Abstract
Objective
Due to partial or poorly enforced restrictions secondhand tobacco smoke (SHS) is still present in outdoor hospitality venues in many European countries. This study aimed to assess SHS concentrations in outdoor hospitality venues across Europe and identify contextual exposure determinants.
Methods
Cross-sectional study. We measured airborne nicotine and evidence of tobacco use in terraces of bars, cafeterias, and pubs from 11 European countries in 2017–2018. Sites were selected considering area-level socioeconomic indicators and half were visited during nighttime. We noted the smell of smoke, presence of smokers, cigarette butts, ashtrays, and number of physical covers. Contextual determinants included national smoke-free policies for the hospitality sector, the Tobacco Control Scale score (2016), and the national smoking prevalence (2017–2018). We computed medians and interquartile ranges (IQR) of nicotine concentrations and used multivariate analyses to characterize the exposure determinants.
Results
Nicotine was present in 93.6% of the 220 sites explored. Overall concentrations were 0.85 (IQR:0.30–3.74) μg/m3 and increased during nighttime (1.45 IQR:0.65–4.79 μg/m3), in enclosed venues (2.97 IQR:0.80–5.80 μg/m3), in venues with more than two smokers (2.79 IQR:1.03–6.30 μg/m3), in venues in countries with total indoor smoking bans (1.20 IQR:0.47–4.85 μg/m3), and in venues in countries with higher smoking prevalence (1.32 IQR:0.49–5.34 μg/m3). In multivariate analyses, nicotine concentrations were also positively associated with the observed number of cigarette butts. In venues with more than two smokers, SHS levels did not significantly vary with the venues’ degree of enclosure.
Conclusions
Our results suggest that current restrictions in outdoor hospitality venues across Europe have a limited protective effect and justify the adoption of total smoking bans in outdoor areas of hospitality venues.
Keywords: Tobacco-smoke pollution, Airborne nicotine, Smoke-free policies, Outdoor, Hospitality venue
Highlights
-
•
94% of the outdoor premises had nicotine and in 92% there were people smoking.
-
•
All outdoor hospitality terraces where smoking was not allowed had smokers.
-
•
When >2 smokers were present, SHS levels did not vary with the venue's enclosure.
-
•
SHS exposure increased at night and in countries with higher smoking prevalence.
-
•
Our data indicate the need for total smoking bans in outdoor hospitality venues.
1. Introduction
Tobacco use releases carcinogens, toxic agents, and pollutants contained in the smoke into the environment (WHO, 2017). Secondhand smoke (SHS) is a prevalent environmental risk factor and a known cause of lung cancer, cardiovascular and respiratory disease in non-smokers (U.S. Department of Health and Human Services, 2006). The World Health Organization state only complete smoke-free environments fully protect non-smokers from the harms of SHS exposures (WHO, 2007).
Indoor smoking bans in hospitality venues have helped reduce SHS exposure (Mulcahy et al., 2005; López et al., 2013) and improve the respiratory health of hospitality workers (Fernández et al., 2009). Still, some studies have questioned if indoor bans alone are sufficient to entirely prevent SHS exposure inside hospitality venues, and advocate for the extension of smoke-free policies to the outdoor areas of such establishments (Mulcahy et al., 2005; Edwards and Wilson, 2011; López et al., 2012, 2013). Based on the assessment of airborne nicotine and PM2.5 concentrations, these studies show SHS levels to be higher inside hospitality venues with outdoor smoking occurring, indicating tobacco smoke can migrate from outdoor settings to nearby indoor areas (Mulcahy et al., 2005; Edwards and Wilson, 2011; López et al., 2012, 2013). Also, Fu et al. (2016) simultaneously measured SHS levels inside and in the outside entrances of cafés and restaurants finding concentrations in both spaces to be directly related.
An unintended consequence of legislation to prevent smoking inside hospitality venues has been the relocation of tobacco consumption to outdoor areas, also leading to a proliferation of outdoor smoking shelters in these settings post-ban. For instance, reported smoking outdoors increased from 33.6% to 75.9% at cafés, bars, or pubs and from 28.9% to 59.0% at restaurants after the French ban on smoking in the hospitality sector (Kennedy et al., 2012). In the city of Barcelona, outside areas in bars and restaurants were the most common outdoor places for smokers to smoke following comprehensive legislation for all indoor public places (Sureda et al., 2015). Moreover, hospitality venue surroundings in the city of Madrid were the outdoor areas with the highest visibility of smokers (Valiente et al., 2020). Given that outdoor hospitality settings are usually on the street and visible for pedestrians, regulations restricting indoor smoking may have also enhanced the visibility of smoking (Kennedy et al., 2010). Smoking visibility in public places is a drawback for tobacco use denormalization and has been associated with positive beliefs towards smoking among European adolescents (Lagerweij et al., 2019).
With tobacco use moving to the outside sections of hospitality establishments, SHS exposure in outdoor settings has gained more attention. A study in eight European countries found airborne nicotine levels to be significantly higher in outdoor areas of hospitality venues with indoor smoking restrictions, compared to those without such measures (López et al., 2012). The outdoor SHS levels reported in this study were considerably higher than those found in households with residential smokers that allowed smoking inside (Arechavala et al., 2018). Other research further characterizing SHS exposure at outdoor hospitality settings also demonstrated that SHS concentrations can be high and increase with the degree of enclosure, smoker density, and the number of active cigarettes (Stafford et al., 2010; Licht et al., 2013; Fu et al., 2016; Sureda et al., 2013, 2018). Furthermore, biomarkers of SHS exposure (i.e. salivary cotinine and urinary NNAL (4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol)) were significantly higher in non-smokers after visiting outdoor hospitality areas when compared to visiting open-air sites free of smokers (St.Helen et al., 2012). Thus, SHS exposure continues to be a significant health hazard in hospitality venues, and total outdoor smoking bans should be adopted especially to protect those who are occupationally exposed.
Some countries in Europe have restricted smoking according to the number of physical structures delimiting each site. Greece, Ireland, Romania, Spain, and the UK outlawed smoking in venues that are covered and have more than two sidewalls. In France, smoking is not permitted in covered venues where the main side or façade is closed. However, while current restrictions rely on the premise that there are low SHS levels in outdoor spaces (Kennedy et al., 2010) available evidence shows SHS exposure outdoors can substantially increase with just the presence of overhead covers (Cameron et al., 2010; Licht et al., 2013; Fu et al., 2016). Besides, there are other issues with these types of partial bans. In general, the law is ambiguous in defining what should be considered an open space and there is often low compliance in these settings, particularly in cold seasons (Sureda et al., 2018). The determinants of exposure to SHS in outdoor areas of hospitality venues are unclear but may include factors such as area-level socioeconomic status, season, time of the day, and number of smokers. In this study, we aimed to describe SHS concentrations and evidence of tobacco use in outdoor hospitality venues across Europe, and assess the association with different contextual exposure determinants.
