Summary
The national lockdown imposed in several countries to counteract the coronavirus disease 2019 (COVID‐19) pandemic led to an unprecedented situation with serious effects on mental health of the general population and of subjects affected by heterogeneous diseases. Considering the positive association between narcoleptic symptoms and creativity, we aimed at exploring the psychological distress associated with COVID‐19 restrictions and its relationship with depressive symptoms and creativity in patients with narcolepsy type 1 (NT1). A total of 52 patients with NT1 and 50 healthy controls, who completed a previous study on creativity, were contacted during the first lockdown period to complete an online survey evaluating psychological distress related to the COVID‐19 outbreak, sleep quality, narcolepsy and depressive symptoms, and creative abilities. The patients with NT1 showed an improvement in subjective sleepiness while controls reported worsening of sleep quality during the lockdown. Depression and NT1 symptom severity proved significant predictors of COVID‐19‐related distress. Creative performance, namely generative fluency, turned out to be a favourable moderator in the relationship between depression and patients’ distress, reducing the detrimental effect of depression on the patients’ wellbeing. On the contrary, creative originality proved to be a disadvantageous moderator in the relationship between NT1 symptom severity and the distress associated with this traumatic event indicating a higher vulnerability to developing COVID‐19‐related distress, particularly evident in patients displaying higher originality. Overall, these results highlight a crucial role of creativity in patients with NT1, suggesting that creative potential could be used as a protective factor against the development of distress associated with the lockdown.
Keywords: COVID‐19, creativity, depression, distress, narcolepsy
1. INTRODUCTION
Narcolepsy type 1 (NT1) is a chronic neurological disease characterised by excessive daytime sleepiness (EDS), clinical phenomena related to wake/rapid eye movement (REM) sleep dissociation (cataplexy, sleep paralysis, hypnagogic/hypnopompic hallucinations, and REM sleep behaviour disorder) and disrupted nocturnal sleep (International Classification of Sleep Disorders Third Edition, [ICSD‐3] American Academy of Sleep Medicine, 2014). Narcolepsy negatively impacts on quality of life and patients with NT1 consistently show increased risk of anxiety and mood disorders (Filardi et al., 2017; Fortuyn et al., 2010; Vignatelli et al., 2011; Zamarian et al., 2015). Nonetheless, patients with narcolepsy show a high creative potential (in terms of creative profile and creative achievement) and creative performance (Lacaux et al., 2019), which have been related to core NT1 symptoms such as sleep‐related hallucination (D'Anselmo et al., 2020) and lucid dreaming (Lacaux et al., 2019).
At the beginning of 2020, the coronavirus disease 2019 (COVID‐19) pandemic forced several countries to impose a national lockdown. This unprecedented situation had a serious impact on mental health, psychological distress, and sleep quality in the general population (Benke et al., 2020; Davico et al., 2021; Di Nicola et al., 2020; Franceschini et al., 2020; Huang & Zhao, 2020; Wang et al., 2020). Moreover, a detrimental impact of the COVID‐19 restrictions has been reported also in subjects with acute and chronic pathologies (Barutcu Atas et al., 2021; González‐Blanco et al., 2020). In the field of narcolepsy a handful of studies have assessed the effect of the COVID‐19 restrictions in both adult patients, who displayed an improvement in subjective sleepiness when working/studying at home during the lockdown (Postiglione et al., 2021), and in NT1 children and adolescents, who contrariwise did not show changes in subjective sleepiness or objective sleep quality (Filardi et al., 2021). However, these results are not replicated in a study comprising both patients with NT1 and NT2, where a little over half of the sample reported worsening of subjective sleepiness, increase in nocturnal awakening, and reduction in quality of life during the COVID‐19 pandemic (Rodrigues Aguilar et al., 2021).
Intriguingly, very recent studies have shown that creativity acts as a mitigating factor of the detrimental effects of COVID‐19 restrictions on wellbeing (Tang et al., 2021; Ying et al., 2020) in healthy subjects. Considering these findings and the tight relationship between creativity and narcolepsy, in the present study we aimed at exploring whether NT1 patients’ creative abilities could affect patients’ wellbeing during the first Italian generalised lockdown (in the period starting from March 10 until May 17, 2020; Government of Italy, 2020).
2. MATERIALS AND METHODS
2.1. Participants
From June to November 2019 we enrolled a group of patients with NT1 and age‐ and sex‐matched healthy controls for a study on creativity in narcolepsy (D'Anselmo et al., 2020). The patients with NT1 were recruited at the Centre for Narcolepsy in Bologna during routine outpatient follow‐up; the healthy controls were an age‐ and sex‐matched group recruited from relatives and accompanying persons of the patients with NT1 visiting the centre, from university students, and through personal contacts. All patients had a previous diagnosis of NT1 (ICSD‐3 American Academy of Sleep Medicine, 2014). Inclusion criteria were age ≥18 years and absence of comorbid neurological and/or psychiatric disorders. Healthy controls were recruited after excluding excessive daytime sleepiness, poor sleep quality, and depression (Epworth Sleepiness Scale [ESS] >11, Pittsburgh Sleep Quality Index [PSQI] >5, and Beck Depression Inventory [BDI] >20). During the first Italian national lockdown (April 22–May 17, 2020), the same participants were invited to take part in an online survey. A totalof 52 out of the 66 patients (mean [SD] age of 33.56 [11.59] years, 31 female) completed the survey. All patients were on stable pharmacological treatment (63% on monotherapy and 37% on pharmacological polytherapy). The final sample of healthy controls comprised 50 participants, out of 65 contacted (mean [SD] age of 34.42 [15.11] years, 36 female).
