Abstract
The Coronavirus disease 19 (COVID-19) pandemic has disrupted both transportation and health systems. While about 40% of Americans have delayed seeking medical care during the pandemic, it remains unclear to what extent transportation is contributing to missed care. To understand the relationship between transportation and unmet health care needs during the pandemic, this paper synthesizes existing knowledge on transportation patterns and barriers across five types of health care needs. While the literature is limited by the absence of detailed data for trips to health care, key themes emerged across populations and settings. We find that some patients, many of whom already experience transportation disadvantage, likely need extra support during the pandemic to overcome new travel barriers related to changes in public transit or the inability to rely on others for rides. Telemedicine is working as a partial substitute for some visits but cannot fulfill all health care needs, especially for vulnerable groups. Structural inequality during the pandemic has likely compounded health care access barriers for low-income individuals and people of color, who face not only disproportionate health risks, but also greater difficulty in transportation access and heightened economic hardship due to COVID-19. Partnerships between health and transportation systems hold promise for jointly addressing disparities in health- and transportation-related challenges but are largely limited to Medicaid-enrolled patients. Our findings suggest that transportation and health care providers should look for additional strategies to ensure that transportation access is not a reason for delayed medical care during and after the COVID-19 pandemic.
Keywords: Health care, Access to care, Transportation equity, COVID-19, Non-emergency medical transportation, NEMT
1. Introduction
The Coronavirus disease 19 (COVID-19) pandemic introduced broad transportation system challenges that have restricted transportation access across the United States. From reduced public transit service to lessened ability to rely on others for fear of contracting the virus, people who already struggled with transportation likely find themselves at an even greater disadvantage now. Transportation disadvantage was widely recognized as a barrier to health care access before the pandemic (Syed et al., 2013), and programs such as paratransit (operated by public transit agencies) and Non-Emergency Medical Transportation (funded and arranged by Medicaid, the public health insurance program for low-income Americans) exist to help people with medical or physical limitations get to essential destinations. The public health threat of COVID-19 has increased the urgency of understanding and alleviating transportation barriers to health care via existing and emerging strategies.
Health systems have made efforts to mitigate barriers to care during the COVID-19 pandemic while maintaining public safety. At the start of the pandemic, most health systems deferred non-emergency medical procedures and replaced in-person appointments with video or telephone visits. However, many types of medical care still require in-person visits, and health systems are increasingly resuming elective in-person care. Delivering necessary in-person care during the pandemic likely requires new transportation strategies.
Emerging data suggest that since the start of the pandemic, many Americans have been unable or unwilling to meet their non-COVID-19-related medical needs. One recent study of data from a West Coast medical system found that transportation barriers are associated with significantly higher odds of a positive COVID-19 test (Rozenfeld et al., 2020). This may reflect a greater risk of disease exposure associated with insecure transportation and therefore greater reliance on public transit and/or shared rides, or it may suggest inadequate access to health care, including timely COVID-19 testing. From April through July 2020, 40% of U.S. adults reported that they had delayed medical care because of the pandemic (U.S. Census Bureau, 2020a). By late October 2020, about 31% of adults still reported these delays, with slightly higher rates of delayed care among women (34%, vs. 28% of men) and among Hispanic adults (35%, vs. 30% of non-Hispanic Whites, 31% of African Americans, and 32% of Asians) (U.S. Census Bureau, 2020b). Little is known about the extent to which transportation has been a barrier to care during the pandemic.
In this article, we seek to examine the likely impacts of the COVID-19 pandemic on transportation for non-COVID-19-related health care in the United States. After briefly considering how the pandemic has impacted transportation and health care systems in general, we examine this issue through the lens of five different types of health care needs: dialysis, prenatal care, cancer treatment, mental-health and substance-use treatment, and health care for people with disabilities. These health care needs are significant because they are disproportionately prevalent among people with transportation disadvantages and/or because transportation interventions are cost-effective or even cost-saving for people with these needs (Bernardo et al., 2019, Wallace et al., 2006).
1.1. Changes in transportation and health care delivery
Changes in employment, transportation service, and health facility operations during the COVID-19 pandemic have broad and potentially long-lasting implications for transportation to health care settings.
First, the COVID-19 pandemic's toll on the labor market has reshaped how and where people access health care. With the estimated number of Americans out of work or underemployed topping 30 million (Shierholz, 2020), many Americans are likely to be newly uninsured. Public health insurance programs have worked to extend access to their plans during the pandemic (Garrett and Gangopadhyaya, 2020), but it is likely that about 7.3 million recently unemployed workers are newly uninsured (Woolhandler and Himmelstein, 2020) in addition to the 29 million Americans who were uninsured before the pandemic (Tolbert et al., 2020). Changes in where people live have also impacted health care travel. Roughly one in five Americans has moved or knows someone who has moved due to job loss, economic insecurity, and educational instruction changes due to the pandemic (Cohn, 2020). People who have moved have been shown to suffer reduced access to care for at least two years after relocating (Chen et al., 2020) and may face longer trips to their prior health care providers, or they may need to find new routes to unfamiliar health facilities. The pace of the nation’s economic recovery, which quickened in summer 2020 but has since slowed amid stagnant consumer demand in many industries (Weber Handwerker et al., 2020), will likely shape how long the pandemic’s economic impact alters access to care for vulnerable Americans.
Second, in response to declining ridership and fiscal pressures, public transit agencies have reduced service in most regions (Hu and Chen, 2021). Additionally, ride-hailing service providers Lyft and Uber have suspended their lower-cost shared-ride services during the pandemic (Bond, 2020). Some volunteer driver programs, such as the “Road to Recovery” program provided by the American Cancer Society, have suspended or reduced service (American Cancer Society, 2020). As a result of these service changes, people who have relied on public transportation, lower-cost shared ride-hailing services, or rides from people living both inside and outside of their home face additional transportation burdens because of the pandemic. Although shared ride services and volunteer driver programs may return once widespread COVID-19 vaccination suppresses the pandemic, the future of public transportation remains under long-term threat, as service cuts and delayed infrastructure upgrades may deter potential riders even after recovery from the COVID-19 pandemic (Verma, 2020). Public transit cuts may be particularly harmful for residents who use transit more (including people without cars, people of color, and low-wage essential workers) as well as for residents of transit deserts, where levels of transit demand outpace available transit services (Martin et al., 2016, Manville et al., 2018, TransitCenter, , 2020, Jiao and Dillivan, 2013). Recent studies have shown that transit service cuts disproportionately impact residents of lower-income, less-educated, and less White neighborhoods, where the drop in transit demand during the pandemic has been the smallest (Brough et al., 2021, Hu and Chen, 2021).
Third, health care facilities have replaced many in-person visits with telemedicine (health care delivered by telephone, video conference, or electronic messaging) to reduce COVID-19 transmission risk (Abelson, 2020, Levey, 2020). This shift has been eased by temporary federal regulatory changes that made it easier for providers to be reimbursed for telemedicine visits during the pandemic (U.S. Department of Health and Human Services, 2020). Although health care visits are down across the board, clinical specialties such as psychiatry, psychology, and endocrinology, which have replaced the largest proportion of patient visits with telemedicine, have generally seen the smallest drops in visit volumes, whereas fields like optometry, physical therapy, and orthopedics have had lower adoption of telemedicine and larger drops in visit volumes (Patel et al., 2021).
Notably, telemedicine has not been able to reach all patients. Patients who are older, lower-income, and non-English-speaking have been least likely to receive care via telemedicine during the COVID-19 pandemic (Eberly et al., 2020, Kakani et al., 2021). Furthermore, residents of neighborhoods with lower income, lower education, and lower broadband internet access have been less likely to access video visits (as opposed to telephone visits), potentially limiting the effectiveness of virtual care they do receive (Rodriguez et al., 2021). It is thus no surprise that community health centers serving low-income and uninsured patients have had more difficulty implementing telemedicine (Johnson and Goodnough, 2020, Kim et al., 2020b). These and other barriers to reaching patients during the pandemic led to the temporary closure of nearly 2000 federally-funded community health center sites, which form the backbone of safety-net health care for many of the most economically and medically vulnerable Americans (HRSA Bureau of Primary Health Care, 2020). For patients who rely on community health centers, clinic closures may mean longer travel distances, greater difficulty accessing health care, and worse clinical outcomes for treatable conditions (Kishore and Hayden, 2020). Fortunately, federal relief funding and increasing adoption of telemedicine have helped many community clinics stay afloat, and community clinics are now poised to play a central role in delivering COVID-19 vaccines in neighborhoods hardest-hit by the pandemic (Corallo et al., 2020).