2. Methods
2.1. Study design
This study is part of the TackSHS project, developed to comprehensively explore the extent and impact of SHS and electronic cigarette emissions in Europe (Fernández et al., 2020). In this cross-sectional study conducted between March 2017 and April 2018, we objectively assessed SHS exposure concentrations at outdoor terraces in hospitality venues that were located in large urban areas from 11 European countries: Bulgaria, France, Germany, Greece, Ireland, Italy, Poland, Portugal, Romania, Spain, and the United Kingdom (UK). In each of the countries, we used a convenience sampling strategy to identify 20 different sites, taking a total of 220 outdoor environmental measurements. Venues were selected considering the neighborhoods’ socioeconomic status (SES), which we determined through different socioeconomic indicators (Henderson et al., 2020a). Half the measurements were performed in more deprived neighborhoods, below the 20th percentile of the SES distribution, and half in wealthier neighborhoods, above the 80th percentile of the SES distribution. In this study, we also intended to explore differences in SHS exposure by time of the day. Site visits were arranged so that half the measurements were carried out during day hours and the other half during night hours, preferably after dinner hours. Each country specified daytime and nighttime hours and all visits were unannounced and carried out covertly to avoid bias. Moreover, fieldwork was planned to avoid months with more extreme temperatures: no measurements were taken in any country December to February and only in Bulgaria, Poland, and the UK some measurements were taken during July or August. Eligibility for inclusion was restricted to the outdoor areas of bars, cafeterias, or pubs that had at least one sidewall or overhead cover. We monitored SHS concentrations only when five or more customers (adults and/or children) were present. Researchers in charge of the fieldwork were previously trained and equipped with a sampling protocol for additional guidance.
2.2. Nicotine measurements
We measured vapor-phase nicotine, a tobacco-specific constituent, as an indicator for SHS exposure. Nicotine samples were collected on a 37-mm diameter polystyrene cassette holding a filter coated with sodium bisulfate. The sampling methodology we followed had been validated prior to this study (Hammond et al., 1987). We carried nicotine samplers connected to air pumps (Sidekick, SKC Ltd., Dorset, UK). Air pumps were calibrated before and after the fieldwork, allowing us to keep track of the volume of air actively filtered. We set the flow rate at 3 l/min with Defender 510 M (Mesa Labs, Lakewood, CO, USA) calibrator. Air sampling lasted up to approximately 30 min at each venue. Researchers sat at any available table on the outdoor terrace throughout the whole sampling period. Nicotine samples were identified with a unique code paired to a form filled in during each measurement. Once the measurements ended, filters were stored and sent to the Agència de Salut Pública de Barcelona laboratory together with blank filters. The laboratory determined nicotine concentrations using gas chromatography-mass spectrometry. In each batch, the blank filter, a negative sample (solvent), and a fortified sample served as quality control. We calculated the time-weighted average nicotine concentration (μg/m3) dividing the mass of nicotine extracted from the filter by the volume of air filtered (flow rate multiplied by the duration the sampler was exposed). The laboratory had a limit of quantification (LOQ) of 0.06 μg/m3. Concentrations were dichotomized into presence/absence of nicotine using this LOQ as the cut-off point.
2.3. Observational data
Concurrently to monitoring nicotine levels, researchers screened for evidence of tobacco use within the outdoor areas of each hospitality venue: the smell of tobacco smoke (as subjectively assessed by the researcher), visual evidence of people smoking, presence of cigarette butts, ashtrays or similar receptacles. Data were recorded in a specific form at three measurement points: at the start, half-way through the visit (approximately 15 min), and at the end. In the analyses, there was a smell of smoke and people were smoking if applicable in at least one of the three-time points. We also calculated the average number of smokers observed in each venue in the three-time points. Subsequently, we used the median value of smokers (1.6 smokers) to classify venues into two categories: those with two or fewer smokers and those with more than two smokers. We considered there were cigarette butts when researchers noticed that one or more cigarette butts had been discarded, including those lying on the adjoining pavement and in ashtrays. The form was also used to note other relevant information: date and time of sampling, type of venue, number of sidewalls, and presence of overhead covers.
2.4. Contextual variables
Contextual data were extracted from multiple sources. We grouped terraces into three different levels of enclosure (no roof + 0–4 walls, roof + 0–2 walls, roof + 3–4 walls) using the information compiled during the fieldwork on the structures delimiting each site. Categories were set after reviewing the national smoke-free policies for outdoor hospitality venues during 2017–2018. Except for France, jurisdictions with regulations allowed smoking in sites with no overhead covers, or with overhead covers and up to a maximum of two sidewalls (Supplementary Table 1). We further categorized sites combining data on outdoor smoke-free regulations and the degree of enclosure. We defined three categories: venues in the highest level of enclosure (roof + 3–4 walls) were divided according to whether smoking was banned (regulated terraces and terraces in France with four sidewalls) or allowed (terraces with no regulation and terraces in France with three sidewalls); a third category included all other terraces since smoking was permitted regardless of the existence of national smoking regulations for outdoor hospitality venues. Given the possible relocation of smoking behaviors towards the outdoor areas of hospitality venues with total indoor smoking bans, we also checked for the national indoor smoke-free legislation in the hospitality sector. Germany, Italy, Poland, and Portugal allowed smoking rooms if certain standards are met, but the other seven countries had total smoking bans for the indoor areas (Supplementary Table 1). We used the Tobacco Control Scale 2016 overall score (Joossens and Raw, 2016), which is a 100-point scale measuring six tobacco control policies, to differentiate countries by their tobacco control activity. Following the 2016 edition report, we classified countries with scores above or equal to 50 points in one group and countries below 50 points in another, as done in previous studies (Henderson et al., 2020a, Henderson et al., 2020b, Henderson et al., 2021). Finally, we acquired data on the country's smoking prevalence from a European survey conducted as part of the TackSHS project in a representative sample aged 15 years and older in 2017–2018 (Fernández et al., 2020; Gallus et al., 2021). The respondents were smokers if they reported smoking at the time of the survey and had smoked at least 100 cigarettes, including roll-your-own cigarettes. We generated two categories with the median smoking prevalence (31%) as the cut-off point.
2.5. Statistical analyses
Nicotine samples below the laboratory's LOQ were given half this value in the statistical analyses. Concentration values were not normally distributed. For this reason, we provide medians and their corresponding interquartile ranges (IQR). We applied U-Mann Whitney or Kruskal Wallis test to compare median nicotine concentrations across countries and contextual variables. We report raw frequencies and percentages to describe tobacco-related observational data, which we compared with the Chi-squared test. We plotted nicotine concentrations according to the degree of enclosure and stratifying by the number of smokers. We also fitted a multiple regression model to analyze the relationship between observational and contextual variables, and nicotine levels in the outdoor areas of hospitality venues. Because of the skewed distribution, we used the log-transformed concentrations. The final model was tested for normality of errors, homoscedasticity, absence of outliers, multicollinearity, and self-correlation. The level of statistical significance was set at 5%. All analyses were performed with the statistical package STATA 15.
2.6. Ethical issues
The TackSHS project was approved by the Clinical Research Ethics Committee of the Bellvitge University Hospital (PR341/15) and this study was approved by each country's local Ethics Committees. The study protocol was registered in ClinicalTrials.gov (ID: NCT03150186).
3. Results
Overall, SHS was present in 93.6% of the 220 venues and the median nicotine concentration was 0.85 μg/m3 (IQR: 0.30–3.74 μg/m3). Romania (3.12 μg/m3 IQR: 0.88–6.69 μg/m3), Ireland (2.55 μg/m3 IQR: 0.53–6.43 μg/m3), Greece (2.29 μg/m3 IQR: 1.13–3.66 μg/m3), and France (2.16 μg/m3 IQR: 0.64–5.05 μg/m3) had the highest median nicotine concentrations. We identified people smoking in more than 90% of the terraces, with smokers being present at all the sites visited in Bulgaria, France, Greece, Ireland, Italy, and Spain. There was smell of tobacco smoke at around 80% of the outdoor establishments. Three-quarters of the terraces had discarded cigarette butts and at almost nine out of ten venues ashtrays or similar receptacles were observed (Table 1).