The study was carried out in accordance with the principles of the Declaration of Helsinki and approved by the local ethics committee (Comitato Etico Indipendente di Area Vasta Emilia Centro ‐ CE‐AVEC ‐ Prot. N.66930).
2.2. Measures
The presence and severity of narcolepsy symptoms were evaluated, in the NT1 sample, with the Narcolepsy Severity Scale (NSS) (Dauvilliers et al., 2017). Subjective sleep quality was assessed, in healthy controls, using the PSQI (Curcio et al., 2013). Subjective sleepiness was assessed with the ESS (Vignatelli et al., 2003). Creative activities were measured with a short version of the Creative Activity and Accomplishment Checklist (CAAC) (Runco et al., 1987), in which participants have to report the frequency with which they performed creative activities (in the artistic, technological, and everyday creative domains; Agnoli et al., 2016) during the lockdown. For each item the response was given by participants on a 4‐point Likert scale (“never did it”; “did it once or twice”; “3–5 times” and “more than 5 times”). Creative abilities were assessed in terms of divergent thinking (Runco & Acar, 2012), with the Alternative Use Test (AUT) (Guilford, 1967). Participants were asked to produce as many as possible uncommon/original uses for six common objects (e.g. a book, a chair). Two indexes have been computed: (a) fluency (number of alternative ideas produced by the participant) and (b) ideas originality (as scored by two independent, external raters; Silvia et al., 2008). COVID‐19‐related psychological distress was assessed using the 22‐item Impact of Event Scale‐Revised scale (IES‐R) (Weiss, 2007). This scale measures the subjective distress caused by traumatic events (three subscales: “intrusion”, “avoidance”, and “hyperarousal”). Participants were asked to rate the level of distress with specific reference to the COVID‐19 outbreak. Finally, depressive symptoms were assessed using the BDI (Beck et al., 1961).
2.3. Procedure
In the pre‐lockdown session, all participants completed a computerised version of the AUT and completed the ESS, NSS, and BDI. Healthy controls also completed the PSQI. In the lockdown session online versions of questionnaires (ESS, NSS, CAAC and IES) were administered through “PsyToolkit” (Stoet, 2017). Healthy controls completed the PSQI in the lockdown session.
2.4. Statistics
Data were explored with descriptive statistics (mean ± SD). Differences in NSS, ESS, PSQI scores before and during the lockdown period were assessed by means of paired sample t tests. A set of Pearson correlation analyses was conducted to assess the relationship between the measures of creativity (creative activities, AUT fluency, and AUT originality), distress (IES), and clinical data (NSS, ESS, BDI). Finally, to assess whether creative ability interacts with depression (BDI) and narcolepsy symptom severity (NSS) in the prediction of distress during the lockdown (IES) we conducted hierarchical multiple regressions including five blocks of variables (Table 3). AUT fluency and AUT originality were included in two distinct models. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS®) version 26 (SPSS, Inc. Chicago, IL, USA). An alpha level < 0.05 was considered statistically significant.
TABLE 3.
Hierarchical multiple regression of the relation between Beck Depression Inventory, Narcolepsy Severity Scale and creative abilities (fluency and originality) in the prediction of the Impact of Event Scale in patients with narcolepsy type 1 and in healthy controls
| IES | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patients with NT1 | Healthy controls | |||||||||
| Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | |
| A | ||||||||||
| BDI | 0.36* | 0.20 | 0.20 | 0.19 | 0.18 | 0.33* | 0.30 | 0.29 | 0.32 | 0.38 |
| NSS | 0.32* | 0.31 | 0.35 | 0.35 | 0.11 | 0.11 | 0.10 | 0.10 | ||
| AUT fluency | 0.11 | 0.02 | 0.04 | −0.08 | −0.07 | −0.07 | ||||
| AUT fluency × BDI | −0.29* | −0.33 | 0.04 | 0.18 | ||||||
| AUT fluency × NSS | 0.11 | −0.26 | ||||||||
| R2 | 0.11 | 0.17 | 0.16 | 0.22 | 0.21 | 0.09 | 0.08 | 0.07 | 0.04 | 0.08 |
| ΔR2 | 0.13* | 0.08* | 0.01 | 0.07* | 0.01 | 0.11* | 0.01 | 0.01 | 0.00 | 0.05 |
| F | 6.55* | 5.58* | 3.90* | 4.22* | 3.42* | 5.63* | 3.04 | 2.09 | 1.55 | 1.83 |
| ΔF | 6.55* | 4.14* | 0.62 | 4.27* | 0.46 | 5.63* | 0.52 | 0.28 | 0.05 | 2.72 |
| df | 44 | 43 | 42 | 41 | 40 | 46 | 45 | 44 | 43 | 42 |
| B | ||||||||||
| BDI | 0.36* | 0.20 | 0.19 | 0.19 | 0.26 | 0.33* | 0.30 | 0.30 | 0.32 | 0.33 |
| NSS | 0.32* | 0.30 | 0.30 | 0.25 | 0.11 | 0.11 | 0.09 | 0.09 | ||
| AUT originality | 0.08 | 0.07 | 0.16 | 0.01 | 0.06 | 0.08 | ||||
| AUT originality × BDI | −0.00 | −0.27 | 0.09 | 0.09 | ||||||
| AUT originality × NSS | 0.41* | −0.04 | ||||||||
| R2 | 0.11 | 0.17 | 0.16 | 0.13 | 0.21 | 0.09 | 0.08 | 0.06 | 0.04 | 0.02 |
| ΔR2 | 0.13* | 0.08* | 0.01 | 0.00 | 0.09* | 0.11* | 0.01 | 0.00 | 0.01 | 0.00 |
| F | 6.56* | 5.58* | 3.74* | 2.74* | 3.38* | 5.63* | 3.04 | 1.98 | 1.52 | 1.20 |
| ΔF | 6.56* | 4.14* | 0.25 | 0.00 | 4.90* | 5.63* | 0.52 | 0.00 | 0.25 | 0.02 |
| df | 44 | 43 | 42 | 41 | 40 | 46 | 45 | 44 | 43 | 42 |
AUT, Alternative Use Test; BDI, Beck Depression Inventory; IES, Impact of Event Scale; NSS, Narcolepsy Severity Scale total score; NT1, narcolepsy type 1.