Finally, some trips to health care may have been eliminated or rerouted thanks to mobile care services. Mobile medical clinics have existed for years; most are supported by private philanthropy, leading to operational and funding challenges that have limited their services to a small segment of the health care sector. During the COVID-19 pandemic, as many as 80% of existing mobile clinics temporarily suspended or reduced operations, while some physical clinics began to offer new mobile services (Attipoe-Dorcoo et al., 2020, Heath, 2020). In addition to mobile clinics, paramedics and paratransit agencies have also worked to address transportation barriers by delivering non-emergency care, medications, food, COVID-19 tests, and vaccines to high-risk patients at their homes during the pandemic, but it is unclear whether these programs will be scalable or sustainable after the pandemic (Attipoe-Dorcoo et al., 2020, Corallo et al., 2020, Wicklund, 2020).
Structural inequity is evident in the repeated racial and socioeconomic patterns in poverty, job and insurance loss, transportation disadvantage, and access to telemedicine felt disproportionately among people and communities of color (Johnson and Goodnough, 2020, Kim et al., 2020a, Kim et al., 2020b).
2. Methods
To illustrate different aspects of the COVID-19 pandemic’s impact on transportation and its potential influence on health care, we outline considerations and constraints for transportation to five specific types of health care during the pandemic. Lack of transportation is a documented barrier to accessing health care for end-stage kidney disease (Ellis et al., 2019), cancer care (Burg et al., 2010), prenatal care (Braveman et al., 2000, Mazul et al., 2017), care for mental health and substance use disorders (Choi and Gonzalez, 2005, Palmer et al., 2009), and health care, in general, for people with disabilities (Drainoni et al., 2006, Henning-Smith et al., 2016). The first four of these health conditions were examined in a 2006 cost-effectiveness analysis, which found that transportation interventions to overcome barriers to health care can be cost-effective or cost-saving for society and might improve quality of life and life expectancy for these patients (Wallace et al., 2006). Here, we expand on the list of health care needs identified by Wallace et al. to additionally explore health care transportation needs among people with disabilities, who require and use health care at higher rates than people without disabilities and often face added challenges when traveling (Anand and Ben-Shalom, 2014, Kennedy et al., 2017).
Given the quickly evolving nature of the COVID-19 pandemic, we performed a rapid literature review by searching academic databases focused on medicine, public health, and social sciences, including PubMed, TRID (Transportation Research International Documentation), ScienceDirect, PAIS Index, AcademicSearchComplete, and Google Scholar. Our search strategy combined descriptors of each health care need and/or associated patient population with transportation keywords including “transportation needs,” “transportation access,” “public transportation,” and other travel modes. We focused on research from the United States conducted in the last 30 years. Additionally, we searched gray literature through Google and Google Scholar to identify reports and news articles relevant to the transportation needs and COVID-19 context for each type of health care need.
In addition to reviewing the literature, we also incorporated a small descriptive analysis of data from the 2017 National Household Travel Survey (NHTS), a nationally-representative sample of travel in the United States (Federal Highway Administration, 2020), with the goal of understanding how people typically travel to health care. NHTS collects information on respondents’ disability status but not on specific health care needs or health conditions, so we evaluated NHTS data for just one of the five health care needs examined in this report: care for people with disabilities. For this analysis, we classified NHTS respondents as having disabilities if they reported having a disability that limited travel outside of the home (Brumbaugh, 2018). Using the trip purpose summary data, we defined trips to health care as travel to obtain “medical/dental services.” We report the proportion of trips to health care made by people with versus without disabilities via each of the following modes: personal vehicle, public transit, paratransit, taxi/ride-hailing, walk, bicycle, and other. NEMT services were not explicitly identified in NHTS survey questions but were likely reported as either “Taxi/ride-hailing” or “Other.” Because raw NHTS data describe trips that survey participants took over the course of a single day, we applied trip weights in order to estimate the annual travel behaviors of the United States population and to account for NHTS sampling procedures.
3. Findings
3.1. Dialysis for End-Stage Kidney Disease
Most people with end-stage kidney disease (ESKD) depend on dialysis, a blood filtration process that replaces the function of the kidneys. Dialysis sessions, which in most cases are necessary to keep these patients alive, last several hours and typically require visits to a dialysis facility three to four times per week. During the COVID-19 pandemic, there has been a push to increase the use of home-based dialysis (Brown and Perl, 2020, Yerram and Misra, 2020), but most patients are still traveling to dialysis facilities for their care. Dialysis facilities have implemented a number of COVID-19 related safety protocols, including clustering patients during treatments and transportation (Verma et al., 2020) as well as dedicating treatment facilities to dialysis for COVID-19-positive patients (Ikizler and Kliger, 2020).
Notably, racial and ethnic minorities are disproportionately impacted by ESKD. After controlling for gender and age, the prevalence of ESKD incidence is 3.7 times higher for African Americans and 9.5 times higher for Native Hawaiians/Pacific Islanders compared to non-Hispanic Whites, while prevalence among Hispanics is 1.6 times greater than among non-Hispanics. The same minority groups are also less likely than Whites to receive kidney transplants, which can eliminate the need for dialysis and the travel associated with it (United States Renal Data System, 2019). These racial/ethnic inequities in ESKD are driven predominantly by social and structural factors related to lower socioeconomic status, worse access to care, clinician bias, lower quality of care, and worse control of ESKD risk factors (Norris et al., 2017).
Many patients with ESKD require help with transportation to dialysis, even in the absence of a pandemic. Due to various factors, including their advanced stage of illness and the fatigue associated with the dialysis procedure itself, about three out of four patients do not drive themselves to and from dialysis facilities. Roughly half of patients on dialysis rely on various forms of public transportation, including paratransit, to get to their dialysis sessions. Twenty percent rely on rides from friends and family, and ten percent rely on Non-Emergency Medical Transportation (NEMT) rides (arranged and paid for by an insurer, usually Medicaid) or other similar services (Ellis et al., 2019).
Existing programs for transportation to dialysis are far from perfect. Patients without private vehicles who rely on these programs cite unreliability and scheduling difficulty as significant concerns. A paratransit van may be late in dropping off a patient, resulting in a shortened—and often incomplete—dialysis treatment. In some cases, transportation worries provoke so much stress that patients choose to end dialysis early to ensure that they do not miss a ride (Ellis et al., 2019). Transportation barriers also contribute to patients missing appointments altogether, with grave consequences: skipped or shortened dialysis sessions put patients at increased risk for hospitalization and life-threatening complications (Chan et al., 2014, Gray et al., 2017, Obialo et al., 2012). These adverse events are particularly concerning for people who rely on public transportation, as they miss dialysis sessions more often than people who use private vehicles (Chan et al., 2014).
3.2. Prenatal care
For many women, pregnancy occasions a sudden uptick in the frequency of trips to medical care. Pregnant women are asked to attend upwards of twelve prenatal care visits during a typical pregnancy. Even before the pandemic, clinicians had begun to question the recommended frequency of prenatal care visits (Carter et al., 2016); COVID-19 only heightened the push for fewer trips to prenatal care. During the pandemic, obstetricians have implemented new prenatal care schedules, recommending as few as five total in-person visits for low-risk women. These clinicians are using virtual visits and home monitoring devices to check in with patients in between their trips to the clinic (Peahl, 2020, The American College of Obstetricians and Gynecologists, 2020).