Table 1.
Airborne nicotine concentration (μg/m3) and tobacco-related signs in outdoor terraces of hospitality venues by country (2017–2018).
| Country | N | Nicotine concentration (μg/m3) Median (μg/m3) (IQR) |
Nicotine presence % (n) |
Smell of smoke % (n) |
People smoking % (n) |
Cigarette butts % (n) |
Ashtrays % (n) |
|---|---|---|---|---|---|---|---|
| Overall | 220 | 0.85 (0.30–3.74) | 93.6 (206) | 82.3 (181) | 92.3 (203) | 74.6 (164) | 87.7 (193) |
| Bulgaria | 20 | 0.66 (0.37–4.21) | 95.0 (19) | 90.0 (18) | 100.0 (20) | 75.0 (15) | 100.0 (20) |
| France | 20 | 2.16 (0.64–5.05) | 100.0 (20) | 100.0 (20) | 100.0 (20) | 70.0 (14) | 80.0 (16) |
| Germany | 20 | 0.38 (0.24–1.00) | 90.0 (18) | 65.0 (13) | 80.0 (16) | 80.0 (16) | 85.0 (17) |
| Greece | 20 | 2.29 (1.13–3.66) | 100.0 (20) | 80.0 (16) | 100.0 (20) | 20.0 (4) | 95.0 (19) |
| Ireland | 20 | 2.55 (0.53–6.43) | 95.0 (19) | 95.0 (19) | 100.0 (20) | 90.0 (18) | 95.0 (19) |
| Italy | 20 | 1.36 (0.88–3.10) | 95.0 (19) | 90.0 (18) | 100.0 (20) | 100.0 (20) | 90.0 (18) |
| Poland | 20 | 0.13 (<0.06–0.36) | 70.0 (14) | 70.0 (14) | 70.0 (14) | 65.0 (13) | 80.0 (16) |
| Portugal | 20 | 0.31 (0.17–3.46) | 95.0 (19) | 90.0 (18) | 95.0 (19) | 80.0 (16) | 80.0 (16) |
| Romania | 20 | 3.12 (0.88–6.69) | 100.0 (20) | 95.0 (19) | 95.0 (19) | 60.0 (12) | 100.0 (20) |
| Spain | 20 | 0.87 (0.49–5.16) | 100.0 (20) | 95.0 (19) | 100.0 (20) | 100.0 (20) | 85.0 (17) |
| UK | 20 | 0.25 (0.08–0.47) | 90.0 (18) | 35.0 (7) | 75.0 (15) | 80.0 (16) | 75.0 (15) |
| p-value | 0.0001a | 0.005b | <0.0001b | <0.0001b | <0.0001b | 0.161b |
Note: IQR, Interquartile Range. Limit of Quantification (LOQ): 0.06 μg/m3.
Kruskal-Wallis test.
Chi-squared test.
We found significantly higher median nicotine concentrations in venues visited during nighttime hours (1.45 μg/m3 IQR: 0.56–4.79 μg/m3), in those with two or more smokers (2.79 μg/m3 IQR: 1.03–6.30 μg/m3), in countries with total indoor smoking bans (1.20 μg/m3 IQR: 0.47–4.85 μg/m3), and in countries with higher smoking prevalence (1.32 μg/m3 IQR: 0.49–5.34 μg/m3). Compared to venues with lower levels of enclosure, median concentrations were significantly increased in terraces with overhead covers and 3 to 4 walls (2.97 μg/m3 IQR: 0.80–5.80 μg/m3). Moreover, median concentrations were higher in terraces with overhead covers and 3 to 4 walls where smoking was allowed (3.49 μg/m3 IQR: 1.19–6.46 μg/m3) in contrast to terraces with the same degree of enclosure but where smoking was banned (2.11 μg/m3 IQR: 0.58–5.62 μg/m3). Terraces with lower degrees of enclosure where smoking was also allowed had the lowest concentrations (0.71 μg/m3 IQR: 0.25–2.67 μg/m3) (Table 2).
Table 2.
Airborne nicotine concentration (μg/m3) in outdoor terraces of hospitality venues by area-level socioeconomic status, time of the day, terrace degree of enclosure, smoke-free regulations, Tobacco Control Scale overall score, and national smoking prevalence (2017–2018).
| Contextual factors | N | Median (μg/m3) (IQR) | p-valuea | Min (μg/m3) | Max (μg/m3) |
|---|---|---|---|---|---|
| Overall | 220 | 0.85 (0.30–3.74) | <0.06 | 77.40 | |
| SES | |||||
| High | 107 | 0.74 (0.23–2.85) | <0.06 | 20.50 | |
| Low | 113 | 1.00 (0.35–4.34) | 0.133 | <0.06 | 77.40 |
| Time of the day | |||||
| Daytime | 115 | 0.50 (0.19–2.57) | <0.06 | 77.40 | |
| Nighttime | 105 | 1.45 (0.56–4.79) | 0.0001 | <0.06 | 68.07 |
| Number of smokersb | |||||
| ≤2 smokers | 130 | 0.49 (0.16–1.13) | <0.06 | 77.40 | |
| >2 smokers | 90 | 2.79 (1.03–6.30) | <0.0001 | 0.117 | 68.07 |
| Degree of enclosure | |||||
| No roof and 0–4 walls | 63 | 0.47 (0.14–2.32) | <0.06 | 68.07 | |
| Roof and 0–2 walls | 113 | 0.76 (0.29–3.69) | 0.001 | <0.06 | 77.40 |
| Roof and 3–4 walls | 44 | 2.97 (0.80–5.80) | <0.06 | 31.64 | |
| Regulation site | |||||
| Roof and 3–4 walls banned | 23 | 2.11 (0.58–5.62) | <0.06 | 12.71 | |
| Roof and 3–4 walls allowed | 21 | 3.49 (1.19–6.46) | 0.001 | <0.06 | 31.64 |
| Others allowed | 176 | 0.71 (0.25–2.67) | <0.06 | 77.40 | |
| Indoor total smoking ban | |||||
| No | 80 | 0.49 (0.15–2.25) | <0.06 | 77.40 | |
| Yes | 140 | 1.20 (0.47–4.85) | 0.0003 | <0.06 | 54.50 |
| TCS overall scorec | |||||
| ≥50 points | 160 | 0.84 (0.25–3.74) | <0.06 | 77.40 | |
| <50 points | 60 | 0.90 (0.37–3.32) | 0.449 | <0.06 | 68.07 |
| Smoking prevalence (2017–18)d | |||||
| <31% | 100 | 0.53 (0.12–2.15) | <0.06 | 68.07 | |
| ≥31% | 120 | 1.32 (0.49–5.34) | <0.0001 | <0.06 | 77.40 |
Note: SES, socioeconomic status; TCS, Tobacco Control Scale.
Mann-Whitney U test or Kruskal Wallis test.
Average number of smokers in the three-time periods categorized using the median value of 1.6 smokers.
TCS overall score: ≥50 (France, Italy, Ireland, Poland, Portugal, Romania, Spain, UK); <50 (Bulgaria, Germany, Greece).
