Abstract
To reveal the role of the postoperative choledochoscopy in treating the residual calculi in the caudate lobe (CL) of the liver.
We recruited 66 patients with T-tube/percutaneous transhepatic cholangioscopy tract who still had residual gallstones in the CL at least 6 weeks after the operation. Imaging examinations determined the gallstones’ locations in the patients, and all of them underwent the postoperative choledochoscopic examination through the T-tube/percutaneous transhepatic cholangioscopy tract for therapeutic intervention.
Among the 66 patients, the residual gallstones were mostly located in the Spiegel lobe (48/66, 72.7%), and the residual gallstones that located in the origin of the CL bile branches were successfully determined in the 57 patients (57/66, 86.4%), the remaining 9 patients were unclear because the proximal ducts were severely narrow or even atresia. The mean frequency of the postoperative choledochoscopy was 3.6 (range, 1–10) times. There were 9 patients with complications, and no mortality occurred. In the origin-proved 57 patients, 6 patients failed to remove the gallstones altogether, and the final residual gallstone clearance rate was 77.3% (51/66). There was no significant difference between the Spiegel lobe and the other parts of the CL in determining the bile duct's origins, gallstone clearance rate, and complications. However, the frequency of choledochoscopy in the other parts of the CL was more than in the Spiegel lobe.
The postoperative choledochoscopy, an essential method for treating the residual gallstones in the CL, commands high efficiency for calculi extraction and fewer complications. The main reasons for failing to remove the residual gallstones are that the bile duct's origins could not be determined, and the distal bile ducts are atretic in the CL.
Keywords: postoperative choledochoscopy, residual hepatolithiasis, the caudate lobe, T-tube drainage
1. Introduction
Hepatolithiasis is a kind of benign bile disease, and the incidence could be as high as 50%, which is more common in East Asian countries, such as China, South Korea, Japan, Philippines, Malaysia, and Indonesia.[1] Several etiologies for hepatolithiasis have been previously proposed, including genetic, dietary, and environmental factors.[2] The treatment of hepatolithiasis is still challenging and often combined with high recurrence and various complications, such as recurrent cholangitis, biliary strictures, liver abscess, hepatotrophy, liver cirrhosis, and cholangiocarcinoma.[3,4] Hepatolithiasis is characterized by gallstones situated in the intrahepatic bile ducts, including the right and left hepatic ducts. However, the CL involved is not uncommon.[5] The CL lies in the liver's particular location, deep and adjacent to major blood vessels, and this unique anatomical structure makes it difficult for the gallstones in the CL to diagnose or treat. The caudate lobectomy has been gradually increased in recent years, including the complete laparoscopic caudate lobe resection. However, most cases are tumors in the caudate lobe, and liver resections for hepatolithiasis involved the caudate lobe are rarely reported.[6–10] Due to the limitation of the hepatectomy, the complete clearance of the bile duct calculi is low, and the incidence of residual gallstones is still high.[1] Postoperative choledochoscopy has been reported to be a safe and effective method in treating intrahepatic bile duct stones.[11,12] There are no reports about postoperative choledochoscopy in the treatment of patients with residual hepatolithiasis involving the CL. In this study, we first investigated patients with residual gallstones in the CL who underwent choledochoscopic examination through the T-tube/ percutaneous transhepatic cholangioscopy (PTCs) tract for therapeutic intervention, and we further analyzed the safety and efficiency of this therapy.
2. Materials and methods
2.1. Patients
This study enrolled 66 patients with residual gallstones in the CL, which retained the T-tube /PTCs tract at least 6 weeks after the common bile duct exploration (CBDE) or PTCs, who were admitted to the Shandong Provincial Third Hospital, Shandong University, from January 2017 to June 2019. All of the patients underwent physical examinations and imaging tests. The participants were comprised of 66 patients with hepatolithiasis, including patients with previous biliary tract surgery (n = 41), patients with hepatic lobe atrophy (n = 14), and patients with liver cirrhosis or hypersplenism (n = 8). There were 25 men and 41 women, aged 33 to 89 (median, 62) years. Among the 66 cases, 30 patients underwent laparoscopic CBDE with T-tube drainage, including 7 patients combined with hepatic lobectomy. Furthermore, 30 patients underwent open CBDE with T-tube drainage, including 9 patients with hepatic lobectomy, 4 with cholangiojejunostomy, and 2 with splenectomy and paraesophagogastric devascularization. Besides, 6 patients underwent PTCs. Intraoperative choledochoscopy was performed in 46 of the 66 patients. The patients began to clamp the T-tube on the 10th day after surgery, and all patients recovered smoothly (Table 1). Informed consent for the study was obtained from all participants. The study was approved by the Institutional Ethics Review Board of Shandong Provincial Third Hospital on March 17, 2020 (document No.KYLL-2020027).