However, even with the reduced number of prenatal care visits during the pandemic, transportation challenges will likely remain a barrier to adequate and timely prenatal care for some women. Transportation barriers are especially common among low-income women of color, who remain at significant risk for missed prenatal care (Braveman et al., 2000, Mazul et al., 2017); for example, in 2018, 81% of pregnant White women received timely and adequate prenatal care, compared to 68% of pregnant Black women and 72% of Hispanic women (Office of Disease Prevention and Health Promotion, 2020). This reduced access to prenatal care contributes to the fact that Black women are about 3 times more likely than White women to die from pregnancy-related complications (Petersen, 2019). Previous studies highlight how transportation interventions (e.g. bus passes and taxi vouchers) can increase women's timely engagement with prenatal care in certain settings (Melnikow et al., 1997) but may need to be paired with broader socioeconomic support to be most effective (Johnson et al., 2011).
3.3. Cancer care
The landscape of transportation to cancer care in the United States was already shifting before the COVID-19 pandemic. In the last few decades, advances in treatment options and changing reimbursement rules have driven a transition in oncology care from a dispersed web of community clinics to more specialized, centralized, hospital-based clinics. As a result, cancer patients face longer travel distances and widening travel disparities (Fisher et al., 2016, Stitzenberg et al., 2009, Yang and Wapnir, 2018).
Similar to patients requiring facility-based dialysis, many people seeking active cancer treatment have continued to rely on in-person care during the COVID-19 pandemic, as many cancer treatments cannot be delivered at home. The health consequences of delayed cancer care are highly variable across patient factors and cancer treatment characteristics, and the risk of COVID-19 transmission has forced oncologists to make complicated triage decisions. Some interventions, such as surgery for low-risk prostate cancer, are considered safe to delay for several months or longer. In contrast, other treatments, like radiation therapy for fast-spreading gynecologic cancers, should not be delayed at all, lest the narrow window for treatment success close as the pandemic continues to cause major devastation across the nation (Kutikov et al., 2020).
Estimating the impact of the COVID-19 pandemic on transportation to cancer care is challenging because of scant literature assessing the impact of mode of transportation on cancer treatment. Previous studies have focused predominantly on the correlation between transportation mode and receipt of cancer screening, rather than cancer treatment. A 1991 study of older patients in New Mexico who were newly diagnosed with cancer found that 33% of participants relied on others for rides to cancer care (Goodwin et al., 1991); more recent transportation-mode data for trips to cancer treatment are lacking. Nonetheless, transportation barriers are prominent in this clinical setting. In national studies, the percentage of patients who reported that transportation was a barrier to accessing cancer care varies from 13 to 19% (Shelby et al., 2002, Zullig et al., 2012).
As a result of greater exposure to cancer risk factors, lower access to routine cancer screening tests, and greater barriers to initiating treatment once diagnosed with cancer, inequities in cancer care parallel those observed in other health conditions. For example, although White women are slightly more likely than Black women to be diagnosed with breast cancer, Black women are more likely to die from breast cancer (Yedjou et al., 2019). Meanwhile, both the incidence and mortality rates for prostate cancer are higher for Black men compared to White men (Siegel et al., 2020).
3.4. Mental health care and substance use treatment
Although mental health and substance use disorders are grouped together under the jurisdiction of the federal Substance Abuse and Mental Health Services Administration, the role of transportation in access to care for these two types of disorders often differs. Milder forms of common mental health disorders, such as depression and anxiety, are often treated by primary care physicians and therapists in local community clinics (Unützer and Park, 2012). In contrast, severe mental illness and substance use disorder (SUD) often require treatment at specialized facilities. Often clustered in urban centers, these specialized facilities may necessitate prolonged travel for residents of suburban and rural areas (Ghorbanzadeh et al., 2020). Patients seeking medication therapy for opioid use disorder, a type of SUD, have been particularly burdened by frequent trips to care. Federal rules require patients treated with methadone to travel to specialized clinics most days of the week to pick up their daily dose of medication. Patients treated instead with buprenorphine are typically seen in-person on a weekly or bi-weekly basis (Jankowski, 2019, Priest, 2020).
Adaptation to the COVID-19 pandemic has differed starkly between systems of care for mental health conditions and SUD. Most mental health providers have transitioned to telemedicine, which, prior to the pandemic, had been demonstrated to be as safe and effective as in-person care for common mental health conditions (Bashshur et al., 2016, Hubley et al., 2016, Whaibeh et al., 2020). There may, however, be barriers to initiating treatment for new patients.
In contrast, delivering SUD treatment during the pandemic has required more significant changes from usual practice. The Drug Enforcement Agency issued a temporary rule at the start of the pandemic allowing clinics to dispense up to a month's supply of methadone and to initiate buprenorphine treatment via telemedicine. Although these relaxed guidelines should reduce travel burden for patients, not all SUD treatment facilities have implemented these changes (Dunlop et al., 2020, Priest, 2020). Combined with closures and reduced hours at some facilities, patients seeking SUD treatment may be stuck making frequent and potentially longer trips to care during the pandemic (Davis and Samuels, 2020, Dunlop et al., 2020, Priest, 2020). A study based in Philadelphia estimated that a patient’s likelihood of initiating outpatient SUD treatment was cut in half for every 10 minutes of added driving time (Mennis et al., 2012).
In general, the transportation needs and behaviors of people seeking care for common mental health conditions and SUD are not well understood. There is some evidence that both groups of patients are more likely to depend on public transportation and/or rides from others compared to the general population (O’Brien et al., 2019). Among people with mental illness and SUD, lower transportation independence and longer travel distances may contribute to lower likelihood of initiating treatment and increased risk of dropping out of treatment (Mennis et al., 2012, Palmer et al., 2009, Rosen et al., 2004).
Notably, rates of mental illness are roughly equal across racial/ethnic groups, but Black and Hispanic patients with probable mental illness are less likely than White patients to initiate treatment (Lê Cook et al., 2014). Although data are mixed on whether rates of initiating treatment for SUD differ by race/ethnicity (Lê Cook and Alegría, 2011), communities with higher concentrations of Black residents are served by fewer SUD treatment facilities that accept Medicaid, suggesting that low-income Black patients may have to travel farther to access SUD treatment (Cummings et al., 2014).
Transportation challenges, coupled with the additional stresses of COVID-19, may not only exacerbate the treatment needs of existing patients with mental illness and SUD but also increase the number of people requiring care for new-onset conditions (Czeisler et al., 2020). The pandemic seems to have widened racial inequities, too: recent data from Massachusetts has shown that during the COVID-19 pandemic, the volume of mental health and SUD visits dropped significantly more among Black and Hispanic patients than among White patients (Yang et al., 2020).
3.5. People with disabilities
More than 40 million Americans have some form of disability (hearing, vision, cognitive, physical/ambulatory or other) that limits their participation in daily activities in minor to major ways (U.S. Census Bureau, 2020c). The prevalence of disabilities is highest among Native Americans (29.9%) and Black Americans (21.2%) and lowest among Asian Americans (11.6%) (Wolf et al., 2008).
Disability often occurs as a secondary health condition; for example, people with multiple sclerosis may experience physical and visual limitations secondary to their neurological disorder. Health care needs and travel patterns for accessing health care vary widely across categories of disability and types of underlying health conditions. Duration of disability likely also influences travel behaviors: patients who have experienced their disability for longer may be more likely to have developed strategies to overcome their disability-related limitations (Henly and Brucker, 2019).
In general, people with disabilities require health care more frequently and are more likely to have delayed or not received necessary care compared to people without disabilities (Henning-Smith et al., 2016). When they do travel to health care, people with disabilities spend more time in transit, even after controlling for trip distance and various personal and modal characteristics (Brucker and Rollins, 2016). People with disabilities are also more likely to have low income and to depend on federal health insurance programs (Kennedy et al., 2017), making them potentially eligible for transportation assistance through NEMT services offered by Medicaid and, to a lesser extent, Medicare.