Based on a European survey conducted in the TackSHS project. Smoking prevalence (median): <31% (Germany, Ireland, Italy, Poland, UK); ≥31% (Bulgaria, France, Greece, Portugal, Romania, Spain).
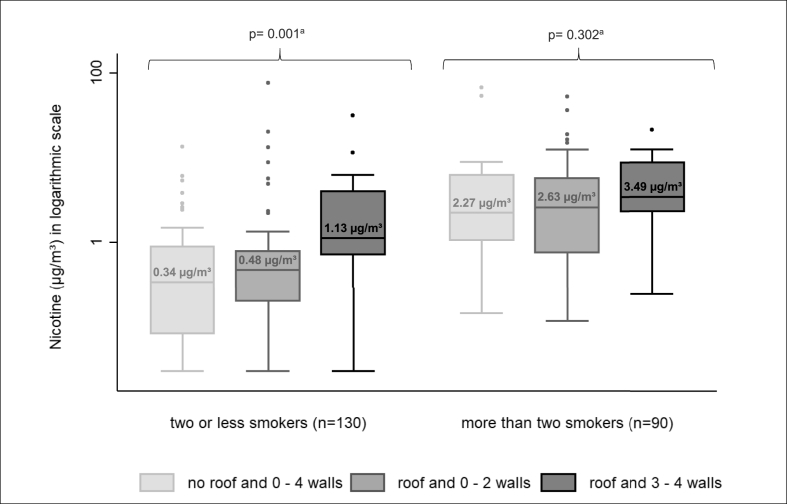
In Fig. 1 we show median nicotine concentrations according to the level of enclosure and stratifying by the number of smokers. In those terraces with 2 or less smokers, SHS concentrations significantly increased with the venues’ degree of enclosure (p < 0.05). In turn, when more than 2 smokers were present median concentrations slightly increased but did not significantly differ between levels of enclosure.
Fig. 1.
Nicotine distribution and median concentrations (μg/m3) in outdoor areas of hospitality venues according to the degree of enclosure and stratifying by the average number of smokers present in the observation. N = 220. TackSHS project 2017–2018. Note: For layout purposes, nicotine distribution is represented in a logarithmic scale. Values correspond to median nicotine concentrations in each category.
aKruskal-Wallis test.
We more often noticed people smoking in outdoor areas of venues with total indoor smoking bans, and smell of tobacco smoke and people smoking in countries with higher smoking prevalence (p < 0.05). Both these tobacco-related signs were also more common in venues with roofs and 3 to 4 walls. Moreover, all the sites visited where smoking was already banned had people smoking (Table 3).
Table 3.
Tobacco-related variables in outdoor terraces of hospitality venues by area-level socioeconomic status, time of the day, terrace degree of enclosure, smoke-free regulations, Tobacco Control Scale overall score, and national smoking prevalence (2017–2018).
| Contextual factors | N | Smell of smoke % (n) |
People smoking % (n) |
Cigarette butts % (n) |
Ashtrays % (n) |
|---|---|---|---|---|---|
| Overall | 82.3 (181) | 92.3 (203) | 74.6 (164) | 87.7 (193) | |
| SES | |||||
| High | 107 | 80.4 (86) | 90.7 (97) | 70.1 (75) | 89.7 (96) |
| Low | 113 | 84.1 (95) | 93.8 (106) | 78.8 (89) | 85.8 (97) |
| p-valuea | 0.473 | 0.382 | 0.140 | 0.381 | |
| Time of the day | |||||
| Daytime | 115 | 80.9 (93) | 89.6 (103) | 67.0 (77) | 86.1 (99) |
| Nighttime | 105 | 83.8 (88) | 95.2 (100) | 82.9 (87) | 89.5 (94) |
| p-valuea | 0.568 | 0.116 | 0.007 | 0.438 | |
| Degree of enclosure | |||||
| No roof and 0–4 walls | 63 | 71.4 (45) | 84.1 (53) | 65.1 (41) | 82.5 (52) |
| Roof and 0–2 walls | 113 | 85.0 (96) | 93.8 (106) | 74.3 (84) | 89.4 (101) |
| Roof and 3–4 walls | 44 | 90.9 (40) | 100.0 (44) | 88.6 (39) | 90.9 (40) |
| p-valuea | 0.019 | 0.007 | 0.023 | 0.321 | |
| Regulation site | |||||
| Roof and 3–4 walls banned | 23 | 91.3 (21) | 100.0 (23) | 82.6 (19) | 87.0 (20) |
| Roof and 3–4 walls allowed | 21 | 90.5 (19) | 100.0 (21) | 95.2 (20) | 95.2 (20) |
| Others allowed | 176 | 80.1 (141) | 90.3 (159) | 71.0 (125) | 86.9 (153) |
| p-valuea | 0.244 | 0.100 | 0.035 | 0.544 | |
| Indoor total smoking ban | |||||
| No | 80 | 78.8 (63) | 86.3 (69) | 81.3 (65) | 83.8 (67) |
| Yes | 140 | 84.3 (118) | 95.7 (134) | 70.7 (99) | 90.0 (126) |
| p-valuea | 0.301 | 0.011 | 0.084 | 0.174 | |
| TCS overall scoreb | |||||
| ≥50 points | 160 | 83.8 (134) | 91.9 (147) | 80.6 (129) | 85.6 (137) |
| <50 points | 60 | 78.3 (47) | 93.3 (56) | 58.3 (35) | 93.3 (56) |
| p-valuea | 0.349 | 0.718 | 0.001 | 0.121 | |
| National smoking prevalence (2017–18)c | |||||
| <31% | 100 | 71.0 (71) | 85.0 (85) | 83.0 (83) | 85.0 (85) |
| ≥31% | 120 | 91.7 (110) | 98.3 (118) | 67.5 (81) | 90.0 (108) |
| p-valuea | <0.0001 | <0.0001 | 0.009 | 0.260 |
Note: SES, socioeconomic status; TCS, Tobacco Control Scale.
Chi-squared test.
TCS overall score: ≥50 (France, Italy, Ireland, Poland, Portugal, Romania, Spain, UK); <50 (Bulgaria, Germany, Greece).
Based on a European survey conducted in the TackSHS project. Smoking prevalence (median): <31% (Germany, Ireland, Italy, Poland, UK); ≥31% (Bulgaria, France, Greece, Portugal, Romania, Spain).
According to multiple linear regression analysis, nicotine concentrations at terraces significantly increased during nighttime hours β = 0.49 (95%CI: 0.10–0.88), when more than two smokers were present β = 1.37 (95%CI: 0.98–1.77), with discarded cigarette butts β = 0.56 (95%CI: 0.09–1.02), with the highest level of enclosure (roof and 3 to 4 walls) β = 0.74 (95%CI: 0.15–1.33), in countries with indoor smoking bans β = 0.61 (95%CI: 0.14–1.08), and in countries with higher smoking prevalence β = 0.63 (95%CI: 0.16–1.10) (Table 4).
Table 4.