A) Step 1: BDI; Step 2: NSS; Step 3: AUT fluency; Step 4: AUT fluency × BDI; Step 5: AUT fluency × NSS. B) Step 1: BDI; Step 2: NSS; Step 3: AUT originality; Step 4: AUT originality × BDI; Step 5: AUT originality × NSS. Numbers in the first four rows represent standardised regression coefficients; *p < 0.05.
3. RESULTS
Demographic, clinical data and questionnaires’ scores are reported in Table 1.
TABLE 1.
Demographic, sleep, clinical characteristics, and Psychological impact in the patients with narcolepsy type 1 and controls
| Variable | Patients with NT1 (n = 52) | Controls (n = 50) |
|---|---|---|
| Demographic data | ||
| Male/female, n | 14/36 | 21/31 |
| Age, years, mean±(SD) | 33.56 ± (11.59) | 34.42 ± (15.11) |
| Education, years, mean±(SD) | 13.50 ± (3.31) | 14.42 ± (3.31) |
| Age at diagnosis, years, mean (SD) | 17.06 ± (10.29) | |
| Disease duration, years, mean (SD) | 17.90 ± (10.62) | |
| Medication used, n | ||
| Stimulants | 14 | |
| Sodium oxybate | 19 | |
| Antidepressant | 9 | |
| Stimulants plus sodium oxybate | 19 | |
| Sleepiness, sleep quality and clinical characteristics | ||
|
ESS, mean (SD) Pre During P |
_ 11.28 ± (4.53) 9.85 ± (4.50) 0.04* |
_ 5.29 ± (2.79) 5.31 ± (3.04) 0.96 |
|
PSQI, mean (SD) Pre During P |
_ 4.26 (2.25) 5.34 ± (2.88) 0.01* |
|
|
SP‐H (NSS), mean (SD) Pre During p |
_ 4.17 ± (4.32) 4.23 ± (4.54) 0.90 |
|
|
EDS‐NS (NSS), mean (SD) Pre During p |
_ 13.25 ± (5.87) 10.79 ± (5.46) 0.00* |
|
|
CATA (NSS), mean (SD) Pre During P |
_ 5.38 ± (3.94) 5.10 ± (3.81) 0.55 |
|
|
NSS, mean (SD) Pre During P |
_ 22.81 ± (11.12) 20.12 ± (10.26) 0.01* |
|
| Psychological impact IES‐R, mean (SD) | ||
| Total score | 5.87 ± (1.91) | 6.29 ± (1.99) |
| Intrusion | 1.83 ± (0.66) | 1.95 ± (0.74) |
| Avoidance | 2.00 ± (0.67) | 2.14 ± (0.68) |
| Hyperarousal | 2.05 ± (0.82) | 2.20 ± (0.78) |
CATA, cataplexy; EDS‐NS, excessive daytime sleepiness and night‐time sleep; ESS, Epworth Sleepiness Scale; NSS, Narcolepsy Severity Scale total score; NT1, narcolepsy type 1; PSQI, Pittsburgh Sleep Quality Index; SP‐H, Sleep paralysis and hypnagogic hallucinations.
*p < 0.05
The patients with NT1 showed significant improvement in sleepiness (ESS pre > ESS during; p = 0.04) and in the factors “excessive daytime sleepiness and nocturnal sleep” of the NSS (EDS‐NS pre > EDS‐NS during; p < 0.001). The control group showed a significant deterioration of sleep quality during lockdown (PSQI pre < PSQI during; p = 0.01). Controls also showed a delay in bedtime (~40 min, mean [SD] pre = 23.30 [1.00] and during = 24.10 [1.25], p < 0.001) and wake‐up time (~36 min, mean [SD] pre = 7.39 [1.30] and during = 8.15 [1.24], p < 0.001) but not in the time in bed (TIB) before and during lockdown (mean [SD] pre = 8.02 [1.18] and during = 8.06 [1.07], p = non‐significant).