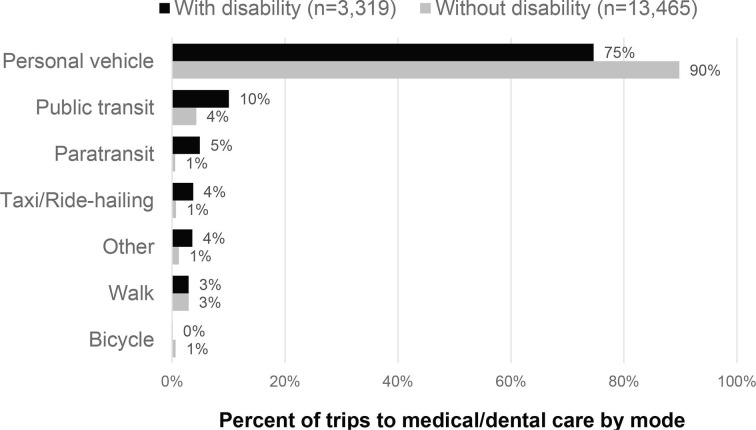
Using the National Household Travel Survey, as described above, we analyzed data on mode of travel to health care for people with disabilities. Fig. 1 presents our bivariate analysis showing the distribution of modes used for trips to health care among people with and without disabilities. These estimates are based on 2017 NHTS data describing 16,784 trips to health care reported in a sample of 129,696 US households (Federal Highway Administration, 2020). The weighted estimates shown in Fig. 1 represent an estimated 5.6 billion trips to health care made each year in the U.S. Compared to people without disabilities, those with disabilities are generally more likely to use modes that require contact with others, namely public transit, paratransit, and taxi/ride-hailing services.
Fig. 1.
Modal frequency for trips to medical/dental care among people with and without travel-limiting disabilities in the 2017 National Household Travel Survey. Sample sizes (n) are unweighted; percentages reflect estimates that were weighted to represent total annual travel by the United States population) (Federal Highway Administration, 2020).
Notably, a recent study of San Francisco residents with disabilities showed that dependence on others for rides and fear of exposure to COVID-19 during travel resulted in heightened barriers to seeking medical care during the pandemic (Cochran, 2020). Patterns revealed in the NHTS trip data thus have important implications for improving access to care for people with disabilities, given this population’s increased reliance on travel modes most impacted by the pandemic.
4. Discussion of key themes
Four cross-cutting themes emerged from this review of COVID-19-related transportation system disruptions in the context of existing disparities in health care access.
4.1. Compounding inequity
Reduced trips to health care during the COVID-19 pandemic may have serious long-term effects on health disparities. Although some routine health services, like some screening tests for breast or colorectal cancer, can likely be safely delayed by a year without causing major harm, delays in other types of care can lead to deterioration of many acute and chronic health conditions. Clinicians have warned that avoidable complications from missed care could result in an increased demand for health care for years to come (Chen and McGeorge, 2020, Kohli and Virani, 2020). Disparities in access to health care during the pandemic may thus translate to even greater health inequities after the pandemic.
For each of the health care needs highlighted in this report, the same communities—especially low-income families and Black, Indigenous, and People of Color—are subject to policies and practices rooted in structural racism that lead to compounding inequality in socioeconomic standing along with impaired access to multiple resources, including transportation and health care. Not only do these structural inequalities place these communities at elevated risk for many adverse health conditions, they also contribute to greater transportation challenges when health care is needed. These groups that are historically and persistently marginalized and under-resourced because of discrimination through multiple reinforcing systems of housing, education, employment, health care, earnings, criminal justice, and more (Bailey et al., 2017) are also hardest hit by the economic and health-related consequences of COVID-19. These intersecting structural barriers underlie and exacerbate disparities in transportation and health. Achieving health equity will require both systemic reform and immediate, targeted relief to overcome transportation barriers to health care for marginalized groups.
4.2. Strategies for overcoming transportation barriers
Across all of the health care needs we surveyed, we found extensive use of public transit, paratransit, NEMT services, and rides from others. In order to ensure that the most medically vulnerable patients retain access to these programs during and after the COVID-19 pandemic, leaders in transportation and health care will need to pay close attention to the relationship between their fields. Clinical teams should work with patients to understand their transportation needs in order to better advocate for equitable access to care. Transportation agencies must ensure that service cuts are not creating even greater barriers to health care access among people with the highest need. In the short term, both health care and transportation agencies will need to augment efforts to enroll eligible patients into transportation programs, like NEMT for patients with Medicaid or paratransit service for people with disabilities. Additionally, expanding Medicaid eligibility criteria could help increase the number of transportation-disadvantaged patients who can benefit from NEMT.
In the longer term, increased public transportation funding and service is likely to benefit both transportation and health care industries. In light of the growing recognition that health outcomes are largely influenced by circumstances outside the doctor’s office, it may also be wise to expand the types of trip destinations covered by NEMT. Lastly, coordinating or consolidating NEMT and paratransit may be worth considering as a strategy to enhance service efficiency and effectiveness, given the overlapping rider demographics and objectives of these programs (Rall and Myers, 2015). Although likely to be bureaucratically complex up front, improved coordination has high potential to provide a better, simpler transportation experience that helps overcome existing barriers to health care access.
Notably, while existing services may all help overcome transportation barriers, they can also have shortcomings related to reliability, convenience, and cost. Successful interventions provide patients with lower-cost or more reliable transportation, and people who can overcome transportation barriers are more likely to receive their necessary health services (Whetten et al., 2006). However, research to date has yielded mixed evidence on whether offering transportation assistance reduces no-show rates, suggesting that such interventions may need to be tailored to the highest-need patients to be most effective (Solomon et al., 2020). During the COVID-19 pandemic, any transportation intervention that involves contact between non-household members must also emphasize careful hygiene and social distancing practices to reduce the risk of viral transmission.
Increasingly, ride-hailing and technology companies are partnering with health care, health insurance, and paratransit providers to improve access to care. A recent review identified 53 instances of these partnerships (Wolfe and McDonald, 2020). A growing number of state Medicaid programs have partnered with ride-hailing companies to provide NEMT, and during the pandemic at least three additional states have taken steps to facilitate new partnerships (Fraade-Blanar and Whaley, 2020). Because of the flexible, on-demand nature of ride-hailing services and the potential to integrate ride requests directly into the patient's medical records, patients have found these services appealing and convenient (Wolfe and McDonald, 2020). Health care systems and insurers may be particularly motivated to pursue these partnerships because of their potential to improve patient health outcomes while protecting revenue during the COVID-19 pandemic by reducing transportation-related no shows and delays.
An alternative strategy for addressing individualized transportation needs is the patient navigator model, which originated in the 1990s to improve outcomes for low-income women with breast cancer (Riley and Riley, 2016). This model takes many forms but centers on the use of a designated navigator (typically a nurse, social worker, or fellow patient) who is trained to understand patients' various health-related social needs and challenges. The navigator’s job is to find flexible solutions to various intersecting barriers to health care, including transportation issues. Patient navigator programs have the potential to be more effective than isolated transportation interventions by addressing co-occurring issues like childcare, which can create transportation barriers but may not be resolved with transportation assistance alone. Published estimates suggest that navigators spend between 6 and 25% of their time arranging transportation (Lin et al., 2008, Phillips et al., 2014). Patient navigator programs have been effective at improving timely diagnosis and treatment for patients with cancer in diverse settings (Bush et al., 2018), and they are increasingly used outside of the cancer context (Peart et al., 2018).
Finally, the COVID-19 pandemic has also demonstrated that strategies to reduce the need for health care trips – such as increased use of telemedicine, novel use of mobile care units, and relaxed requirements for in-person SUD treatment – may be necessary for improving access to health care for people facing transportation barriers. Transportation leaders can join clinicians in advocating for policy change to ensure that these positive but temporary COVID-19 policies become permanent. Advocacy for expanded access to health insurance and broadband internet can also support long-term equity in access to health care.
4.3. Risk/benefit trade-offs
The COVID-19 pandemic has added a layer of risk to all travel, including trips to health care settings. Any trip must be assessed as a trade-off between potential risks and benefits. Individuals must weigh COVID-19 exposure risk versus the need for health care, not only for acute and chronic conditions but also for the prevention of future illness. There are risks and benefits at the community level, too: more trips to health care may contribute to COVID-19 transmission and externalities of vehicle emissions, but they also provide financial support for public transportation and community clinics during a time of economic vulnerability. While health care trips via shared vehicles (such as ride-hailing services, volunteer drivers, or other cars) may mean more cars on the road, they may be the easiest and most flexible way to overcome transportation barriers for vulnerable patients during the pandemic.