Multivariable analyses of log-transformed nicotine concentrations in outdoor terraces of hospitality venues in 11 European countries (2017–2018).
| Bivariate model |
Multivariate model |
||||
|---|---|---|---|---|---|
| β (95% CI) | p-value | β (95% CI) | p-value | R2adj | |
| 0.3498 | |||||
| Constant | −2.46 (−3.09, −1.84) | <0.0001 | |||
| SES (ref. high) | 0.38 (−0.09, 0.84) | 0.115 | 0.38 (−0.01, 0.77) | 0.058 | |
| Time of the day (ref. daytime) | 0.86 (0.40, 1.31) | <0.0001 | 0.49 (0.10, 0.88) | 0.015 | |
| Number of smokers (ref. 2 or less smokers) | 1.63 (1.21, 2.06) | <0.0001 | 1.37 (0.98, 1.77) | <0.0001 | |
| Presence of butts (ref. no presence of butts) | 0.70 (0.17, 1.23) | 0.010 | 0.56 (0.09, 1.02) | 0.019 | |
| Degree of enclosure (ref. no roof and 0–4 walls) | |||||
| No roof and 0–2 walls | 0.47 (−0.06, 1.01) | 0.082 | 0.24 (−0.26, 0.74) | 0.352 | |
| Roof and 3–4 walls | 1.21 (0.55, 1.88) | <0.0001 | 0.74 (0.15, 1.33) | 0.015 | |
| Indoor total smoking ban (ref. no) | 0.89 (0.42, 1.37) | <0.0001 | 0.61 (0.14, 1.08) | 0.011 | |
| National smoking prevalence (ref. <31%) | 1.07 (0.62, 1.52) | <0.0001 | 0.63 (0.16, 1.10) | 0.009 | |
Note: ref, reference; CI, Confidence Interval; SES, socioeconomic status.
4. Discussion
This study shows concentrations of airborne nicotine, a marker of SHS, in terraces or outdoor areas of hospitality premises in 11 European countries. SHS was present in more than 90% of the outdoor areas, demonstrating exposure to SHS among non-smokers in Europe is likely to occur in this type of setting. We found higher levels of exposure during nighttime, in sites with overhead covers and 3 to 4 sidewalls, with more than two smokers, and with discarded cigarette butts. Also, there were higher concentrations of SHS in outdoor areas in countries with total smoking bans inside hospitality venues, and among countries with higher national smoking prevalence. Our findings also revealed that when more than two smokers were present SHS levels remained high irrespective of the venues’ degree of enclosure, indicating current smoke-free regulations based on the number of physical covers do not provide adequate protection to customers and hospitality workers.
The results point to increased exposure levels during night hours. This outcome is consistent with one study in Europe finding higher outdoor nicotine concentrations in bars at night (López et al., 2012), and with two studies in New Zealand reporting higher smoking visibility in outside hospitality areas in the evenings (Chan et al., 2014; Pearson et al., 2014). In our study, however, we did not find differences in the presence of smokers between daytime and nighttime hours. A possible explanation for the finding of higher nicotine concentrations at night could be a different patronage according to the time of the day. The purpose of smokers going to hospitality venues during nighttime might be more related to leisure activities and, perhaps, higher levels of tobacco consumption (Chan et al., 2014). This argument would be in line with our result on venues having more discarded cigarette butts at later hours. Even so, this indicator could also reflect the cigarettes smoked over the whole day period or be the result of a cleaning effect, with cigarette butts being swept up once per day at the end of the shift or at the start of each day. Since health inspections are more likely performed during regular office hours, differences in exposure by time of the day could also be explained by a lower adherence to smoking restrictions at night (Peruga et al., 2020).
Nicotine concentrations substantially increased with the venue's degree of enclosure of the outdoor space. Sites with overhead covers and a minimum of three sidewalls had more than twice the median concentrations than less enclosed venues. Earlier studies assessing SHS exposure with airborne markers have reported similar results (Cameron et al., 2010; Stafford et al., 2010; Licht et al., 2013; Fu et al., 2016; Sureda et al., 2018). One study even noted that the presence of overhead covers in outdoor hospitality premises raised average exposure levels by virtually 50% (Cameron et al., 2010). In the present analyses, we further evaluated SHS exposure levels combining the conditions of enclosure with the smoking restrictions for outdoor hospitality areas. As expected, among the sites with the greatest level of enclosure SHS exposure was highest in countries where smoking outdoors was permitted. Yet, to our surprise, terraces where smoking was already banned had high concentrations which were comparable to the levels found in some countries before smoking was banned in indoor hospitality premises (Lopez et al., 2008). This generalized non-compliance was confirmed by the observed presence of smokers in all the venues we visited. Enforcement and compliance might be challenging based on ambiguous regulatory frameworks. In the included European countries, current smoke-free policies for outdoor hospitality venues leave some room for interpretation. While smoking is banned in enclosed places (generally, areas with overhead covers and more than two walls), the laws do not provide a formal definition of what should be considered a sidewall or an overhead cover. Physical coverings might be movable, partial or complete structures, might have openings or windows, might be made of very different materials, and might be placed at different heights. Unclear regulations result in legal loopholes and confusion in the policy's interpretation. Adopting complete smoking bans in all outdoor hospitality areas would certainly remedy both these issues.
Although accumulating evidence supports the notion of higher SHS exposure levels in more enclosed areas (Cameron et al., 2010; Stafford et al., 2010; Licht et al., 2013; Fu et al., 2016; Sureda et al., 2018), this study demonstrates smoke-free policies should not depend on the degree of enclosure to limit smoking behaviors in outdoor hospitality settings. In our analyses, when more than two people were smoking at the venue, SHS concentrations scaled-up and did not significantly vary across the different stages of enclosure defined in current regulations. These results might imply that the smoking restrictions adopted in several European countries have a limited protective effect and reinforce the need for total outdoor smoking bans. Previous literature has shown that even brief SHS exposures could impair several biological mechanisms leading to detrimental health effects on non-smokers (Flouris et al., 2010). Therefore, despite smoking being restricted, SHS exposure levels might still represent a threat to health, especially in the case of vulnerable populations attending hospitality venues (Keogan et al., 2020), and for those who are exposed on a regular basis, such as hospitality workers.
Outdoor hospitality venues in Romania, Ireland, Greece, and France had very high nicotine concentrations. Overall exposure levels in these countries were similar to those reported in the indoor areas of 82 cafeterias and restaurants in 10 European cities (Lopez et al., 2008). By the time this study took place, these countries, as well as Spain and the UK, had enacted total indoor smoking bans for the hospitality sector. As suggested in earlier research, indoor smoke-free policies in hospitality venues seem to have displaced tobacco use, and thus, potential SHS exposures to adjacent outdoor areas (Kennedy et al., 2010; López et al., 2012; van Beek et al., 2019). Our study also showed significantly higher SHS levels and presence of smokers in the outdoor areas of venues covered by indoor smoke-free policies. Consequently, we provide further proof that indoor smoke-free policies in hospitality venues should be accompanied by total outdoor smoking bans to be truly effective measures.
Unlike other outdoor settings, where nicotine concentrations were lower in countries with higher scores in the TCS (Henderson et al., 2020a, Henderson et al., 2020b, Henderson et al., 2021), this study focusing on outdoor hospitality areas did not find differences in SHS exposure levels according to the countries’ TCS total score in 2016. This discrepancy between different types of outdoor spaces might be explained by the fact that outdoor hospitality premises are, apart from popular places for smoking, one of the only spaces where, under most circumstances, smoking is currently allowed across all of the countries studied.