Results of correlation analyses are reported, separately for each group, in Table 2.
TABLE 2.
Descriptive statistics and correlations among the study variables in the patients with narcolepsy type 1 and healthy controls
| Patients with NT1 | ||||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| 1 | CAAC | _ | ||||||
| 2 | Fluency | 0.51** | _ | |||||
| 3 | Originality | 0.19 | 0.44** | _ | ||||
| 4 | IES | 0.43** | 0.15 | 0.24 | _ | |||
| 5 | NSS | 0.24 | 0.12 | 0.36* | 0.36** | _ | ||
| 6 | ESS | −0.07 | 0.08 | 0.08 | 0.01 | 0.52** | _ | |
| 7 | BDI | 0.12 | 0.03 | 0.28 | 0.35* | 0.56** | 0.31* | _ |
| Mean | 1.54 | 25.33 | 2.25 | 5.87 | 22.81 | 11.28 | 9.50 | |
| SD | 0.34 | 11.15 | 0.26 | 1.91 | 11.12 | 4.53 | 9.00 | |
| Healthy controls | |||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| 1 | CAAC | _ | |||||
| 2 | Fluency | −0.09 | _ | ||||
| 3 | Originality | 0.15 | 0.24 | _ | |||
| 4 | IES | 0.25 | −0.15 | 0.03 | _ | ||
| 5 | ESS | 0.10 | −0.12 | 0.02 | −0.04 | _ | |
| 6 | BDI | 0.16 | −0.10 | −0.03 | 0.33* | −0.20 | _ |
| Mean | 1.63 | 32.08 | 2.26 | 6.29 | 5.29 | 6.96 | |
| SD | 0.414 | 15.46 | 0.25 | 1.99 | 2.79 | 7.16 | |
BDI, Beck Depression Inventory; CAAC, Creative achievement; EES, Epworth Sleepiness Scale; IES, Impact of Event Scale; NSS, Narcolepsy Severity Scale total score; NT1, narcolepsy type 1.
p < 0.05, p < 0.01.
In NT1 BDI was positively correlated with NSS‐pre (r = 0.31), ESS‐pre (r = 0.56), and IES (r = 0.35) (all p < 0.037). Moreover, the NSS‐pre was positively correlated with ESS‐pre (r = 0.52), AUT originality (r = 0.36), and IES (r = 0.36) (all p < 0.013). AUT fluency was positively correlated with AUT originality (r = 0.44, p = 0.002). Creative activity was positively correlated with IES (r = 0.43) and AUT fluency (r = 0.51) (all p < 0.001). No significant direct association emerged between IES and the creativity indexes in the AUT task, originality (r = 0.24) and fluency (r = 0.14).
Two separate hierarchical multiple regressions were performed on patients with NT1 including AUT fluency and AUT originality as indices of creative abilities. Both analyses revealed that BDI and NSS‐pre are significant predictors of IES during lockdown in patients with NT1. The interaction effect (BDI × AUT fluency) highlighted a significant moderation (ΔR 2 = 0.07, p < 0.05) by the latter on the detrimental effect of BDI on NT1 patients’ COVID‐19‐related distress (Table 3‐A). A simple slope analysis showed that BDI predicts IES at low level of AUT fluency (ß = 0.14, SE = 0.06, p = 0.02), but not at medium (ß = 0.04, SE = 0.03, p = 0.23), and high levels (ß = −.06, SE = 0.06, p = 0.33) (Figure 1). Therefore, the relationship between BDI and IES is moderated by AUT fluency.
FIGURE 1.
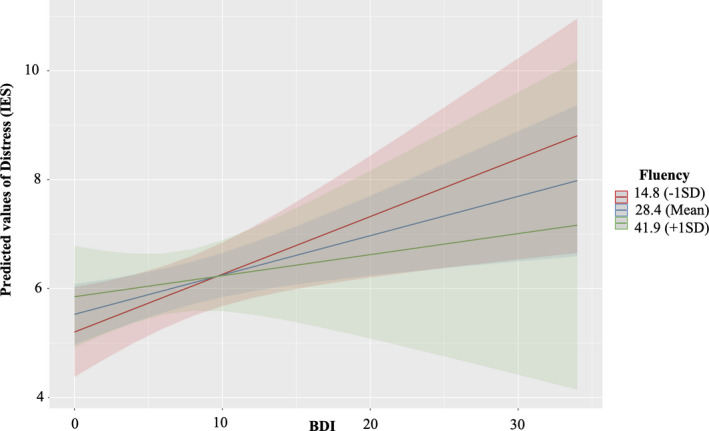
Moderating effect of creative abilities (Alternative Use Test [AUT] fluency) on depression (Beck Depression Inventory [BDI]) in the prediction of distress (Impact of Event Scale [IES]) during quarantine period in patients with narcolepsy type 1 (NT1). The figure shows the significant effect of BDI in the prediction of IES, which emerged at low level of AUT fluency (red line), but not at medium (blue line) and high levels (green line). Shaded areas denote 95% confidence intervals [Colour figure can be viewed at wileyonlinelibrary.com]
Regarding AUT originality, the interaction effect (BDI × AUT originality) was not statistically significant in the prediction of IES; nevertheless, the interaction NSS‐pre × AUT originality produced a significant change in the model, ΔR 2 = 0.09, p<0.05 (Table 3‐B). A simple slope analysis (Figure 2) showed that NSS‐pre predicts IES only at high level of AUT originality (ß = 0.12, SE = 0.04, p = 0.01), but not at medium (ß = 0.05, SE = 0.03, p = 0.12), and low levels (ß = −0.02, SE = 0.05, p = 0.63). Therefore, the relationship between NSS and IES is moderated by AUT originality.