Leaders in health care and public health have begun to develop risk/benefit tools to help patients and clinicians weigh trade-offs in seeking or delaying care during the pandemic (Centers for Disease Control and Prevention, 2020, Kutikov et al., 2020). These tools can be improved by more explicitly considering transportation factors, and health care providers should enhance screening for pandemic-related transportation barriers when possible. Transportation agencies and policymakers may also wish to develop similar risk/benefit decision tools to ensure equitable and safe decision-making as the pandemic continues.
4.4. Need for quality data
Assembling this review was limited by the paucity of data connecting transportation and specific health conditions and/or health care needs, especially related to modes of travel to health care. In particular, we were unable to quantify what proportion of the reduction in trips to health care during the pandemic stemmed from transportation-related hesitation or barriers. In a national survey conducted in the early months of the pandemic, respondents who had missed necessary medical care cited reasons including closure of a medical practice (63%), fear of COVID-19 exposure (57%) and financial hardship (7%) (Anderson et al., 2021). A subsequent study estimated that 24% of people who had missed health care during the pandemic did so because they “felt the health care location was too far or difficult to get to” (Wood Johnson Foundation/HarvardChan School of Public Health, 2020). Although neither survey explicitly asked about transportation, transportation issues conceivably could have contributed to or been exacerbated by each of these reasons for missed health care. A third study found that the perceived risk of COVID-19 infection by travel mode was highest for public transit and shared rides, while the perceived risk by trip destinations was highest for hospitals (Shamshiripour et al., 2020). In the context of these reports, the findings from our review suggest that future studies should evaluate the extent to which transportation barriers have contributed to missed care, especially for vulnerable patient populations.
Even outside of the pandemic context, health systems have not often collected information on patients' transportation access (like car ownership) or how they arrive at their appointments. Paratransit services and Medicaid-funded NEMT represent large public investments; however, the lack of consolidated national data on the use of these services makes it hard to identify patterns in their use across geography, health systems, health care needs, and patient demographics (Chaiyachati et al., 2018). Furthermore, the extent to which volunteer driver programs fulfill health care transportation needs remains unmeasured.
5. Conclusion
As transportation and health care systems continue to grapple both independently and jointly with serving the needs of Americans during the COVID-19 pandemic, leaders in both sectors would benefit from greater attention to the intersection of these two fields. Many people are delaying health care during the pandemic, and existing knowledge on how patients access health care suggests that transportation system disruptions are likely contributing in part to these delays.
Transportation issues have always been a significant component of health care access, with implications for quality of care and health outcomes. Given the additional transportation barriers facing patients during the COVID-19 pandemic, it is more urgent than ever that transportation stakeholders— spanning traditional transportation and health care sectors— collaborate to increase access to transportation services.
Findings in this paper suggest that solutions will need to be both big and small, incremental and systematic, targeted and universal. Better understanding and addressing the challenges of populations that are most in need requires a critical approach to reducing transportation barriers to health care for all. Achieving equity in health care access is inextricably linked to achieving equity in transportation, and this relationship has been magnified during the protracted COVID-19 pandemic.
CRediT authorship contribution statement
Katherine L. Chen: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing, Project administration, Funding acquisition. Madeline Brozen: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing, Project administration, Funding acquisition. Jeffrey E. Rollman: Conceptualization, Methodology, Investigation, Writing - review & editing, Funding acquisition. Tayler Ward: Conceptualization, Methodology, Investigation, Writing - review & editing. Keith C. Norris: Conceptualization, Methodology, Writing - review & editing, Supervision, Funding acquisition. Kimberly D. Gregory: Conceptualization, Methodology, Writing - review & editing, Supervision, Funding acquisition. Frederick J. Zimmerman: Conceptualization, Methodology, Writing - review & editing, Supervision, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The research team wishes to acknowledge the support from Julene Paul and Miriam Pinski for their assistance analyzing NHTS data.
References
- Abelson, R., 2020. Doctors and Patients Turn to Telemedicine in the Coronavirus Outbreak. N. Y. Times.
- Anand P., Ben-Shalom Y. How do working-age people with disabilities spend their time? New evidence from the American time use survey. Demography. 2014;51(6):1977–1998. doi: 10.1007/s13524-014-0336-3. [DOI] [PubMed] [Google Scholar]
- Anderson K.E., McGinty E.E., Presskreischer R., Barry C.L. Reports of forgone medical care among US adults during the initial phase of the COVID-19 pandemic. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.34882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attipoe-Dorcoo S., Delgado R., Gupta A., Bennet J., Oriol N.E., Jain S.H. Mobile health clinic model in the COVID-19 pandemic: lessons learned and opportunities for policy changes and innovation. Int. J. Equity Health. 2020;19:73. doi: 10.1186/s12939-020-01175-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Bashshur R.L., Shannon G.W., Bashshur N., Yellowlees P.M. The empirical evidence for telemedicine interventions in mental disorders. Telemed. J. E Health. 2016;22:87–113. doi: 10.1089/tmj.2015.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardo B.M., Zhang X., Hery C.M.B., Meadows R.J., Paskett E.D. The efficacy and cost-effectiveness of patient navigation programs across the cancer continuum: A systematic review. Cancer. 2019;125:2747–2761. doi: 10.1002/cncr.32147. [DOI] [PubMed] [Google Scholar]
- Braveman P., Marchi K., Egerter S., Pearl M., Neuhaus J. Barriers to timely prenatal care among women with insurance: the importance of prepregnancy factors. Obstet. Gynecol. 2000;95:874–880. doi: 10.1016/S0029-7844(00)00780-8. [DOI] [PubMed] [Google Scholar]
- Brough R., Freedman M., Phillips D. Understanding socioeconomic disparities in travel behavior during the COVID-19 pandemic. Journal of Regional Science. 2021 doi: 10.1111/jors.12527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown E.A., Perl J. Increasing peritoneal dialysis use in response to the COVID-19 pandemic: will it go viral? J. Am. Soc. Nephrol. 2020;31:1928–1930. doi: 10.1681/ASN.2020050729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brucker D.L., Rollins N.G. Trips to medical care among persons with disabilities: Evidence from the 2009 National Household Travel Survey. Disabil. Health J. 2016;9:539–543. doi: 10.1016/j.dhjo.2016.01.001. [DOI] [PubMed] [Google Scholar]
- Brumbaugh S. Department of Transportation Bureau of Transportation Statistics, Washington D.C; U.S: 2018. Travel Patterns of American Adults with Disabilities (Issue brief)https://www.bts.gov/sites/bts.dot.gov/files/docs/explore-topics-and-geography/topics/passenger-travel/222466/travel-patterns-american-adults-disabilities-9-6-2018_1.pdf [Google Scholar]
- Burg M.A., Zebrack B., Walsh K., Maramaldi P., Lim J.-W., Smolinski K.M., Lawson K. Barriers to accessing quality health care for cancer patients: a survey of members of the association of oncology social work. Soc. Work Health Care. 2010;49:38–52. doi: 10.1080/00981380903018470. [DOI] [PubMed] [Google Scholar]
- Bush M.L., Kaufman M.R., Shackleford T. Adherence in the cancer care setting: a systematic review of patient navigation to traverse barriers. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 2018;33:1222–1229. doi: 10.1007/s13187-017-1235-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter E.B., Tuuli M.G., Caughey A.B., Odibo A.O., Macones G.A., Cahill A.G. Number of prenatal visits and pregnancy outcomes in low-risk women. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2016;36:178–181. doi: 10.1038/jp.2015.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond, S., 2020. Uber, Lyft Halt Shared Carpool Service In U.S. And Canada [WWW Document]. NPR.org. URL https://www.npr.org/2020/03/17/817240060/uber-lyft-halt-shared-carpool-service-in-u-s-and-canada (accessed 9.22.20).
- American Cancer Society, 2020. Road To Recovery Program [WWW Document]. Road Recovery. URL https://www.cancer.org/treatment/support-programs-and-services/road-to-recovery.html (accessed 11.3.20).
- Centers for Disease Control and Prevention, 2020. Framework for Healthcare Systems Providing Non-COVID-19 Clinical Care During the COVID-19 Pandemic [WWW Document]. URL https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html (accessed 7.9.20).