We observed disparities in the SHS exposure levels by national smoking prevalence. In agreement with what has been found in other outdoor areas (Henderson et al., 2020a, Henderson et al., 2020b, Henderson et al., 2021), and the indoor spaces of bars and restaurants (Filippidis et al., 2016), SHS exposure levels were higher in venues located in countries with greater national smoking prevalence. Countries with higher smoking prevalence also had a significantly higher presence of visual (smokers) and olfactory (smell of tobacco smoke) smoking stimuli at terraces. Outdoor hospitality areas are social venues commonly patronized by young people, and where smoking, as evidenced in bars, night clubs, and gaming venues, could be socially cued (Trotter et al., 2002). In this sense, smoke-free policies targeting outdoor hospitality premises might be particularly relevant to advance the denormalization of smoking, as well as reducing opportunities to smoke, and help smokers with quit attempts (Chaiton et al., 2016; Satterlund et al., 2012).
Despite the continuing obligation under Article 8 of the WHO FCTC and Article 8 Guidelines to prohibit smoking in outdoor or quasi-outdoor places with proof of a possible health hazard, the absence of a comprehensive approach to smoking bans for hospitality venues is a common trait of all countries in the study. The protracted resistance to smoke-free laws in these settings contrasts with the compelling evidence supporting the fact that this type of interventions not only curtail tobacco-related health and economic costs (Hahn, 2010) but also do not adversely affect the hospitality industry (World Health Organization Regional Office for Europe, 2019).
Some limitations to this research should be acknowledged. We selected the outdoor venues following a convenience sampling approach. Therefore, we cannot extrapolate our results to other terraces in the same city or country. The nature of our sample, however, does not hinder the study's objective of evaluating SHS concentrations in outdoor hospitality venues considering different exposure determinants. Second, we gathered SHS information on a limited number of 20 sites per country. Consequently, data have been analyzed grouping the sample of venues according to contextual factors. Finally, our exposure assessment represents short 30-min measurements of airborne nicotine concentrations on one occasion in each venue. Earlier studies report higher smoking visibility in hospitality areas during weekends (Pearson et al., 2014). Since fieldwork was performed mostly on weekdays and SHS levels are likely greater at the end of the week, the SHS exposure in outdoor hospitality venues might have been underestimated.
Despite the above limitations, this study includes the SHS exposure assessment in hospitality venues distributed across 11 European countries with different cultural, geographical, economic, and tobacco control contexts. For the environmental monitoring, we used airborne nicotine which is an objective and specific marker of SHS (Apelberg et al., 2013). Moreover, all countries shared a common protocol designed in accordance with a previously validated methodology (Hammond et al., 1987). Finally, the present analyses yield new insights regarding the main factors contributing to SHS concentrations on a set of highly frequented outdoor venues.
5. Conclusion
SHS exposure is still a relevant health hazard in outdoor hospitality venues across Europe. Our results show that smoking restrictions which draw on the degree of enclosure to forbid smoking are limited effective means to protect non-smokers. This study demonstrates there is a public health rationale behind totally banning smoking in the outdoor areas of hospitality venues. Moreover, considering the social component of the tobacco pandemic, a potential co-benefit of strong smoke-free policies in outdoor hospitality areas could be the denormalization of tobacco use in settings that are popular for smokers.
Funding
This project has received funding from the European Union's Horizon 2020 research and innovation program under grant agreement No 681040. The work of SG was partially supported by the Italian League Against Cancer (LILT, Milan). EF is partly supported by Ministry of Universities and Research, Government of Catalonia (2017SGR319) and by the Instituto Carlos III and co-funded by the European Regional Development Fund (FEDER) (INT16/00211 and INT17/00103), Government of Spain.
Credit author statement
Elisabet Henderson: Formal analysis, Writing – original draft, Visualization. Xavier Continente: Conceptualization, Investigation, Validation, Writing – review & editing. Esteve Fernández: Investigation, Writing – review & editing. Olena Tigova: Investigation, Writing – review & editing. Nuria Cortés-Francisco: Investigation, Writing – review & editing. Silvano Gallus: Investigation, Writing – review & editing. Alessandra Lugo: Investigation, Writing – review & editing. Sean Semple: Investigation, Writing – review & editing. Ruaraidh Dobson: Investigation, Writing – review & editing. Luke Clancy: Investigation, Writing – review & editing. Sheila Keogan: Investigation, Writing – review & editing. Ario Ruprecht: Investigation, Writing – review & editing. Alessandro Borgini: Investigation, Writing – review & editing. Anna Tzortzi: Investigation, Writing – review & editing. Vergina K Vyzikidou: Investigation, Writing – review & editing. Giuseppe Gorini: Investigation, Writing – review & editing. Angel López-Nicolás: Investigation, Writing – review & editing. Joan B Soriano: Investigation, Writing – review & editing. Gergana Geshanova: Investigation, Writing – review & editing. Joseph Osman: Investigation, Writing – review & editing. Ute Mons: Investigation, Writing – review & editing. Krzysztof Przewozniak: Investigation, Writing – review & editing. José Precioso: Investigation, Writing – review & editing. Ramona Brad: Investigation, Writing – review & editing. Maria J. López: Conceptualization, Investigation, Writing – review & editing, Project administration, Funding acquisition.
Disclaimer
This paper reflects only the authors’ views and the European Commission is not responsible for any use that may be made of the information it contains.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
1The TackSHS Project Investigators:
Catalan Institute of Oncology (ICO); Bellvitge Biomedical Research Institute (IDIBELL), Spain: Esteve Fernández, Yolanda Castellano, Marcela Fu, Montse Ballbè, Beladenta Amalia, Olena Tigova.
Public Health Agency of Barcelona (ASPB), Spain: Maria José López, Xavier Continente, Teresa Arechavala, Elisabet Henderson.
Istituto di Ricerche Farmacologiche Mario Negri IRCCS (IRFMN), Italy: Silvano Gallus, Alessandra Lugo, Xiaoqiu Liu, Elisa Borroni.
Istituto DOXA, Worldwide Independent Network/Gallup International Association, Italy: Paolo Colombo.
University of Stirling (UNISTIR), the UK: Sean Semple, Rachel O'Donnell, Ruaraidh Dobson.
TobaccoFree Research Institute Ireland (TFRI), Ireland: Luke Clancy, Sheila Keogan, Hannah Byrne.
Hellenic Cancer Society - George D. Behrakis Research Lab (HCS), Greece: Panagiotis Behrakis, Anna Tzortzi, Constantine Vardavas, Vergina Konstantina Vyzikidou, Gerasimos Bakelas, George Mattiampa.
Fondazione IRCCS Istituto Nazionale dei Tumori (INT), Italy: Roberto Boffi, Ario Ruprecht, Cinzia De Marco, Alessandro Borgini, Chiara Veronese, Martina Bertoldi, Andrea Tittarelli.
Istituto per lo Studio, la Prevenzione, e la Rete Oncologica (ISPRO), Italy: Giuseppe Gorini, Giulia Carreras, Barbara Cortini, Simona Verdi, Alessio Lachi, Elisabetta Chellini.
Polytechnic University of Cartagena (UPCT), Spain: Ángel López Nicolás, Marta Trapero-Bertran, Daniel Celdrán Guerrero.
European Network on Smoking and Tobacco Prevention (ENSP), Belgium: Cornel Radu-Loghin, Dominick Nguyen, Polina Starchenko.
