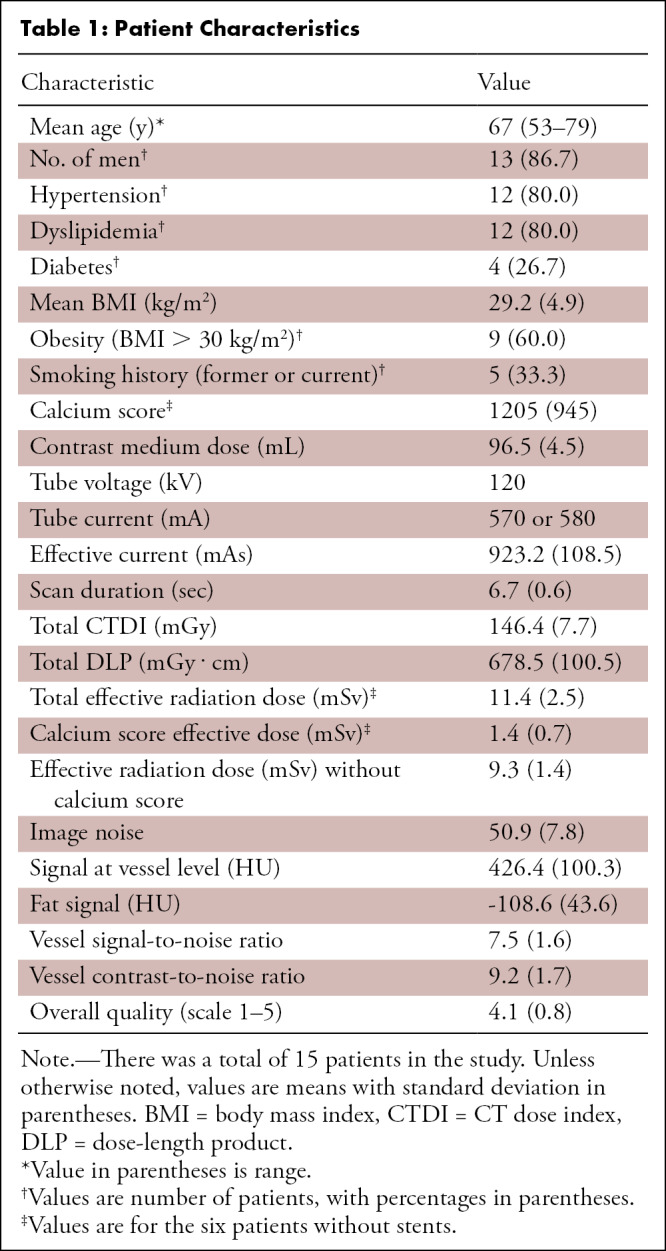
Table 2:
Comparison of Vessel-based SNR and CNR in UHR-CT to CRCT Reconstructions
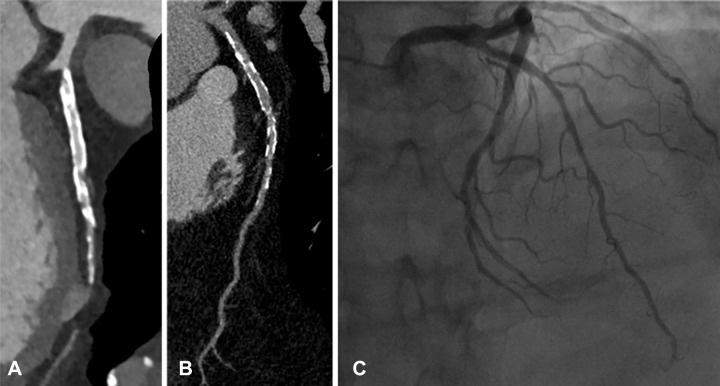
All patients were successfully examined with UHR-CT for the presence or absence of obstructive CHD. Adverse events were not noted for UHR-CT or invasive angiography. Of a total of 86 analyzed vessel segments, 22 were found to have 70% or greater stenosis with cardiac catheterization versus 27 with UHR-CT. Sensitivity and specificity for UHR-CT versus invasive angiography were 86% (19 of 22) and 88% (56 of 64), respectively (95% CI: 65%, 97% and 77%, 95%, respectively) (Table 3). Case examples are shown in Figures 1 and 2. Two patients underwent conventional coronary CTA prior to UHR-CT and invasive angiography. While conventional angiography incorrectly reported severely obstructive coronary artery disease in case 1, UHR-CT correctly depicted the patient as having nonobstructive disease in the setting of a calcium score of 2780 (Fig 3). The second case yielded identical categorical stenosis assessment with UHR-CT and conventional CT (Fig 4).