Table 1.
Features of patients with the residual gallstones in the caudate lobe.
| Features | Values |
| Male, n (%) | 25 (37.8) |
| Age, range (median, yrs) | 33–89 (62) |
| Comorbidity, n (%) | |
| Previous biliary tract surgery | 41 (62.1) |
| Hepatic lobe atrophy | 14 (21.2) |
| Liver cirrhosis with hypersplenism | 8 (12.1) |
| Surgical method, n (%) | |
| LCBDE-T∗ | 23 (34.8) |
| LCBDE-T with hepatic lobectomy | 7 (10.6) |
| OCBDE-T† | 15 (22.7) |
| OCBDE-T with hepatic lobectomy | 9 (13.6) |
| OCBDE-T with cholangiojejunostomy | 4 (6.1) |
| OCBDE-T with splenectomy and paraesophagogastric devascularization | 2 (3) |
| PTCs‡ | 6 (9.1) |
| Intraoperative cholangioscopy | 46 (69.7) |
Laparoscopic common bile duct explorations with T-tube drainage.
Open common bile duct explorations with T-tube drainage.
Percutaneous transhepatic cholangioscopy.
2.2. The location of the residual gallstones in the CL
Advanced imaging techniques including abdominal ultrasound, computed tomography (CT), and magnetic resonance cholangiopancreatography were conducted, and the locations of the residual gallstones in the CL were determined in all 66 patients.
2.3. Choledochoscope equipment
Endoscopic examinations were performed in patients at least 6 weeks after common duct exploration or PTCs. Percutaneous choledochoscopy examination of the biliary tree was performed using the Olympus cholangioscope (CHF-V, Olympus, Japan; ECN-1530, PENTAX, Tokyo, Japan), including the accessories, basket, standard balloon dilatation, and electrohydraulic lithotripsy, which could pass through the irrigating/instrument channel.
2.4. The residual gallstones extraction method
Endoscopic examination was performed in the patient in an awakened state and sterile condition. Before the examination, the T-tube or rubber catheter from the T-tube tract was removed. The endoscope with saline irrigation running was performed along the T-tube tract under direct vision, examined common bile duct and intrahepatic bile ducts, and deflected into the aimed biliary trees where the gallstones located according to the preoperative imaging examination. The giant stones were treated with electrohydraulic lithotripsy, which were then removed by the basket. When the check was completed, a rubber catheter (18 or 20F) was inserted in the T-tube tract to drain the biliary tree until a repeated choledochoscopy after 5 to 7 days. If no biliary duct examination was required, remove the rubber catheter.
2.5. Statistical analysis
The statistical analyses were carried out by the Statistical Package for Social Science for Windows (SPSS, version 22.0, IBM, Chicago, IL). The Chi-squared test, Fisher exact test, t test were used as appropriate, and P < .05 was considered statistically significant.