Hospital Universitario La Princesa (IISP), Spain: Joan B Soriano, Julio Ancochea, Tamara Alonso, María Teresa Pastor, Marta Erro, Ana Roca, Patricia Pérez, Elena García Castillo.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2021.111355.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Apelberg B.J., Hepp L.M., Avila-Tang E., Gundel L., Hammond S.K., Hovell M.F., Hyland A., Klepeis N.E., Madsen C.C., Navas-Acien A., Repace J., Samet J.M., Breysse P.N. Environmental monitoring of secondhand smoke exposure. Tob. Control. 2013;22:147–155. doi: 10.1136/tobaccocontrol-2011-050301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arechavala T., Continente X., Pérez-Ríos M., Schiaffino A., Fernandez E., Cortés-Francisco N., Centrich F., Muñoz G., López M.J. Second-hand smoke exposure in homes with children: assessment of airborne nicotine in the living room and children’s bedroom. Tob. Control. 2018;27:399–406. doi: 10.1136/tobaccocontrol-2017-053751. [DOI] [PubMed] [Google Scholar]
- Cameron M., Brennan E., Durkin S., Borland R., Travers M.J., Hyland A., Spittal M.J., Wakefield M.A. Secondhand smoke exposure (PM2.5) in outdoor dining areas and its correlates. Tob. Control. 2010;19:19–23. doi: 10.1136/tc.2009.030544. [DOI] [PubMed] [Google Scholar]
- Chaiton M., Diemert L., Zhang B., Kennedy R.D., Cohen J.E., Bondy S.J., Ferrence R. Exposure to smoking on patios and quitting: a population representative longitudinal cohort study. Tob. Control. 2016;25:83–88. doi: 10.1136/tobaccocontrol-2014-051761. [DOI] [PubMed] [Google Scholar]
- Chan J., Burnett T., Baillie R., Blomfield S., Cameron-Christie P., Dickson J., Fleishl W., Ghandi S., Gordon K., Heo J., Kesy A., Kao A.Y., Kenny C., Knight A., Wilson N., Thomson G. Smoking in outdoor areas of bars and cafés: large differences between midday and evening prevalences. Drugs: Educ. Prev. Policy. 2014;21:484–488. doi: 10.3109/09687637.2014.917273. [DOI] [Google Scholar]
- Edwards R., Wilson N. Smoking outdoors at pubs and bars: is it a problem? An air quality study. N. Z.Med. J. 2011;124:27–37. [PubMed] [Google Scholar]
- Fernández E., Fu M., Pascual J.A., López M.J., Pérez-Ríos M., Schiaffino A., Martínez-Sánchez J.M., Ariza C., Saltó E., Nebot M., Spanish Smoking Law Evaluation Group Impact of the Spanish smoking law on exposure to second-hand smoke and respiratory health in hospitality workers: a cohort study. PloS One. 2009;4:e4244. doi: 10.1371/journal.pone.0004244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández E., López M.J., Gallus S., Semple S., Clancy L., Behrakis P., Ruprecht A., Gorini G., López-Nicolás Á., Radu-Loghin C., Soriano J.B., TackSHS Project Investigators Tackling second-hand exposure to tobacco smoke and aerosols of electronic cigarettes: the TackSHS project protocol. Gac. Sanit. 2020;34:77–82. doi: 10.1016/j.gaceta.2019.07.002. [DOI] [PubMed] [Google Scholar]
- Filippidis F.T., Agaku I.T., Girvalaki C., Jiménez-Ruiz C., Ward B., Gratziou C., Vardavas C.I., Tobacco Control Committee of the European Respiratory Society Relationship of secondhand smoke exposure with sociodemographic factors and smoke-free legislation in the European Union. Eur. J. Public Health. 2016;26:344–349. doi: 10.1093/eurpub/ckv204. [DOI] [PubMed] [Google Scholar]
- Flouris A.D., Vardavas C.I., Metsios G.S., Tsatsakis A.M., Koutedakis Y. Biological evidence for the acute health effects of secondhand smoke exposure. Am. J. Physiol. Lung Cell Mol. Physiol. 2010;298:L3–L12. doi: 10.1152/ajplung.00215.2009. [DOI] [PubMed] [Google Scholar]
- Fu M., Fernández E., Martínez-Sánchez J.M., San Emeterio N., Quirós N., Sureda X., Ballbè M., Muñoz G., Riccobene A., Centrich F., Saltó E., López M.J. Second-hand smoke exposure in indoor and outdoor areas of cafés and restaurants: need for extending smoking regulation outdoors? Environ. Res. 2016;148:421–428. doi: 10.1016/j.envres.2016.04.024. [DOI] [PubMed] [Google Scholar]
- Gallus S., Lugo A., Liu X., Behrakis P., Boffi R., Bosetti C., Carreras G., Chatenoud L., Clancy L., Continente X., Dobson R., Effertz T., Filippidis F.T., Fu M., Geshanova G., Gorini G., Keogan S., Ivanov H., Lopez M.J., Lopez-Nicolas A., Precioso J., Przewozniak K., Radu-Loghin C., Ruprecht A., Semple S., Soriano J.B., Starchenko P., Trapero-Bertran M., Tigova O., Tzortzi A.S., Vardavas C., Vyzikidou V.K., Colombo P., Fernández E., TackSHS Project Investigators Who smokes in Europe? Data from 12 European countries in the TackSHS survey (2017-2018) J. Epidemiol. 2021;31:145–151. doi: 10.2188/jea.JE20190344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn E.J. Smokefree legislation: a review of health and economic outcomes research. Am. J. Prev. Med. 2010;39(6 Suppl. 1):S66–S76. doi: 10.1016/j.amepre.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Hammond S.K., Leaderer B.P., Roche A.C., Schenker M. Collection and analysis of nicotine as a marker for environmental tobacco smoke. Atmos. Environ. 1987;21:457–462. doi: 10.1016/0004-6981(87)90027-8. [DOI] [Google Scholar]
- Henderson E., Continente X., Fernández E., Tigova O., Cortés-Francisco N., Gallus S., Lugo A., Semple S., O'Donnell R., Clancy L., Keogan S., Ruprecht A., Borgini A., Tzortzi A., Vyzikidou V.K., Gorini G., López-Nicolás A., Soriano J.B., Geshanova G., Osman J., Mons U., Przewozniak K., Precioso J., Brad R., López M.J., TackSHS project Investigators Secondhand smoke exposure and other signs of tobacco consumption at outdoor entrances of primary schools in 11 European countries. Sci. Total Environ. 2020;743:140743. doi: 10.1016/j.scitotenv.2020.140743. [DOI] [PubMed] [Google Scholar]
- Henderson E., Continente X., Fernández E., Tigova O., Cortés-Francisco N., Gallus S., Lugo A., Semple S., O'Donnell R., Clancy L., Keogan S., Ruprecht A., Borgini A., Tzortzi A., Vyzikidou V.K., Gorini G., López-Nicolás A., Soriano J.B., Geshanova G., Osman J., Mons U., Przewozniak K., Precioso J., Brad R., López M.J., TackSHS project investigators. Secondhand smoke exposure in outdoor children's playgrounds in 11 European countries. Environ Int Nov. 2020;20:105775. doi: 10.1016/j.envint.2020.105775. [DOI] [PubMed] [Google Scholar]
- Henderson E., Lugo A., Liu X., Continente X., Fernández E., López M.J., Gallus S., TackSHS project investigators. Corrigendum to “Secondhand smoke presence in outdoor areas in 12 European countries” [Environ. Res. 195 (2021) 110806] Environ Res. 2021 May 19;199:111337. doi: 10.1016/j.envres.2021.111337. Epub ahead of print. Erratum for: Environ Res. 2021 Apr; 195: 110806. [DOI] [PubMed] [Google Scholar]
- Joossens L., Raw M. 2016. The Tobacco Control Scale 2016 in Europe.https://www.tobaccocontrolscale.org/TCS2016.pdf [Google Scholar]