Table 3:
Comparison of Stenosis Assessment by UHR-CT and Invasive Coronary Angiography on Vessel-level Analysis
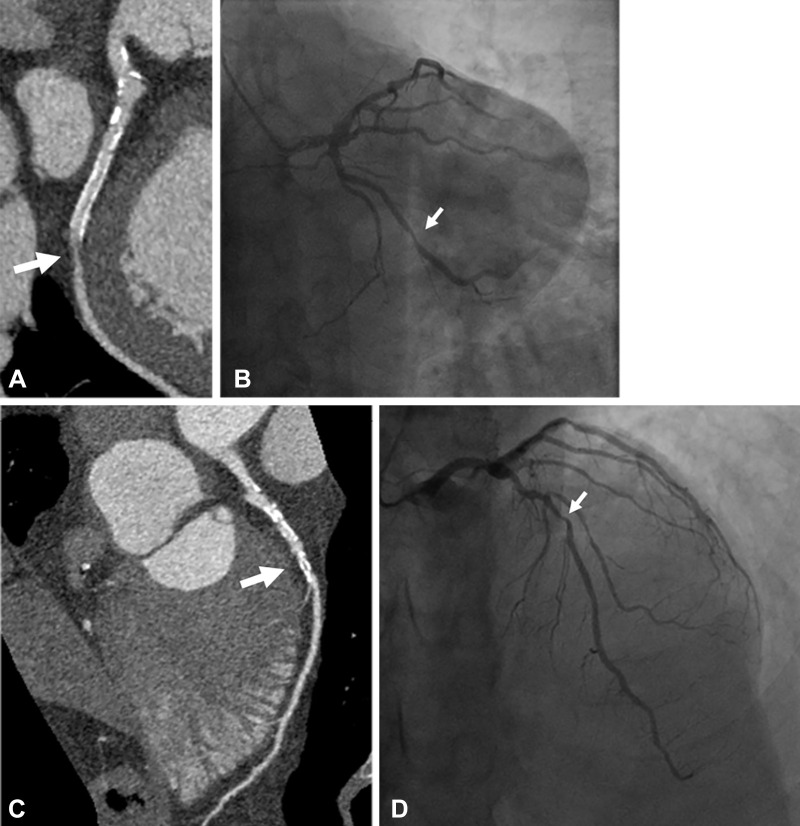
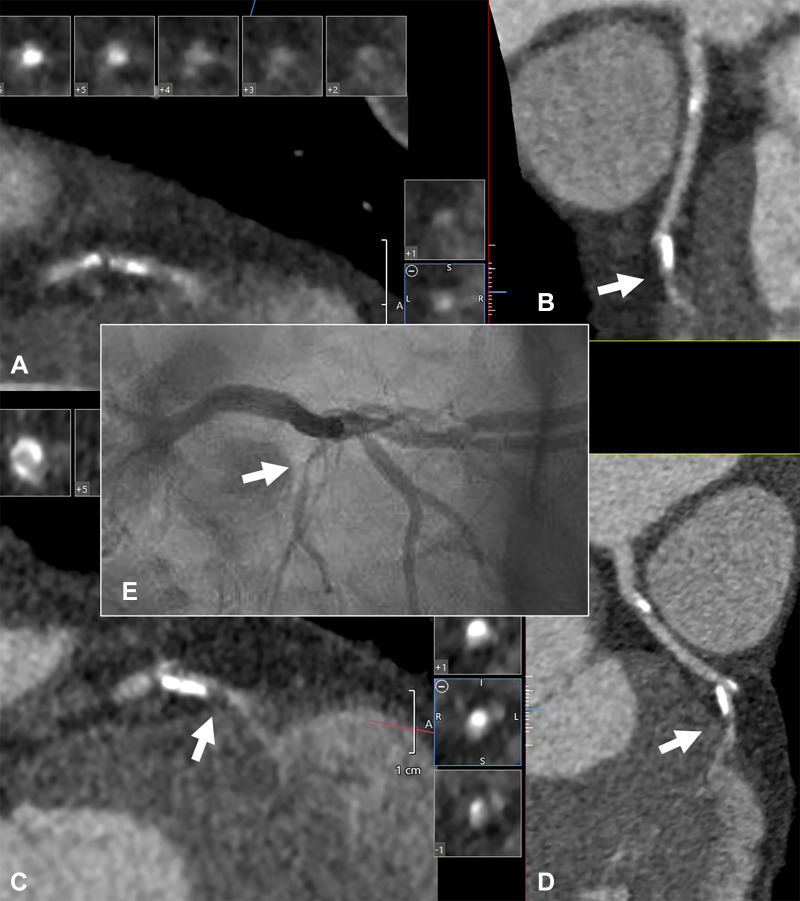
Figure 1:
Case example of a 61-year-old man with history of myocardial infarction who was found at UHR-CT to have a severe (≥ 70%) stenosis in a large obtuse marginal branch of the left circumflex artery just distal to (A) a patent stent, which was confirmed at (B) invasive angiography. In addition, there was moderate disease noted by (C) ultra-high-resolution CT in the left main and in the mid left anterior descending artery (50%–70% stenosis), which was underestimated compared with (D) invasive angiography (70% stenosis). Arrow points to corresponding stenoses.