3. Results
3.1. Locations of the residual gallstones
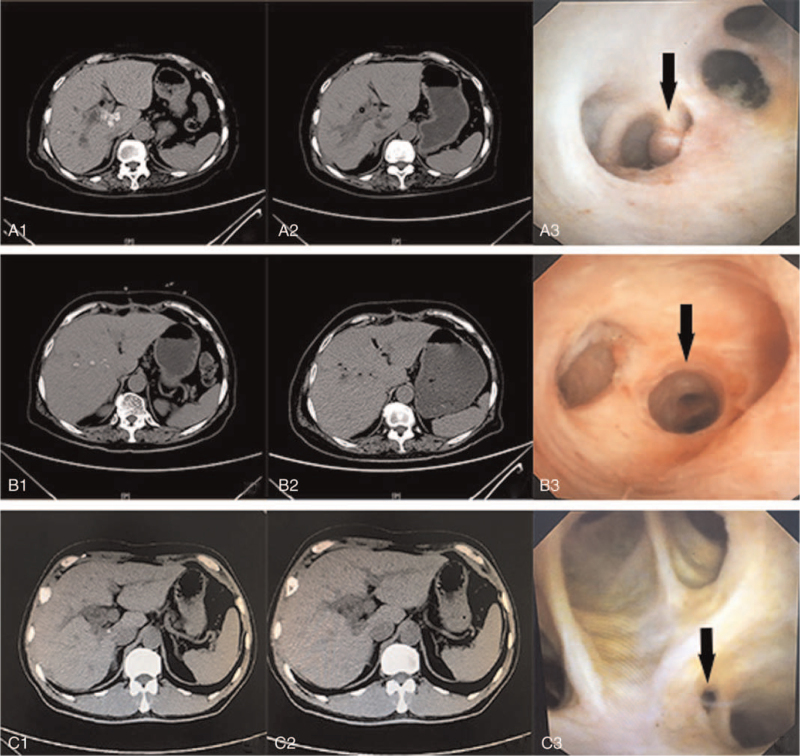
Among the 66 patients, 48 patients (72.7%) had residual gallstones in the Spiegel lobe; 18 patients (27.3%) had residual gallstones in the remaining parts, including 4 patients in the paracaval portion, 7 patients in the caudate process, 5 patients in the Spiegel lobe and paracaval portion, and 2 patients in the Spiegel lobe and caudate process. There was no simple caudate calculus in this group, and all of them combined with multiple intrahepatic stones (Fig. 1).
Figure 1.
The detection of gallstones using CT or choledochoscope. A1, the gallstones in the Spiegel lobe; A2, the gallstones were removed by the choledochoscope; A3, the black arrow was the origin of Spiegel lobe branch; B1, the gallstones in the paracaval portion; B2, the gallstones were removed by the choledochoscope; B3, the black arrow was the confluence of Spiegel lobe and paracaval portion branch; C1, the gallstones in the caudate process; C2, the gallstones were removed by the choledochoscope; C3, the black arrow was the “comet tail sign”; CT = computed tomography.
3.2. Bile branch's origin of the CL involved
Among the 66 patients, the origin of the bile branches of the CL where the residual gallstones were located was successfully determined in the 57 patients (86.4%); the remaining 9 patients were unclear because the proximal ducts were severely narrow or even atresia. Among the 48 patients with the Spiegel lobe gallstones, the branches mainly drained into the left hepatic duct have 31 cases (31/48, 64.6%), and 6 cases (12.5%) could not be defined the origin. Besides, the bile duct's origins were identified in 15 of the 18 patients with the residual gallstones in the other parts of the CL, and 3 cases (16.7%) failed to define mainly involved the paracaval portion (Table 2).
Table 2.
The biliary duct drainage site of the caudate lobe.
| Location of the residual gallstones | |||||
| The drainage site | The Spiegel lobe | The paracaval portion | The caudate process | The Spiegel lobe and paracaval portion | The Spiegel lobe and caudate process |
| The left hepatic duct | 31 (64.6%) | – | – | 3 | – |
| The right hepatic duct | 5 (10.4%) | 1 | 1 | 1 | 1 |
| The convergence of the right and left hepatic duct | 3 (6.25%) | – | – | 1 | – |
| The right posterior hepatic duct | 3 (6.25%) | – | 6 | – | 1 |
| Unclear | 6 (12.5%) | 3 | – | – | – |
| Total (n = 66) | 48 (100%) | 4 | 7 | 5 | 2 |
3.3. Frequency of choledochoscopy, mortalities, complications, and clearance rate of residual gallstone
The mean frequency of choledochoscopy was 3.6 (range, 1–10) times, and no mortality occurred. There were 9 patients with complications, including 5 with fever, 3 with hemobilia, and 1 with hepatopostema, relieved after conservative medical therapy. In the origin-proved 57 patients, 6 patients failed to remove the gallstones altogether. Finally, the residual gallstone clearance rate in the CL was 77.3% (51/66). Between the Spiegel lobe and the other parts of the CL, there was no significant difference in determining the bile duct origins, gallstone clearance rate, and the complications, but a difference of frequency of choledochoscopy became statistically significant (P = .015) (Table 3).
Table 3.