- Chaiyachati K.H., Hubbard R.A., Yeager A., Mugo B., Shea J.A., Rosin R., Grande D. Rideshare-based medical transportation for medicaid patients and primary care show rates: a difference-in-difference analysis of a pilot program. J. Gen. Intern. Med. 2018;33:863–868. doi: 10.1007/s11606-018-4306-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.E., Thadhani R.I., Maddux F.W. Adherence barriers to chronic dialysis in the United States. J. Am. Soc. Nephrol. JASN. 2014;25:2642–2648. doi: 10.1681/ASN.2013111160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, J., McGeorge, R., 2020. Spillover Effects Of The COVID-19 Pandemic Could Drive Long-Term Health Consequences For Non-COVID-19 Patients | Health Affairs Blog. Health Aff. Blog. URL https://www.healthaffairs.org/do/10.1377/hblog20201020.566558/full/ (accessed 2.20.21).
- Chen K.L., Wisk L.E., Nuckols T.K., Elmore J.G., Steers W.N., Zimmerman F.J. Unmet medical needs among adults who move due to unaffordable housing: California health interview survey, 2011–2017. J. Gen. Intern. Med. 2020 doi: 10.1007/s11606-020-06347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi N.G., Gonzalez J.M. Barriers and contributors to minority older adults’ access to mental health treatment. J. Gerontol. Soc. Work. 2005;44:115–135. doi: 10.1300/J083v44n03_08. [DOI] [Google Scholar]
- Cochran A.L. Impacts of COVID-19 on access to transportation for people with disabilities. Transp. Res. Interdiscip. Perspect. 2020;8 doi: 10.1016/j.trip.2020.100263. [DOI] [Google Scholar]
- Cohn, D., 2020. About a fifth of U.S. adults moved due to COVID-19 or know someone who did [WWW Document]. Pew Res. Cent. URL https://www.pewresearch.org/fact-tank/2020/07/06/about-a-fifth-of-u-s-adults-moved-due-to-covid-19-or-know-someone-who-did/ (accessed 7.30.20).
- Corallo, B., Tolbert, J., Rosenbaum, S., Sharac, J., Shin, P., 2020. Community Health Centers’ Role in Delivering Care to the Nation’s Underserved Populations During the Coronavirus Pandemic. KFF. URL https://www.kff.org/coronavirus-covid-19/issue-brief/community-health-centers-role-in-delivering-care-to-the-nations-underserved-populations-during-the-coronavirus-pandemic/ (accessed 2.19.21).
- Cummings J.R., Wen H., Ko M., Druss B.G. Race/ethnicity and geographic access to medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry. 2014;71:190–196. doi: 10.1001/jamapsychiatry.2013.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C.S., Samuels E.A. Opioid policy changes during the COVID-19 pandemic - and beyond. J. Addict. Med. 2020 doi: 10.1097/ADM.0000000000000679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drainoni M.-L., Lee-Hood E., Tobias C., Bachman S.S., Andrew J., Maisels L. Cross-disability experiences of barriers to health-care access: consumer perspectives. J. Disabil. Policy Stud. 2006;17:101–115. doi: 10.1177/10442073060170020101. [DOI] [Google Scholar]
- Dunlop A., Lokuge B., Masters D., Sequeira M., Saul P., Dunlop G., Ryan J., Hall M., Ezard N., Haber P., Lintzeris N., Maher L. Challenges in maintaining treatment services for people who use drugs during the COVID-19 pandemic. Harm. Reduct. J. 2020;17 doi: 10.1186/s12954-020-00370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberly L.A., Kallan M.J., Julien H.M., Haynes N., Khatana S.A.M., Nathan A.S., Snider C., Chokshi N.P., Eneanya N.D., Takvorian S.U., Anastos-Wallen R., Chaiyachati K., Ambrose M., O’Quinn R., Seigerman M., Goldberg L.R., Leri D., Choi K., Gitelman Y., Kolansky D.M., Cappola T.P., Ferrari V.A., Hanson C.W., Deleener M.E., Adusumalli S. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis, E., Knapp, S., Quan, J., Sutton, W., Regenstein, M., Shafi, T., Transit Cooperative Research Program, Transportation Research Board, National Academies of Sciences, Engineering, and Medicine Dialysis Transportation: The Intersection of Transportation and Healthcare 2019 Transportation Research Board Washington, D.C. 10.17226/25385. [DOI]
- Fisher M.D., Punekar R., Yim Y.M., Small A., Singer J.R., Schukman J., McAneny B.L., Luthra R., Malin J. Differences in health care use and costs among patients with cancer receiving intravenous chemotherapy in physician offices versus in hospital outpatient settings. J. Oncol. Pract. 2016;13:e37–e46. doi: 10.1200/JOP.2016.012930. [DOI] [PubMed] [Google Scholar]
- Fraade-Blanar, L., Whaley, C., 2020. Non-Emergency Medical Transportation in the Time of COVID-19. URL https://www.rand.org/blog/2020/05/non-emergency-medical-transportation-in-the-time-of.html (accessed 6.18.20).
- Garrett, B., Gangopadhyaya, A., 2020. How the COVID-19 Recession Could Affect Health Insurance Coverage (Brief). Robert Wood Johnson Foundation & Urban Institute, Washington D.C.
- Ghorbanzadeh M., Kim K., Ozguven E.E., Horner M.W. A comparative analysis of transportation-based accessibility to mental health services. Transp. Res. Part Transp. Environ. 2020;81 doi: 10.1016/j.trd.2020.102278. [DOI] [Google Scholar]
- Goodwin J.S., Hunt W.C., Samet J.M. A population-based study of functional status and social support networks of elderly patients newly diagnosed with cancer. Arch. Intern. Med. 1991;151:366–370. doi: 10.1001/archinte.1991.00400020114022. [DOI] [PubMed] [Google Scholar]
- Gray K.S., Cohen D.E., Brunelli S.M. In-center hemodialysis absenteeism: prevalence and association with outcomes. Clin. Outcomes Res. CEOR. 2017;9:307–315. doi: 10.2147/CEOR.S136577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath S. Mobile Health Clinics Traverse COVID-19’s Access to Care Gaps. PatientEngagementHIT. 2020 [Google Scholar]
- Henly M., Brucker D.L. Transportation patterns demonstrate inequalities in community participation for working-age Americans with disabilities. Transp. Res. Part Policy Pract. 2019;130:93–106. doi: 10.1016/j.tra.2019.09.042. [DOI] [Google Scholar]
- Henning-Smith C.E., Gonzales G., Shippee T.P. Barriers to timely medical care for older adults by disability status and household composition. J. Disabil. Policy Stud. 2016;27:116–127. doi: 10.1177/1044207316637547. [DOI] [Google Scholar]
- Health Center COVID-19 Survey [WWW Document]. URL https://bphc.hrsa.gov/emergency-response/coronavirus-health-center-data (accessed 7.6.20).
- Hu S., Chen P. Who left riding transit? Examining socioeconomic disparities in the impact of COVID-19 on ridership. Transp. Res. Part Transp. Environ. 2021;90 doi: 10.1016/j.trd.2020.102654. [DOI] [Google Scholar]
- Hubley S., Lynch S.B., Schneck C., Thomas M., Shore J. Review of key telepsychiatry outcomes. World J. Psychiatry. 2016;6:269–282. doi: 10.5498/wjp.v6.i2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikizler T.A., Kliger A.S. Minimizing the risk of COVID-19 among patients on dialysis. Nat. Rev. Nephrol. 2020;1–3 doi: 10.1038/s41581-020-0280-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankowski M. Lack of transportation leaves millions in need of substance abuse treatment on the sidelines. MobiHealthNews. 2019 [Google Scholar]
- Jiao J., Dillivan M. Transit deserts: the gap between demand and supply. J. Public Transp. 2013;16:23–39. doi: 10.5038/2375-0901.16.3.2. [DOI] [Google Scholar]
- Johnson A.A., Wesley B.D., El-Khorazaty M.N., Utter J.M., Bhaskar B., Hatcher B.J., Milligan R., Wingrove B.K., Richards L., Rodan M.F., Laryea H.A. African American and Latino patient versus provider perceptions of determinants of prenatal care initiation. Matern. Child Health J. 2011;15:27–34. doi: 10.1007/s10995-011-0864-z. [DOI] [PubMed] [Google Scholar]
- Johnson K., Goodnough A. Clinics for the Poor Face Drastic Cutbacks. N. Y; Times: 2020. Just When They’re Needed Most. [Google Scholar]
- Kakani P., Sorensen A., Quinton J.K., Han M., Ong M.K., Kamdar N., Sarkisian C.A. Patient characteristics associated with telemedicine use at a large academic health system before and after COVID-19. J. Gen. Intern. Med. 2021 doi: 10.1007/s11606-020-06544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy J., Wood E.G., Frieden L. Disparities in insurance coverage, health services use, and access following implementation of the affordable care act: a comparison of disabled and nondisabled working-age adults. Inq. J. Med. Care Organ. Provis. Financ. 2017;54 doi: 10.1177/0046958017734031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E.J., Marrast L., Conigliaro J. COVID-19: magnifying the effect of health disparities. J. Gen. Intern. Med. 2020;35:2441–2442. doi: 10.1007/s11606-020-05881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, J.-H., Desai, E., Cole, M.B., 2020. How The Rapid Shift To Telehealth Leaves Many Community Health Centers Behind During The COVID-19 Pandemic. Health Aff. Blog. URL https://www.healthaffairs.org/do/10.1377/hblog20200529.449762/full/ (accessed 7.6.20).