FIGURE 2.
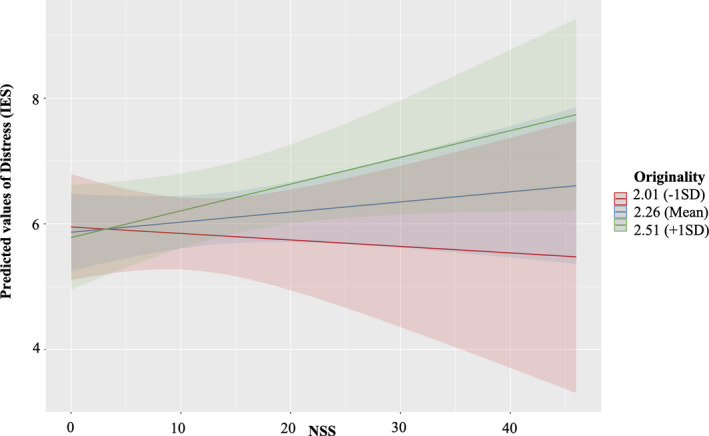
Moderating effect of creative abilities (AUT originality) on narcolepsy severity (NSS) in the prediction of distress (IES) during quarantine period in NT1 patients. The figure shows the significant effect of NSS in the prediction of IES, which emerged at high level of AUT originality (green line), but not at medium (blue line) and low levels (red line). Shaded areas denote 95% confidence intervals [Colour figure can be viewed at wileyonlinelibrary.com]
The same set of hierarchical regressions was performed on the control group. Both analyses revealed that only BDI was a significant predictor of IES during lockdown; the interaction effects between BDI and AUT (fluency or originality) and between NSS‐pre and AUT (fluency or originality) did not significantly increase the variance explained by the model (Table 3).
4. DISCUSSION
The present study explored whether creativity could mitigate the psychological distress related to the COVID‐19 lockdown in patients with NT1. The main findings concern the role of NT1 patients’ creative potential in influencing the vulnerability to this stressful situation. Moreover, the present study also expanded our knowledge on the impact of home confinement on NT1 patients’ symptom severity.
During the lockdown patients with NT1 reported a significant decrease in daytime sleepiness in parallel to a significant improvement in symptom severity, particularly excessive daytime sleepiness, and nocturnal sleep disruption. On the other hand, healthy controls reported a shift in wake/sleep timing and worsening of sleep quality. These results are consistent with previous findings on the impact of COVID‐19 restrictions in patients with narcolepsy (Filardi et al., 2021; Rodrigues Aguilar et al., 2021; Postiglione et al., 2021; Wu et al., 2021) and in the general population (Cellini et al., 2020; Franceschini et al., 2020). We may speculate that the improvement in symptoms (namely daytime sleepiness and night‐time sleep) in patients with narcolepsy may be also due to the greater possibility of self‐management of their sleep/wake and working schedules.
Interestingly, we demonstrated a multifaceted effect of the creative potential on the distress related to the COVID‐19 outbreak. This effect appears to strongly depend on the different creative abilities measured before the COVID‐19 outbreak, namely generative fluency (ability to find alternative responses to an ill‐defined problem) and originality (ability to generate original solutions to the same problems). These findings confirm that creative thinking can be considered a skill that fosters a positive attitude and in turn may improve mental health when challenging circumstances occur (Forgeard, 2013). Moreover, correlational analyses showed that the level of distress is positively associated with the frequency of creative activities performed during the lockdown. Again, this result suggests that patients with NT1 may use creative activities to react to psychological distress. Creativity has been indeed associated with an adaptive prospection, (Kashdan & Rottenberg, 2010), especially when it is applied to everyday activities, promoting a psychologically healthy state that fosters personal growth (Kaufman, 2018). Noteworthy, depressive symptoms are quite common in narcolepsy (Zamarian et al., 2015) and, interestingly, the results of the present study suggest a complex interplay between depression/depressive symptoms and creativity, which did not emerge in the controls.
By contrast creative performance, evaluated in terms of originality, displays a negative impact on the relationship between symptom severity and COVID‐19 distress. In more detail, patients with NT1 who had more severe symptoms proved more vulnerable to developing distress during the lockdown, when they showed higher originality. Consistent with previous studies (Lacaux et al., 2019; D'Anselmo et al., 2020), we found that higher NSS levels are associated with a higher ability to generate original contents.
While narcolepsy negatively affects patients’ quality of life (Vignatelli et al., 2011), creativity seems to represent an enhanced cognitive domain (Lacaux et al., 2019). Indeed, patients with NT1 have in the expression of their creative potential a wellbeing window through which to realise their identity (D'Anselmo et al., 2020). We might speculate that the unprecedented situation of home‐confinement may have restricted the occasions of expression of patients’ creative potential, and in particular of their ability to produce original contents; this restriction might have in turn increased the distress associated with the COVID‐19 situation. Noteworthy, a recent study showed that healthy participants with high‐base creativity prior to the lockdown emerged to be particularly affected by these circumstances (Mercier et al., 2021).