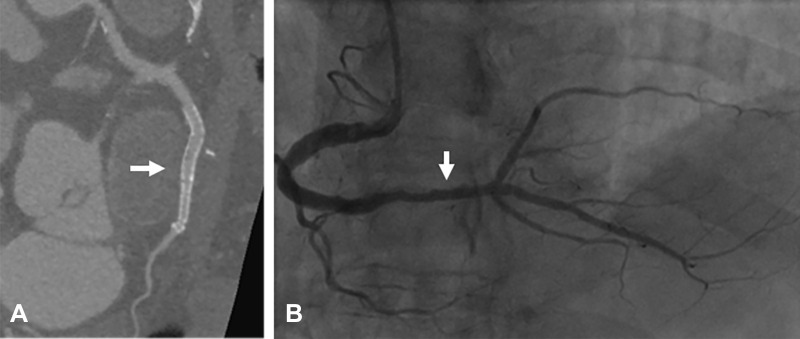
Figure 2:
Case example of a 62-year-old man complaining of chest pain who was found to have patent stents in his mid and distal right coronary artery at ultra-high-resolution CT (UHR-CT), displayed in (A) curved multiplanar view, which was confirmed with (B) invasive coronary angiography. Arrow points to the corresponding parts in the vessel by UHR-CT and invasive angiography.
Figure 3:
Case example of a 52-year-old man with history of hypertension, familial hyperlipidemia, and a normal nuclear stress test but with a calcium score of 2780. The patient initially underwent conventional CT angiography (CTA) for further assessment. Images were acquired with a dual-source (2 × 128 section) system, 285-msec gantry rotation, 110 kV, 371 mA. Images were reconstructed using 0.75-mm slice thickness and kernel Bv38f\3. (A) Curved planar reformatted projection of the left anterior descending artery (LAD) with conventional CTA along with cross-sectional views. With conventional CT, the LAD was reported to contain 70%–99% stenoses in proximal and mid section and a greater than 95% stenosis in the distal vessel. In contrast, (B) results from blinded ultra-high-resolution CT evaluation suggested heavily calcified LAD and lumen without obstructive disease, which was confirmed with (C) invasive angiography.
Figure 4:
Case example of a 62-year-old man with history of hypertension, severe obesity, hyperlipidemia, and atrial fibrillation presenting with progressive, exertional chest discomfort. He initially underwent coronary angiography using conventional CT technology (320-detector scanner with 0.5-mm detector width, 0.275-msec gantry rotation). His heart rate was less than 50 beats per minute at the time of image acquisition, and tube settings were 120 kV and 740 mA (maximum). (A) Corresponding images of the mid left anterior descending artery are shown using a sharp reconstruction filter (FC05). Note the poorly differentiated lumen borders (arrow) leading to uncertainty about the stenosis severity in the corresponding (B) curved multiplanar reformatted projection. The patient then underwent ultra-high-resolution (UHR) CT within 1 week of the conventional CT using a gantry rotation of 350 msec, 120 kV, and 580 mA (maximum). Recorded heart rate was 61 beats per minute. Images were again reconstructed using a sharp reconstruction kernel (FC05). (C, D) UHR-CT images. Note the sharper lumen borders and clear identification of a severe stenosis (arrow). (E) Corresponding invasive angiogram obtained within 72 hours of the UHR-CT. The arrow points to the stenosis in the small mid distal left anterior descending artery system.