Outcomes of the postoperative choledochoscopy in the patients.
| Outcomes | The Spiegel lobe | The other partsa | Overall | P |
| Location of the residual gallstones, n (%) | 48 (72.7) | 18 (27.3) | 66 | – |
| Frequency of choledochoscopy, median (range)∗ | 2.9 times(1–10) | 4.3 times (1–8) | 3.6 times (1–10) | .015 |
| The determined origin of the bile ducts, n (%)∗∗ | 42 (87.5) | 15 (83.3) | 57 (86.4) | .467 |
| Complete removal of the gallstones, n (%)∗∗ | 38 (79.2) | 13 (72.2) | 51 (77.3) | .549 |
| Complications, n (%)∗∗ | 6 (12.5)b | 3 (16.7)c | 9 (13.6) | .467 |
Including 4 patients in the paracaval portion, 7 patients in the caudate process, 5 patients in the Spiegel lobe and paracaval portion, and 2patients in the Spiegel lobe and caudate process.
Four patients had fever, and 2 patients had hemobilia.
One patient had fever, 1 patient had hemobilia, and 1 patient had hepatapostema.
t test, P < .05 have statistic significant.
Chi-squared test, Fisher test, P < .05 have statistical significance.
4. Discussion
The CL, located deep in the liver, is adjacent to the hepatic vein and the inferior vena cava. Kumon divided the caudate lobe into 3 parts: Spiegel lobe, caudate process, and paracaval portion. The 3 portions often have their independent branches, tortuous and slender, and sometimes form acute angles with the hilar bile ducts.[13] The factors mentioned above could result in the biliary drainage unsmoothed, inducing the formation of hepatolithiasis. The bile duct stone incidence in the caudate lobe was between 24% and 42.3%.[5] Hepatectomy is regarded as the best approach to treat hepatolithiasis because it can remove stones and expand the bile duct simultaneously.[1] Meanwhile, CBDE, endoscopic approaches, liver transplantation, chemical bile duct embolization, and a combination of these are effective methods for treating hepatolithiasis.[11,14–16] Due to the unique anatomical location, caudate lobe resection is technically challenging, especially for isolated caudactomy, because it is easy to damage the hilum and the inferior vena cava, which could potentially cause uncontrolled bleeding.[17] Herein, there was no simple caudate calculus, and all of them combined with multiple intrahepatic stones. Owing to these limitations, the incidence of residual hepatolithiasis in patients is still high.
Choledochoscopy plays a vital role in diagnosing and treating hepatopancreatobiliary diseases, involving removing the biliary system stones, biopsy or cytology for the diagnosis biliary tract malignancies, balloon dilatation of the biliary stricture, and stent implantation for bile duct tumor.[18] Meanwhile, postoperative choledochoscopy is an essential and effective method for residual hepatolithiasis.[11] The reported clearance rate of postoperative choledochoscopy for residual calculus in the intrahepatic duct ranges from 90% to 95.5%.[12,18,19]
Nonetheless, the caudate lobe is supplied by both the right and left biliary tract, and the confluence of the CL bile ducts is not constant. Kumon[13] reported that the mean of biliary branches was 3.8 (range, 2–6), and the biliary branches of the Spiegel lobe and the caudate process portion were ramified mainly from the left-side tract and the right-side tract, respectively. Takamatsu et al[20] reported that the mean number of the bile ducts in the CL was 2.68 per liver, and about 80% of the Spiegel lobe branches drained into the left hepatic duct system, and almost all of the caudate process branches (92.4%) drained into the right posterior hepatic duct. Besides, Edo et al[21] reported that over 60% of the Spiegel lobe branches joined into the left hepatic duct system. Therefore, confirmed the distribution and the origin of the target bile ducts by CT, MR, and choledochoscope examinations were the keys to remove the gallstones.
Meanwhile, the bile duct's repeated inflammation where the stone is located could contribute to inflammatory floc floating called “comet tail sign,” which frequently suggests the target bile duct.[11] Another obstacle to identifying the bile ducts’ origin is the acute angle between the hilar bile ducts and the CL's bile ducts. During the endoscopic examination, we should rotate the endoscope repeatedly and confirm the choledochoscope “looking back” to find the origin of the target bile ducts, especially those with “comet tail sign.”