Overall, our present results indicate a different role for creativity in relation to the lockdown situation between patients with NT1 and controls. Compared to healthy controls, in patients with NT1 creativity seems to show a strong relationship with depression and with narcolepsy symptoms in predicting the distress associated with the lockdown. Therefore, creativity appears to be a double‐edged skill in home‐confined patients with NT1, as it represents an intrinsic feature of their personal identity: creative potential both offered a protective factor against the detrimental effect of depression and induced a higher level of distress as it cannot be fully expressed due to restrictions related to the lockdown situation.
One limitation that should be considered in the present study is that a direct causality between measures of creativity and the level of distress associated within the lockdown period can not be established. Nevertheless, unlike previous studies, in the present study we collected an overall assessment of symptom severity (NSS) in patients with NT1 with repeated measurements (before and during the lockdown).
In conclusion, creativity in NT1 seems to be a factor to be taken into consideration in order to foster the ability to cope with highly stressful situations in these patients and to promote their wellbeing. We can indeed infer that these findings could be extended to other stressful situations, which can give rise to distress. However, other studies in this field are needed in order to generalise the findings emerging from the present study. Based on the results of the present study, we would in particular suggest developing ad hoc behavioral interventions in patients with NT1 in order to foster specific creative abilities. The efficacy of training interventions in increasing creative abilities and attitudes has already been demonstrated in the healthy population (Scott et al., 2004; Tsai, 2013). We might hypothesise that greater awareness and control over their creative abilities could act in patients with NT1 as mitigating factors for the arising of psychopathological conditions associated with stressful situations.
CONFLICT OF INTEREST
GP participated in advisory board for Jazz pharmaceuticals, Bioprojet, Takeda and Idorsia outside the submitted work. The other authors have no potential financial conflict of interest to disclose.
AUTHOR CONTRIBUTIONS
AD: conception of the study, statistical analysis, interpretation of data, drafting the initial manuscript and revising it for important intellectual content. SA: conception of the study, statistical analysis, interpretation of data, drafting the initial manuscript and revising it for important intellectual content. MF: acquisition of data, interpretation of data, reviewed the manuscript for intellectual content. FP: interpretation of data, reviewed the manuscript for intellectual content. SM: interpretation of data, reviewed the manuscript for intellectual content. GEC: interpretation of data, reviewed the manuscript for intellectual content. GP: conception of the study, study supervision, drafting the initial manuscript and revising it for important intellectual content.
ACKNOWLEDGMENTS
We are indebted to all the patients participating in this study, most notably the Italian Association of Narcolepsy (AIN onlus) patients. Without their contributions, this study would not have been possible. We also thank Cecilia Baroncini for editing the English text.
D’Anselmo, A. , Agnoli, S. , Filardi, M. , Pizza, F. , Mastria, S. , Corazza, G. E. , & Plazzi, G. (2022). Being creative during lockdown: The relationship between creative potential and COVID‐19‐related psychological distress in narcolepsy type 1. Journal of Sleep Research, 31, e13461. 10.1111/jsr.13461
Anita D’Anselmo and Sergio Agnoli contributed equally.
Contributor Information
Anita D’Anselmo, Email: anita.danselmo@unibo.it.
Sergio Agnoli, Email: sergio.agnoli@unibo.it.
DATA AVAILABILITY STATEMENT
Data are available from the corresponding author upon reasonable request.
REFERENCES
- Agnoli, S. , Corazza, G. E. , & Runco, M. A. (2016). Estimating creativity with a multiple‐measurement approach within scientific and artistic domains. Creativity Research Journal, 28(2), 171–176. 10.1080/10400419.2016.1162475 [DOI] [Google Scholar]
- American Academy of Sleep Medicine (2014). International Classification of Sleep Disorders, Third Edition. American Academy of Sleep Medicine. [Google Scholar]
- Barutcu Atas, D. , Aydin Sunbul, E. , Velioglu, A. , & Tuglular, S. (2021). The association between perceived stress with sleep quality, insomnia, anxiety and depression in kidney transplant recipients during Covid‐19 pandemic. PLoS One, 16(3), e0248117. 10.1371/journal.pone.0248117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. T. , Ward, C. H. , Mendelson, M. , Mock, J. , & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571. 10.1001/archpsyc.1961.01710120031004 [DOI] [PubMed] [Google Scholar]