- Kishore S., Hayden M. Community health centers and Covid-19 — time for congress to act. N. Engl. J. Med. 2020;383 doi: 10.1056/NEJMp2020576. [DOI] [PubMed] [Google Scholar]
- Kohli P., Virani S.S. Surfing the waves of the COVID-19 pandemic as a cardiovascular clinician. Circulation. 2020;142:98–100. doi: 10.1161/CIRCULATIONAHA.120.047901. [DOI] [PubMed] [Google Scholar]
- Kutikov, A., Weinberg, D.S., Edelman, M.J., Horwitz, E.M., Uzzo, R.G., Fisher, R.I., 2020. A War on Two Fronts: Cancer Care in the Time of COVID-19. Ann. Intern. Med. 10.7326/M20-1133. [DOI] [PMC free article] [PubMed]
- Lê Cook, B., Alegría, M., 2011. Racial-Ethnic Disparities in Substance Abuse Treatment: The Role of Criminal History and Socioeconomic Status. Psychiatr. Serv. Wash. DC 62, 1273–1281. 10.1176/appi.ps.62.11.1273. [DOI] [PMC free article] [PubMed]
- Lê Cook B., Zuvekas S.H., Carson N., Wayne G.F., Vesper A., McGuire T.G. Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Serv. Res. 2014;49:206–229. doi: 10.1111/1475-6773.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levey N.N. Los Angel; Times: 2020. Coronavirus could change how you go to the doctor. [Google Scholar]
- Lin C.J., Schwaderer K.A., Morgenlander K.H., Ricci E.M., Hoffman L., Martz E., Cosgrove R.H., Heron D.E. Factors associated with patient navigators’ time spent on reducing barriers to cancer treatment. J. Natl. Med. Assoc. 2008;100:1290–1297. doi: 10.1016/S0027-9684(15)31507-8. [DOI] [PubMed] [Google Scholar]
- Manville M., Taylor B.D., Blumenberg E. California and Southern California. Southern California Association of Governments; 2018. Falling Transit Ridership. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin E., Shaheen S., Zohdy I. Federal Highway Administration; 2016. Understanding Travel Behavior: Research Scan. [Google Scholar]
- Mazul M.C., Salm Ward T.C., Ngui E.M. Anatomy of Good Prenatal Care: Perspectives of Low Income African-American Women on Barriers and Facilitators to Prenatal Care. J. Racial Ethn. Health Disparities. 2017;4:79–86. doi: 10.1007/s40615-015-0204-x. [DOI] [PubMed] [Google Scholar]
- Melnikow J., Paliescheskey M., Stewart G.K. Effect of a transportation incentive on compliance with the first prenatal appointment: A randomized trial. Obstet. Gynecol. 1997;89:1023–1027. doi: 10.1016/S0029-7844(97)00147-6. [DOI] [PubMed] [Google Scholar]
- Mennis J., Stahler G.J., Baron D.A. Geographic barriers to community-based psychiatric treatment for drug-dependent patients. Ann. Assoc. Am. Geogr. 2012;102:1093–1103. doi: 10.1080/00045608.2012.657142. [DOI] [Google Scholar]
- Norris K.C., Williams S.F., Rhee C.M., Nicholas S.B., Kovesdy C.P., Kalantar-Zadeh K., Boulware L.E. Hemodialysis disparities in african americans: the deeply integrated concept of race in the social fabric of our society. Semin. Dial. 2017;30:213–223. doi: 10.1111/sdi.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obialo C.I., Hunt W.C., Bashir K., Zager P.G. Relationship of missed and shortened hemodialysis treatments to hospitalization and mortality: observations from a US dialysis network. Clin. Kidney J. 2012;5:315–319. doi: 10.1093/ckj/sfs071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien P., Crable E., Fullerton C., Hughey L. U.S; Department of Health and Human Services, Washington, D.C.: 2019. Best Practices and Barriers to Engaging People with Substance Use Disorders in Treatment. [Google Scholar]
- Office of Disease Prevention and Health Promotion, 2020. Maternal, Infant, and Child Health: MICH-10.2 Increase the proportion of pregnant women who receive early and adequate prenatal car [WWW Document]. Healthy People 2020. URL https://www.healthypeople.gov/2020/data-search/Search-the-Data#objid=4834 (accessed 7.3.20).
- Palmer R.S., Murphy M.K., Piselli A., Ball S.A. Substance abuse treatment drop-out from client and clinician perspectives. Subst. Use Misuse. 2009;44:1021–1038. doi: 10.1080/10826080802495237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel S.Y., Mehrotra A., Huskamp H.A., Uscher-Pines L., Ganguli I., Barnett M.L. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff. (Millwood) 2021;40:349–358. doi: 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peahl, A.F., 2020. Prenatal Care During the COVID-19 Pandemic: Prenatal Patient Resources [WWW Document]. Univ. Mich. Obstet. Gynecol. URL https://medicine.umich.edu/dept/obgyn/patient-care-services/prenatal-care-during-covid-19-pandemic-prenatal-patient-resources (accessed 7.3.20).
- Peart A., Lewis V., Brown T., Russell G. Patient navigators facilitating access to primary care: a scoping review. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-019252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen, E.E., 2019. Racial/Ethnic Disparities in Pregnancy-Related Deaths — United States, 2007–2016. MMWR Morb. Mortal. Wkly. Rep. 68. 10.15585/mmwr.mm6835a3. [DOI] [PMC free article] [PubMed]
- Phillips S.S., Tom L.S., Bularzik C., Simon M.A. Time and motion study of a community patient navigator. AIMS Public Health. 2014;1:51–59. doi: 10.3934/publichealth.2014.2.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priest, K., 2020. The COVID-19 Pandemic: Practice And Policy Considerations For Patients With Opioid Use Disorder. Health Aff. Blog. URL https://www.healthaffairs.org/do/10.1377/hblog20200331.557887/full/ (accessed 7.24.20).
- Rall, J., Myers, A., 2015. State Human Service Transportation Coordinating Councils: An Overview and State Profiles. National Conference of State Legislatures, Washington, D.C.