Discussion
Our initial experience with UHR-CT suggests high diagnostic confidence in patients with severely calcified coronary artery disease, a setting which typically is associated with poor diagnostic accuracy with conventional CTA. In the multicenter Coronary Evaluation Using Multidetector Spiral Computed Tomography Angiography Using 64 Detectors CT (CORE-64) study, a calcium score of 600 or higher, or the presence of stents, was associated with 56% and 57% test specificity, respectively, for detecting significant stenoses versus 91% in patients without stents or severe calcification (5,6). Diagnostic accuracy did not improve in this setting with most recent technology (4). Our preliminary data suggest UHR-CT has the potential to improve diagnostic accuracy in this challenging and important patient population.
Coronary CTA has become a first-line test for the evaluation of patients suspected of having CHD (3,13). However, the test is currently considered inappropriate in the setting of severe coronary calcification because of an unacceptable associated decrease in diagnostic accuracy (14). Overcoming this limitation would mark a substantial advance for this technology with potentially extended impact. On the basis of CORE-64 data, at least one-third of patients referred for invasive coronary angiography have severe coronary calcification or prior stent placement and thus would benefit from UHR-CT (6). Three participants with very severely elevated calcium scores in our study would not have needed to undergo invasive coronary angiography after identifying only nonobstructive disease at UHR-CT. Furthermore, given the results from the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches trial, the indication of coronary CTA may expand to patients with high pretest probability of obstructive coronary artery disease (and associated calcification or stents) for excluding high-risk coronary anatomy, for example, substantial left main disease, to confirm eligibility for conservative medical management (15).
CT image quality and interpretability are affected by numerous factors, including detector characteristics, acquisition time, and reconstruction parameters. As expected with decreased detector width, image noise was greater than typically encountered with conventional CT. Still, diagnostic quality and interpretability were not only maintained but possibly even enhanced, presumably due to reduced “blooming” artifact from calcification and stents. Further investigations may elucidate how individual factors may contribute to diagnostic accuracy. We were not yet able to take advantage of the system's advanced deep learning image reconstruction algorithm using artificial intelligence, which is expected to further improve image quality (13,16). We acquired images using a longer exposure window (70%–99% R-R interval) than usually applied in clinical practice (70%–80% R-R interval) to accommodate advanced research software application, which increased radiation dose by approximately 30%.
The halt in enrollment of patients due to the COVID-19 pandemic limited our study population, and our results therefore are preliminary. Other limitations include a single-center experience and lack of dedicated core laboratory assessment. Furthermore, our data on conventional image reconstruction represent a simulation of images obtained with conventional CT technology. Such simulation, however, cannot fully account for the complex process of image acquisition among two different detector and scan configurations. Last, our analysis did not include advanced noise reduction algorithms to allow reduced radiation doses compared with our acquisition settings.
UHR-CT appears promising for accurately defining the coronary anatomy in the setting of severe coronary calcification and stents. These preliminary results indicate UHR-CT may overcome an important limitation of conventional-resolution CT in this challenging and important patient population.
Supported by a research grant from Canon Medical Systems. The sponsor had no influence on study design, execution, or interpretation.
Disclosures of Conflicts of Interest: J.L. disclosed no relevant relationships. M.S. Activities related to the present article: disclosed grant to author's institution from Canon, the provider of the CT device. Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships. K.K. disclosed no relevant relationships. S.P.W. disclosed no relevant relationships. J.C.T. disclosed no relevant relationships. J.S. disclosed no relevant relationships. S.D. disclosed no relevant relationships. M.M. disclosed no relevant relationships. J.A.C.L. Activities related to the present article: disclosed grant support to author's institution from Canon Medical Systems, formerly named Toshiba Medical Systems. Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships. A.A.Z. Activities related to the present article: disclosed research grant to author's institution from Canon Medical Systems. Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships.