- Benke, C. , Autenrieth, L. K. , Asselmann, E. , & Pané‐Farré, C. A. (2020). Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID‐19 pandemic among adults from Germany. Psychiatry Research, 293, 113462. 10.1016/j.psychres.2020.113462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini, N. , Canale, N. , Mioni, G. , & Costa, S. (2020). Changes in sleep pattern, sense of time and digital media use during COVID‐19 lockdown in Italy. Journal of Sleep Research, 29(4), e13074. 10.1111/jsr.13074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curcio, G. , Tempesta, D. , Scarlata, S. , Marzano, C. , Moroni, F. , Rossini, P. M. , Ferrara, M. , & De Gennaro, L. (2013). Validity of the Italian version of the Pittsburgh sleep quality index (PSQI). Neurological Sciences, 34(4), 511–519. 10.1007/s10072-012-1085-y [DOI] [PubMed] [Google Scholar]
- D'Anselmo, A. , Agnoli, S. , Filardi, M. , Pizza, F. , Mastria, S. , Corazza, G. E. , & Plazzi, G. (2020). Creativity in narcolepsy type 1: The role of dissociated REM sleep manifestations. Nature and Science of Sleep, 12, 1191. 10.2147/NSS.S277647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauvilliers, Y. , Beziat, S. , Pesenti, C. , Lopez, R. , Barateau, L. , Carlander, B. , Luca, G. , Tafti, M. , Morin, C. M. , Billiard, M. , & Jaussent, I. (2017). Measurement of narcolepsy symptoms: the narcolepsy severity scale. Neurology, 88(14), 1358–1365. 10.1212/WNL.0000000000003787 [DOI] [PubMed] [Google Scholar]
- Davico, C. , Ghiggia, A. , Marcotulli, D. , Ricci, F. , Amianto, F. , & Vitiello, B. (2021). Psychological impact of the COVID‐19 pandemic on adults and their children in Italy. Frontiers in Psychiatry, 12, 239. 10.3389/fpsyt.2021.572997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Nicola, M. , Dattoli, L. , Moccia, L. , Pepe, M. , Janiri, D. , Fiorillo, A. , Janiri, L. , & Sani, G. (2020). Serum 25‐hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID‐19 pandemic. Psychoneuroendocrinology, 122, 104869. 10.1016/j.psyneuen.2020.104869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filardi, M. , D'Anselmo, A. , Mazzoni, A. , Moresco, M. , Pizza, F. , & Plazzi, G. (2021). The importance of social zeitgeber in pediatric Type 1 Narcolepsy: What we can learn from the COVID‐19 restrictions adopted in Italy? Journal of Sleep Research, Online ahead of print. 10.1111/jsr.13423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filardi, M. , Pizza, F. , Tonetti, L. , Antelmi, E. , Natale, V. , & Plazzi, G. (2017). Attention impairments and ADHD symptoms in adult narcoleptic patients with and without hypocretin deficiency. PLoS One, 12(8), e0182085. 10.1371/journal.pone.0182085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forgeard, M. J. (2013). Perceiving benefits after adversity: The relationship between self‐reported posttraumatic growth and creativity. Psychology of Aesthetics, Creativity, and the Arts, 7(3), 245. 10.1037/a0031223 [DOI] [Google Scholar]
- Fortuyn, H. A. D. , Lappenschaar, M. A. , Furer, J. W. , Hodiamont, P. P. , Rijnders, C. A. T. , Renier, W. O. , Buitelaar, J. K. , & Overeem, S. (2010). Anxiety and mood disorders in narcolepsy: A case–control study. General Hospital Psychiatry, 32(1), 49–56. 10.1016/j.genhosppsych.2009.08.007 [DOI] [PubMed] [Google Scholar]
- Franceschini, C. , Musetti, A. , Zenesini, C. , Palagini, L. , Scarpelli, S. , Quattropani, M. C. , Lenzo, V. , Freda, M. F. , Lemmo, D. , Vegni, E. , Borghi, L. , Saita, E. , Cattivelli, R. , De Gennaro, L. , Plazzi, G. , Riemann, D. , & Castelnuovo, G. (2020). Poor sleep quality and its consequences on mental health during the COVID‐19 lockdown in Italy. Frontiers in Psychology, 11, 3072. 10.3389/fpsyg.2020.574475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González‐Blanco, L. , Dal Santo, F. , García‐Álvarez, L. , de la Fuente‐Tomás, L. , Moya Lacasa, C. , Paniagua, G. , Sáiz, P. A. , García‐Portilla, M. P. , & Bobes, J. (2020). COVID‐19 lockdown in people with severe mental disorders in Spain: Do they have a specific psychological reaction compared with other mental disorders and healthy controls? Schizophrenia Research, 223, 192–198. 10.1016/j.schres.2020.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Italy (2020). Decree of the President of the Council of Ministers 9 March 2020. Retrieved from www.gazzettaufficiale.it/eli/id/2020/03/09/20A01558/sg [Google Scholar]
- Guilford, J. P. (1967). Creativity: Yesterday, today and tomorrow. The Journal of Creative Behavior, 1(1), 3–14. 10.1002/j.2162-6057.1967.tb00002.x [DOI] [Google Scholar]
- Huang, Y. , & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID‐19 outbreak in China: a web‐based cross‐sectional survey. Psychiatry Research, 288, 112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan, T. B. , & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30, 865–878. 10.1016/j.cpr.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman, J. C. (2018). Finding meaning with creativity in the past, present, and future. Perspectives on Psychological Science, 13, 734–749. 10.1177/1745691618771981 [DOI] [PubMed] [Google Scholar]
