FIGURE 1.
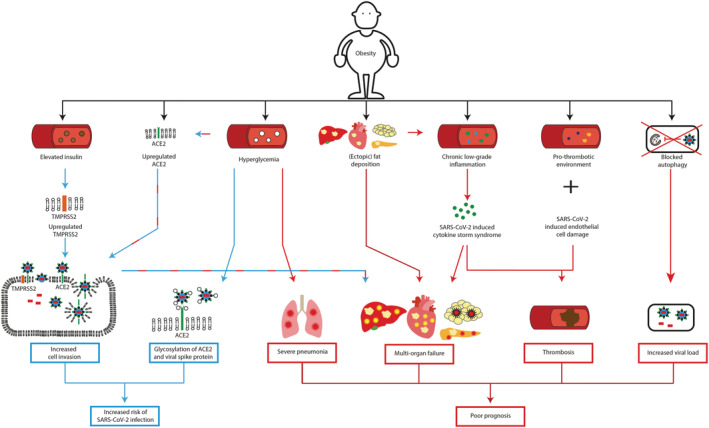
Obesity increases the risk of SARS‐CoV‐2 infection and leads to poorer prognosis. Blue arrows: Mechanisms contributing to increased SARS‐CoV‐2 infection risk in patients with obesity. Red arrows: Mechanisms contributing to poorer prognosis of COVID‐19 patients with obesity. In patients with obesity, elevated insulin levels upregulates TMPRSS2 expression, which in combination with overexpression of ACE2 increases SARS‐CoV‐2 cell invasion. Hyperglycemia increases ACE2 expression and potentially changes the glycosylation of ACE2 and the viral spike protein S, altering binding of S to ACE2. Together, these factors contribute to an increased risk of SARS‐CoV‐2 infection in patients with obesity. Hyperglycemia compromises the immune response in the lungs and may contribute to lung inflammation. Overexpression of ACE2 increases SARS‐CoV‐2 viral cell entry. Intracellularly, the virus induces cellular damage in adipose, heart, pancreas, and liver cells. In obesity, the organ function of the adipose tissue, heart, pancreas and liver is already affected due to (ectopic) fat deposition. SARS‐CoV‐2 can aggravate organ damage and thus contribute to multi‐organ failure. Chronic low‐grade inflammation, as observed in obesity, potentially facilitates the cytokine storm induced by SARS‐CoV‐2 consequently, extremely high levels of pro‐inflammatory cytokines, enhance cellular damage and eventually induce multi‐organ failure. Obesity is associated by a pro‐thrombotic environment. SARS‐CoV‐2 induces endothelial cell damage. In combination with the cytokine storm induced by SARS‐CoV‐2 this increases the risk of thrombosis in COVID‐19 patients with obesity. SARS‐CoV‐2 might block autophagy, resulting in decreased viral clearance. The disrupted autophagy process in obesity potentially further reduces SARS‐CoV‐2 clearance and by extension increases viral load. Together, these mechanisms lead to poorer prognosis of patients with obesity infected with SARS‐CoV‐2. ACE2, Angiotensin‐converting enzyme 2; TMPRSS2, transmembrane protease serine 2