Our study found the residual gallstones of the CL were mainly located in the Spiegel lobe (72.7%) by CT and MR examinations. Furthermore, we adopted the methods of “looking back” and “comet tail sign” to find the target bile ducts during the endoscopic examination. Finally, we successfully determined the origin of the CL's bile branches and found the residual gallstones in 57 patients (86.4%), and the remaining 9 patients were unclear because the proximal ducts were severely narrow or even atresia. In the origin-proved 57 patients, the branches involving the Spiegel lobe mainly drained into the left hepatic duct (64.6%) and involving the caudate process mainly into the right posterior hepatic duct. However, the origin of the branches involving the paracaval portion was most unclear. The paracaval portion branches were unconstant, drained into the right biliary tracts, left biliary tracts, and right posterior segment ducts at almost equal frequencies.[13,20] Due to the aforementioned reasons, it is difficult to confirm the duct's origin involving the paracaval portion under choledochoscope.
Choledochoscope should be adopted as far as possible to enter the target bile duct for lithotomy under direct vision to improve stone removal efficiency and stone removal rate, whereas the stricture and acute angle between the adjacent bile ducts could prevent the choledochoscope from entering this bile duct. Moreover, balloon dilatation was frequently used as a therapeutic modality for the stricture bile ducts.[11] For some bile ducts with acute angles, we should first position the basket at the duct's distal end, thereby placing the choledochoscope into the target bile duct under the basket's guidance. By the aforementioned methods, most patients could successfully enter the target bile ducts by the choledochoscope. For some bile ducts that are always inaccessible, repeated extraction of the stone by the basket could be an effective method. There were 51 patients whose gallstones were completely removed among the origin-proved 57 patients in this study through the above methods. Besides, gallstones were not removed in 6 patients due to the distal bile duct's atresia and blocked stones. Overall, the residual gallstone clearance rate in the CL was 77.3% (51/66).
It had been reported that the overall complications of cholangioscopy ranged from 18.28% to 32.73%.[18,22] Kong et al[12] reported that 986 patients with residual bile duct stones were performed with post-operative percutaneous choledochoscopy; 13 patients had complications, including perforated sinus, biliary peritonitis, sinus hypoplasia, bleeding, and intestinal fistular. Hemobilia and infection are the most common complications, occurring in about 8% of cases.[18] In our study, 9 patients had complications (13.6%), which were fever and hemobilia, and relieved after conservative medical therapy. No severe complications and mortalities occurred.
As previously mentioned, the residual gallstones of the CL mainly located in the Spiegel lobe, whereas there was no significant difference between the spiegel lobe and the other parts of the CL in determining the bile duct origins, gallstone clearance rate, and the complications, except the frequency of choledochoscopy. The frequency of choledochoscopy in the other parts of the CL was more than in the Spiegel lobe, mainly due to the more challenging to find the origins of the bile ducts and a wider distribution of stones in other parts of CL compared with the Spiegel lobe.
In nutshell, the postoperative choledochoscopy is a safe and effective method, by which the residual stones in the CL can be successfully removed and with mild or no complications; nevertheless, it remains a challenge to locate the bile ducts’ origin due to the atresia in some cases.
Author contributions
Conceptualization: Li Liang, Xuting Zhi.
Data curation: Li Liang, Donghai Zhuang.
Formal analysis: Li Liang, Donghai Zhuang.
Funding acquisition: Li Liang.
Investigation: Li Liang, Donghai Zhuang.
Methodology: Li Liang, Xianguang Feng.
Resources: Donghai Zhuang, Xianguang Feng, Xuting Zhi.
Software: Li Liang, Xianguang Feng.
Supervision: Kai Zhang, Xuting Zhi.
Visualization: Kai Zhang.
Writing – original draft: Li Liang.
Writing – review & editing: Xuting Zhi.
Footnotes
Abbreviations: CBDE = common bile duct exploration, CL = caudate lobe, CT = Computed Tomography, PTCs = percutaneous transhepatic cholangioscopy, SPSS = Statistic Package for Social Science.
How to cite this article: Liang L, Zhuang D, Feng X, Zhang K, Zhi X. The postoperative choledochoscopy in the management of the residual hepatolithiasis involving the caudate lobe: A retrospective study. Medicine. 2021;100:35(e26996).