- Lacaux, C. , Izabelle, C. , Santantonio, G. , De Villèle, L. , Frain, J. , Lubart, T. , Pizza, F. , Plazzi, G. , Arnulf, I. , & Oudiette, D. (2019). Increased creative thinking in narcolepsy. Brain, 142(7), 1988–1999. 10.1093/brain/awz137 [DOI] [PubMed] [Google Scholar]
- Mercier, M. , Vinchon, F. , Pichot, N. , Bonetto, E. , Bonnardel, N. , Girandola, F. , & Lubart, T. (2021). COVID‐19: A boon or a bane for creativity? Frontiers in Psychology, 11, 3916. 10.3389/fpsyg.2020.601150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postiglione, E. , Pizza, F. , Ingravallo, F. , Vignatelli, L. , Filardi, M. , Mangiaruga, A. , Antelmi, E. , Moresco, M. , Oriolo, C. , Pagotto, U. , & Plazzi, G. (2021). Impact of COVID‐19 pandemic lockdown on narcolepsy type 1 management. Brain and Behavior, 11(1), e01955. 10.1002/brb3.1955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues Aguilar, A. C. , Frange, C. , Huebra, L. , Dias Gomes, A. C. , Tufik, S. , & Santos Coelho, F. M. (2021). The effects of the COVID‐19 pandemic on patients with narcolepsy. Journal of Clinical Sleep Medicine, 17(4), 621–627. 10.5664/jcsm.8952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runco, M. A. , & Acar, S. (2012). Divergent thinking as an indicator of creative potential. Creativity Research Journal, 24(1), 66–75. 10.1080/10400419.2012.652929 [DOI] [Google Scholar]
- Runco, M. A. , Okuda, S. M. , & Thurston, B. J. (1987). The psychometric properties of four systems for scoring divergent thinking tests. Journal of Psychoeducational Assessment, 5(2), 149–156. 10.1177/073428298700500206 [DOI] [Google Scholar]
- Scott, G. , Leritz, L. E. , & Mumford, M. D. (2004). The effectiveness of creativity training: A quantitative review. Creativity Research Journal, 16(4), 361–388. 10.1080/10400410409534549 [DOI] [Google Scholar]
- Silvia, P. J. , Winterstein, B. P. , Willse, J. T. , Barona, C. M. , Cram, J. T. , Hess, K. I. , Martinez, J. L. , & Richard, C. A. (2008). Assessing creativity with divergent thinking tasks: Exploring the reliability and validity of new subjective scoring methods. Psychology of Aesthetics, Creativity, and the Arts, 2(2), 68. 10.1037/1931-3896.2.2.68 [DOI] [Google Scholar]
- Stoet, G. (2017). A novel web‐based method for running online questionnaires and reaction‐time experiments. Teaching of Psychology, 44(1), 24–31. 10.1177/0098628316677643 [DOI] [Google Scholar]
- Tang, M. , Hofreiter, S. , Reiter‐Palmon, R. , Bai, X. , & Murugavel, V. (2021). Creativity as a means to well‐being in times of COVID‐19 pandemic: Results of a cross‐cultural study. Frontiers in Psychology, 12, 601389. 10.3389/fpsyg.2021.601389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai, K. C. (2013). A review of the effectiveness of creative training on adult learners. Journal of Social Science Studies, 1(1), 17. 10.5296/jsss.v1i1.4329 [DOI] [Google Scholar]
- Vignatelli, L. , Plazzi, G. , Barbato, A. , Ferini‐Strambi, L. , Manni, R. , Pompei, F. , & D'Alessandro, R. (2003). Italian version of the Epworth sleepiness scale: External validity. Neurological Sciences, 23(6), 295–300. 10.1007/s100720300004 [DOI] [PubMed] [Google Scholar]
- Vignatelli, L. , Plazzi, G. , Peschechera, F. , Delaj, L. , & D'Alessandro, R. (2011). A 5‐year prospective cohort study on health‐related quality of life in patients with narcolepsy. Sleep Medicine, 12(1), 19–23. 10.1016/j.sleep.2010.07.008 [DOI] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , McIntyre, R. S. , Choo, F. N. , Tran, B. , Ho, R. , Sharma, V. K. , & Ho, C. (2020). A longitudinal study on the mental health of general population during the COVID‐19 epidemic in China. Brain, Behavior, and Immunity, 87, 40–48. 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss, D. S. (2007). The impact of event scale: revised. In Cross‐cultural assessment of psychological trauma and PTSD (pp. 219–238). Springer. 10.1007/978-0-387-70990-1_10 [DOI] [Google Scholar]
- Wu, M. , Ren, J. , Li, S. X. , Xue, P. , Su, C. , & Zhou, J. (2021). Management of narcolepsy during COVID‐19: a challenge or an opportunity? Sleep, 44(2), zsaa273. 10.1093/sleep/zsaa273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying, D. , Yang, Y. , Xie, C. , Wang, X. , Liu, C. , Hu, W. , & Li, Y. (2020). A positive role of negative mood on creativity: the opportunity in the crisis of the COVID‐19 epidemic. Frontiers in Psychology, 11, 3853. 10.3389/fpsyg.2020.600837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamarian, L. , Högl, B. , Delazer, M. , Hingerl, K. , Gabelia, D. , Mitterling, T. , Brandauer, E. , & Frauscher, B. (2015). Subjective deficits of attention, cognition and depression in patients with narcolepsy. Sleep Medicine, 16(1), 45–51. 10.1016/j.sleep.2014.07.025 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.