Abbreviations:
- CHD
- coronary heart disease
- CNR
- contrast-to-noise ratio
- CORE-64
- Coronary Evaluation Using Multidetector Spiral Computed Tomography Angiography Using 64 Detectors CT
- CTA
- CT angiography
- DLP
- dose-length product
- SNR
- signal-to-noise ratio
- UHR-CT
- ultra-high-resolution CT
References
- 1.SCOT-HEART investigators , Newby DE, Adamson PD, et al. Coronary CT and 5-year risk of myocardial infarction. N Engl J Med 2018;379:924–933. [DOI] [PubMed] [Google Scholar]
- 2. Timmis A , Roobottom CA . National Institute for Health and Care Excellence updates the stable chest pain guideline with radical changes to the diagnostic paradigm . Heart 2017. ; 103 : 982 – 986 . [DOI] [PubMed] [Google Scholar]
- 3. Knuuti J , Wijns W , Saraste A , et al . 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes . Eur Heart J 2019. ; pii : ehz425 . [DOI] [PubMed] [Google Scholar]
- 4. Song YB , Arbab-Zadeh A , Matheson MB , et al . Contemporary discrepancies of stenosis assessment by computed tomography and invasive coronary angiography . Circ Cardiovasc Imaging 2019. ; 12 ( 2 ): e007720 . [DOI] [PubMed] [Google Scholar]
- 5. Wykrzykowska JJ , Arbab-Zadeh A , Godoy G , et al . Assessment of in-stent restenosis using 64-MDCT: analysis of the CORE-64 Multicenter International Trial . AJR Am J Roentgenol 2010. ; 194 ( 1 ): 85 – 92 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arbab-Zadeh A , Miller JM , Rochitte CE , et al . Diagnostic accuracy of computed tomography coronary angiography according to pre-test probability of coronary artery disease and severity of coronary arterial calcification. The CORE-64 (Coronary Artery Evaluation Using 64-Row Multidetector Computed Tomography Angiography) International Multicenter Study . J Am Coll Cardiol 2012. ; 59 ( 4 ): 379 – 387 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Motoyama S , Ito H , Sarai M , et al . Ultra-high-resolution computed tomography angiography for assessment of coronary artery stenosis . Circ J 2018. ; 82 ( 7 ): 1844 – 1851 . [DOI] [PubMed] [Google Scholar]
- 8. Takagi H , Tanaka R , Nagata K , et al . Diagnostic performance of coronary CT angiography with ultra-high-resolution CT: Comparison with invasive coronary angiography . Eur J Radiol 2018. ; 101 : 30 – 37 . [DOI] [PubMed] [Google Scholar]
- 9. Oostveen LJ , Boedeker KL , Brink M , Prokop M , de Lange F , Sechopoulos I . Physical evaluation of an ultra-high-resolution CT scanner [ published correction appears in Eur Radiol . 2020. March 25 ]. Eur Radiol . 2020. ; 30 ( 5 ): 2552 – 2560 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The 2007 Recommendations of the International Commission on Radiological Protection . ICRP publication 103. Ann ICRP 2007. ; 37 ( 2–4 ): 1 – 332 . [DOI] [PubMed] [Google Scholar]
- 11. Trattner S , Halliburton S , Thompson CM , et al . Cardiac-specific conversion factors to estimate radiation effective dose from dose-length product in computed tomography . JACC Cardiovasc Imaging 2018. ; 11 ( 1 ): 64 – 74 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Agatston AS , Janowitz WR , Hildner FJ , Zusmer NR , Viamonte M Jr , Detrano R . Quantification of coronary artery calcium using ultrafast computed tomography . J Am Coll Cardiol 1990. ; 15 ( 4 ): 827 – 832 . [DOI] [PubMed] [Google Scholar]
- 13. Ferraro R , Latina JM , Alfaddagh A , et al . Evaluation and Management of Patients With Stable Angina: Beyond the Ischemia Paradigm: JACC State-of-the-Art Review . J Am Coll Cardiol 2020. ; 76 ( 19 ): 2252 – 2266 . [DOI] [PubMed] [Google Scholar]
- 14. Taylor AJ , Cerqueira M , Hodgson JM , et al . ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance . J Am Coll Cardiol 2010. ; 56 ( 22 ): 1864 – 1894 . [DOI] [PubMed] [Google Scholar]
- 15. Maron DJ , Hochman JS , Reynolds HR , et al . Initial invasive or conservative strategy for stable coronary disease . N Engl J Med 2020. ; 382 ( 15 ): 1395 – 1407 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Singh R , Digumarthy SR , Muse VV , et al . Image quality and lesion detection on deep learning reconstruction and iterative reconstruction of submillisievert chest and abdominal CT . AJR Am J Roentgenol . 2020. ; 214 ( 3 ): 566 – 573 . [DOI] [PubMed] [Google Scholar]