- Kennedy R.D., Behm I., Craig L., Thompson M.E., Fong G.T., Guignard R., Beck F. Outdoor smoking behaviour and support for outdoor smoking restrictions before and after France’s national smoking ban. Eur. J. Public Health. 2012;22(Suppl. 1):29–34. doi: 10.1093/eurpub/ckr208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy R.D., Elton-Marshall T., Mutti S., Dubray J., Fong G.T. Understanding the impact of the Smoke-Free Ontario Act on hospitality establishments’ outdoor environments: a survey of restaurants and bars. Tob. Control. 2010;19:165–167. doi: 10.1136/tc.2009.031872. [DOI] [PubMed] [Google Scholar]
- Keogan S., Alonso T., Sunday S., Tigova O., Fernández E., López M.J., Gallus S., Semple S., Tzortzi A., Boffi R., Gorini G., López-Nicolás Á., Radu-Loghin C., Soriano J.B., Clancy L., the TackSHS Project Investigators Lung function changes in patients with chronic obstructive pulmonary disease (COPD) and asthma exposed to secondhand smoke in outdoor areas. J. Asthma. 2020;22:1–7. doi: 10.1080/02770903.2020.1766062. [DOI] [PubMed] [Google Scholar]
- Lagerweij N.A., Kuipers M.A.G., Schreuders M., Grard A., Mlinarić M., Richter M., Leão T., Kinnunen J.M., Kunst A.E. The visibility of smoking in Europe and its relationship with youth’s positive beliefs about smoking. Int. J. Public Health. 2019;64:1335–1344. doi: 10.1007/s00038-019-01288-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licht A.S., Hyland A., Travers M.J., Chapman S. Secondhand smoke exposure levels in outdoor hospitality venues: a qualitative and quantitative review of the research literature. Tob. Control. 2013;22:172–179. doi: 10.1136/tobaccocontrol-2012-050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López M.J., Fernández E., Gorini G., Moshammer H., Polanska K., Clancy L., Dautzenberg B., Delrieu A., Invernizzi G., Muñoz G., Precioso J., Ruprecht A., Stansty P., Hanke W., Nebot M. Exposure to secondhand smoke in terraces and other outdoor areas of hospitality venues in eight European countries. PloS One. 2012;7 doi: 10.1371/journal.pone.0042130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López M.J., Fernández E., Pérez-Rios M., Martínez-Sánchez J.M., Schiaffino A., Galán I., Moncada A., Fu M., Montes A., Saltó E., Nebot M. Impact of the 2011 Spanish smoking ban in hospitality venues: indoor secondhand smoke exposure and influence of outdoor smoking. Nicotine Tob. Res. 2013;15:992–996. doi: 10.1093/ntr/nts218. [DOI] [PubMed] [Google Scholar]
- Lopez M.J., Nebot M., Albertini M., Birkui P., Centrich F., Chudzikova M., Georgouli M., Gorini G., Moshammer H., Mulcahy M., Pilali M., Serrahima E., Tutka P., Fernandez E. Secondhand smoke exposure in hospitality venues in Europe. Environ. Health Perspect. 2008;116:1469–1472. doi: 10.1289/ehp.11374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulcahy M., Evans D.S., Hammond S.K., Repace J.L., Byrne M. Secondhand smoke exposure and risk following the Irish smoking ban: an assessment of salivary cotinine concentrations in hotel workers and air nicotine levels in bars. Tob. Control. 2005;14:384–388. doi: 10.1136/tc.2005.011635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson A.L., Nutsford D., Thomson G. Measuring visual exposure to smoking behaviours: a viewshed analysis of smoking at outdoor bars and cafés across a capital city’s downtown area. BMC Public Health. 2014;14:300. doi: 10.1186/1471-2458-14-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peruga A., Molina X., Delgado I., Matute I., Olea A., Hirmas M., González C., Aguilera X. Compliance with the smoking ban in enclosed, semiopen and open areas of workplaces and public places in Chile. Tob Control Jul. 2020;23 doi: 10.1136/tobaccocontrol-2020-055632. tobaccocontrol-2020-055632. [DOI] [PubMed] [Google Scholar]
- Satterlund T.D., Lee J.P., Moore R.S. Changes in smoking-related norms in bars resulting from California's Smoke-Free Workplace Act. J. Drug Educ. 2012;42:315–326. doi: 10.2190/DE.42.3.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford J., Daube M., Franklin P. Second hand smoke in alfresco areas. Health Promot. J. Aust. 2010;21:99–105. doi: 10.1071/he10099. [DOI] [PubMed] [Google Scholar]
- St.Helen G., Bernert J.T., Hall D.B., Sosnoff C.S., Xia Y., Balmes J.R., Vena J.E., Wang J.S., Holland N.T., Naeher L.P. Exposure to secondhand smoke outside of a bar and a restaurant and tobacco exposure biomarkers in nonsmokers. Environ. Health Perspect. 2012;120:1010–1016. doi: 10.1289/ehp.1104413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sureda X., Bilal U., Fernández E., Valiente R., Escobar F.J., Navas-Acien A., Franco M. Second-hand smoke exposure in outdoor hospitality venues: smoking visibility and assessment of airborne markers. Environ. Res. 2018;165:220–227. doi: 10.1016/j.envres.2018.04.024. [DOI] [PubMed] [Google Scholar]
- Sureda X., Fernández E., López M.J., Nebot M. Secondhand tobacco smoke exposure in open and semi-open settings: a systematic review. Environ. Health Perspect. 2013;121:766–773. doi: 10.1289/ehp.1205806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sureda X., Fernández E., Martínez-Sánchez J.M., Fu M., López M.J., Martínez C., Saltó E. Secondhand smoke in outdoor settings: smokers' consumption, non-smokers’ perceptions, and attitudes towards smoke-free legislation in Spain. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-007554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotter L., Wakefield M., Borland R. Socially cued smoking in bars, nightclubs, and gaming venues: a case for introducing smoke-free policies. Tob. Control. 2002;11:300–304. doi: 10.1136/tc.11.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2006. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General.https://www.ncbi.nlm.nih.gov/books/NBK44324/pdf/Bookshelf_NBK44324.pdf [Google Scholar]
- Valiente R., Escobar F., Pearce J., Bilal U., Franco M., Sureda X. Mapping the visibility of smokers across a large capital city. Environ. Res. 2020;180:108888. doi: 10.1016/j.envres.2019.108888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Beek K.N.J., Kuipers M.A.G., Lignac O., Kunst A.E. Smoking in bars in eight European countries in 2010 and 2016: an observational comparative study. Eur. J. Public Health. 2019;29:159–163. doi: 10.1093/eurpub/cky111. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2007. Media center. News releases 2007.https://www.who.int/mediacentre/news/releases/2007/pr26/en/ [Google Scholar]
- World Health Organization . 2017. Tobacco and its Environmental Impact: an overview.https://www.who.int/tobacco/publications/environmental-impact-overview/en/ [Google Scholar]
- World Health Organization Regional Office for Europe . 2019. Tobacco Control Playbook.https://www.euro.who.int/__data/assets/pdf_file/0011/395687/Tobacco-Control-Playbook-final.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.