- Riley S., Riley C. The role of patient navigation in improving the value of oncology care|Journal of Clinical Pathways. J. Clin. Pathways. 2016;2:41–47. [Google Scholar]
- Rodriguez J., Betancourt J.R., Sequist T.D., Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am. J. Manage. Care. 2021;27:21–26. doi: 10.37765/ajmc.2021.88573. 10.37765/ajmc.2021.88573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen D., Tolman R.M., Warner L.A. Low-income women’s use of substance abuse and mental health services. J. Health Care Poor Underserved. 2004;15:206–219. doi: 10.1353/hpu.2004.0028. [DOI] [PubMed] [Google Scholar]
- Rozenfeld Y., Beam J., Maier H., Haggerson W., Boudreau K., Carlson J., Medows R. A model of disparities: risk factors associated with COVID-19 infection. Int. J. Equity Health. 2020;19:126. doi: 10.1186/s12939-020-01242-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamshiripour, A., Rahimi, E., Shabanpour, R., Mohammadian, A. (Kouros), 2020. How is COVID-19 reshaping activity-travel behavior? Evidence from a comprehensive survey in Chicago. Transp. Res. Interdiscip. Perspect. 7, 100216. 10.1016/j.trip.2020.100216. [DOI] [PMC free article] [PubMed]
- Shelby R.A., Taylor K.L., Kerner J.F., Coleman E., Blum D. The role of community-based and philanthropic organizations in meeting cancer patient and caregiver needs. CA. Cancer J. Clin. 2002;52:229–246. doi: 10.3322/canjclin.52.4.229. [DOI] [PubMed] [Google Scholar]
- Shierholz H. Econ. Policy Inst. Work. Econ; Blog: 2020. At least 33 million workers are being hurt by the coronavirus recession. https://www.epi.org/blog/at-least-33-million-workers-are-being-hurt-by-the-coronavirus-recession/ (accessed 11.10.20) [Google Scholar]
- Siegel D.A., O’Neil M.E., Richards T.B., Dowling N.F., Weir H.K. Prostate Cancer Incidence and Survival, by Stage and Race/Ethnicity — United States, 2001–2017. Morb. Mortal. Wkly. Rep. 2020;69:1473–1480. doi: 10.15585/mmwr.mm6941a1. 10.15585/mmwr.mm6941a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon E.M., Wing H., Steiner J.F., Gottlieb L.M. Impact of Transportation Interventions on Health Care Outcomes: A Systematic Review. Med. Care. 2020;58:384–391. doi: 10.1097/MLR.0000000000001292. [DOI] [PubMed] [Google Scholar]
- Stitzenberg K.B., Sigurdson E.R., Egleston B.L., Starkey R.B., Meropol N.J. Centralization of cancer surgery: implications for patient access to optimal care. J. Clin. Oncol. 2009;27:4671–4678. doi: 10.1200/JCO.2008.20.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed S.T., Gerber B.S., Sharp L.K. Traveling towards disease: transportation barriers to health care access. J. Community Health. 2013;38:976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The American College of Obstetricians and Gynecologists, 2020. COVID-19 FAQs for Obstetrician-Gynecologists, Telehealth [WWW Document]. URL https://www.acog.org/en/Clinical Information/Physician FAQs/COVID 19 FAQs for Ob Gyns Telehealth (accessed 6.23.20).
- Tolbert, J., Orgera, K., Damico, A., 2020. Key Facts about the Uninsured Population. Kais. Fam. Found. URL https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/ (accessed 11.10.20).
- TransitCenter, 2020. Transit Is Essential: 2.8 Million U.S. Essential Workers Ride Transit to Their Jobs [WWW Document]. TransitCenter Blog. URL https://transitcenter.org/2-8-million-u-s-essential-workers-ride-transit-to-their-jobs/ (accessed 2.25.21).
- NPR/Robert Wood Johnson Foundation/Harvard T.H. Chan School of Public Health, 2020. The Impact of Coronavirus on Households Across America. Harvard University. URL https://cdn1.sph.harvard.edu/wp-content/uploads/sites/94/2020/09/NPR-RWJF-Harvard-National-Report_092220_Final-1.pdf (accessed 02.26.2021).
- United States Renal Data System, 2019. Chapter 1: Incidence, Prevalence, Patient Characteristics, and Treatment Modalities. Am. J. Kidney Dis. 73, S291–S332. 10.1053/j.ajkd.2018.12.012. [DOI]
- Unützer J., Park M. Strategies to improve the management of depression in primary care. Prim. Care. 2012;39:415–431. doi: 10.1016/j.pop.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau, 2020a. Phase 1 Interactive Data Tool Indicators., Phase 1 Household Pulse Survey: April 23 - July 21. Phase 1 Household Pulse Survey: April 23 - July 21.
- U.S. Census Bureau, 2020b. Table 1. Coronavirus Pandemic Related Problems with Access to Medical Care, in Last 4 Weeks, by Select Characteristics, Week 17 Household Pulse Survey: October 14-October 26.
- U.S. Census Bureau, 2020c. Table S1810: Disability Characteristics, 2018 American Community Survey, 5-Year Estimates.
- U.S. Department of Health and Human Services, 2020. Telehealth: Delivering Care Safely During COVID-19 [WWW Document]. URL https://www.hhs.gov/coronavirus/telehealth/index.html (accessed 11.3.20).
- Verma A., Patel A.B., Tio M.C., Waikar S.S. Caring for dialysis patients in a time of COVID-19. Kidney Med. 2020 doi: 10.1016/j.xkme.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Highway Administration, 2020. 2017 National Household Travel Survey, Version 1.2. United States Department of Transportation. URL https://nhts.ornl.gov/.
- Verma, P., 2020. Public Transit Officials Fear Virus Could Send Systems Into ‘Death Spiral.’ N. Y. Times.
- Wallace, R., Hughes-Cromwick, P., Mull, H., 2006. Cost-Effectiveness of Access to Nonemergency Medical Transportation: Comparison of Transportation and Health Care Costs and Benefits. Transp. Res. Rec. 10.1177/0361198106195600111. [DOI]
- Weber Handwerker, E., Meyer, P.B., Piacentini, J., Schultz, M., Sveikauskas, L., 2020. Employment recovery in the wake of the COVID-19 pandemic, Monthly Labor Review. U.S. Bureau of Labor Statistics.
- Whaibeh E., Mahmoud H., Naal H. Telemental Health in the Context of a Pandemic: the COVID-19 Experience. Curr. Treat. Options Psychiatry. 2020;1–5 doi: 10.1007/s40501-020-00210-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whetten R., Whetten K., Pence B.W., Reif S., Conover C., Bouis S. Does distance affect utilization of substance abuse and mental health services in the presence of transportation services? AIDS Care. 2006;18:27–34. doi: 10.1080/09540120600839397. [DOI] [PubMed] [Google Scholar]
- Wicklund, E., 2020. A Pandemic Gives Telehealth a New Purpose With Community Paramedicine [WWW Document]. mHealthIntelligence. URL https://mhealthintelligence.com/news/a-pandemic-gives-telehealth-a-new-purpose-with-community-paramedicine (accessed 2.19.21).
- Wolf L.A., Armour B.S., Campbell V.A. Racial/Ethnic Disparities in Self-Rated Health Status Among Adults With and Without Disabilities -- United States, 2004 -2006. MMWR Morb Mortal Wkly Rep. 2008;57:1069–1073. [PubMed] [Google Scholar]
- Wolfe M.K., McDonald N.C. Innovative health care mobility services in the US. BMC Public Health. 2020;20 doi: 10.1186/s12889-020-08803-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolhandler S., Himmelstein D.U. Intersecting U.S. Epidemics: COVID-19 and Lack of Health Insurance. Ann. Intern. Med. 2020 doi: 10.7326/M20-1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Landrum M.B., Zhou L., Busch A.B. Disparities in outpatient visits for mental health and/or substance use disorders during the COVID surge and partial reopening in Massachusetts. Gen. Hosp. Psychiatry. 2020;67:100–106. doi: 10.1016/j.genhosppsych.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang R.L., Wapnir I. Hispanic breast cancer patients travel further for equitable surgical care at a comprehensive cancer center. Health Equity. 2018;2:109–116. doi: 10.1089/heq.2017.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yedjou C.G., Sims J.N., Miele L., Noubissi F., Lowe L., Fonseca D.D., Alo R.A., Payton M., Tchounwou P.B. Health and racial disparity in breast cancer. Adv. Exp. Med. Biol. 2019;1152:31–49. doi: 10.1007/978-3-030-20301-6_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yerram P., Misra M. Home Dialysis in the Coronavirus Disease 2019 Era. Adv. Chronic Kidney Dis. 2020;27:442–446. doi: 10.1053/j.ackd.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zullig L.L., Jackson G.L., Provenzale D., Griffin J.M., Phelan S., van Ryn M. Transportation – A Vehicle or Roadblock to Cancer Care for VA Colorectal Cancer Patients? Clin. Colorectal Cancer. 2012;11:60–65. doi: 10.1016/j.clcc.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]