This research was supported by Medical and health science and technology development Program of Shandong province (2019WS449).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Feng X, Zheng S, Xia F, et al. Classification and management of hepatolithiasis: a high-volume, single-center's experience. Intractable Rare Dis Res 2012;1:151–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Catena M, Aldrighetti L, Finazzi R, et al. Treatment of non-endemic hepatolithiasis in a Western country. The role of hepatic resection. Ann R Coll Surg Engl 2006;88:383–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Kim HJ, Kim JS, Joo MK, et al. Hepatolithiasis and intrahepatic cholangiocarcinoma: a review. World J Gastroenterol 2015;21:13418–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Park JS, Jeong S, Lee DH, et al. Risk factors for long-term outcomes after initial treatment in hepatolithiasis. J Korean Med Sci 2013;28:1627–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Sun YM, Zou YT, Zhao HL, Wang XH. Diagnosis and treatment of bile duct stones of caudate lobe. Chin J Pract Surg 2001;21:283–4. in Chinese. [Google Scholar]
- [6].Chaib E, Ribeiro MA, Jr, Souza YE, D’Albuquerque LA. Anterior hepatic transection for caudate lobectomy. Clinics (Sao Paulo) 2009;64:1121–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Jin B, Jiang Z, Hu S, et al. Surgical technique and clinical analysis of twelve cases of isolated laparoscopic resection of the hepatic caudate lobe. Biomed Res Int 2018;2018:5848309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ishii H, Ogino S, Ikemoto K, et al. Mesohepatectomy with total caudate lobectomy of the liver for hepatocellular carcinoma. World J Surg Oncol 2013;11:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ahanatha Pillai S, Sathyanesan J, Perumal S, et al. Isolated caudate lobe resection: technical challenges. Ann Gastroenterol 2013;26:150–5. [PMC free article] [PubMed] [Google Scholar]
- [10].Peng SY, Li JT, Mou YP, et al. Different approaches to caudate lobectomy with “curettage and aspiration” technique using a special instrument PMOD: a report of 76 cases. World J Gastroenterol 2003;9:2169–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Wen XD, Wang T, Huang Z, et al. Step-by-step strategy in the management of residual hepatolithiasis using post-operative cholangioscopy. Therap Adv Gastroenterol 2017;10:853–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kong J, Wu SD, Xian GZ, Yang S. Complications analysis with postoperative choledochoscopy for residual bile duct stones. World J Surg 2010;34:574–80. [DOI] [PubMed] [Google Scholar]
- [13].Kumon M. Anatomical study of the caudate lobe with special reference to portal venous and biliary branches using corrosion liver casts and clinical application. Liver Cancer 2017;6:161–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Li EL, Yuan RF, Liao WJ, et al. Intrahepatic bile duct exploration lithotomy is a useful adjunctive hepatectomy method for bilateral primary hepatolithiasis: an eight-year experience at a single centre. BMC Surg 2019;19:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Tsuyuguchi T, Miyakawa K, Sugiyama H, et al. Ten-year long-term results after non-surgical management of hepatolithiasis, including cases with choledochoenterostomy. J Hepatobiliary Pancreat Sci 2014;21:795–800. [DOI] [PubMed] [Google Scholar]
- [16].Ali JM, See TC, Wiseman O, Griffiths WJ, Jah A. Salvage of liver transplant with hepatolithiasis by percutaneous transhepatic cholangioscopic hepatolithotomy. Transpl Int 2014;27:e126–8. [DOI] [PubMed] [Google Scholar]
- [17].Wen ZQ, Yan YQ, Yang JM, Wu MC. Precautions in caudate lobe resection: report of 11 cases. World J Gastroenterol 2008;14:2767–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Disci E, Atamanalp SS, Ozogul B, Yildirgan MI. The role of choledochoscopy in hepatopancreatobiliary diseases. Eurasian J Med 2016;48:29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ayoub F, Yang D, Draganov PV. Cholangioscopy in the digital era. Transl Gastroenterol Hepatol 2018;3:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Takamatsu S, Goseki N, Nakajima K, Teramoto K, Iwai T, Arii S. Distributing pattern of the bile duct of the caudate lobe on computed tomography with drip infusion cholangiography and its surgical significance. Hepatogastroenterology 2004;51:29–32. [PubMed] [Google Scholar]
- [21].Edo H, Sekiguchi R, Edo N, Kajiyama A, Nagamoto M, Gomi T. Evaluation of biliary anatomy in the caudate lobe using drip infusion cholangiography-computed tomography. Abdom Radiol (NY) 2019;44:886–93. [DOI] [PubMed] [Google Scholar]
- [22].Wen XD, Xiao L, Wang T, Navarro-Alvarez N, Liu WH. Routine guidewire application facilitates cholangioscopy in the management of postoperative residual hepatolithiasis. Dig Endosc 2018;30:372–9. [DOI] [PubMed] [Google Scholar]