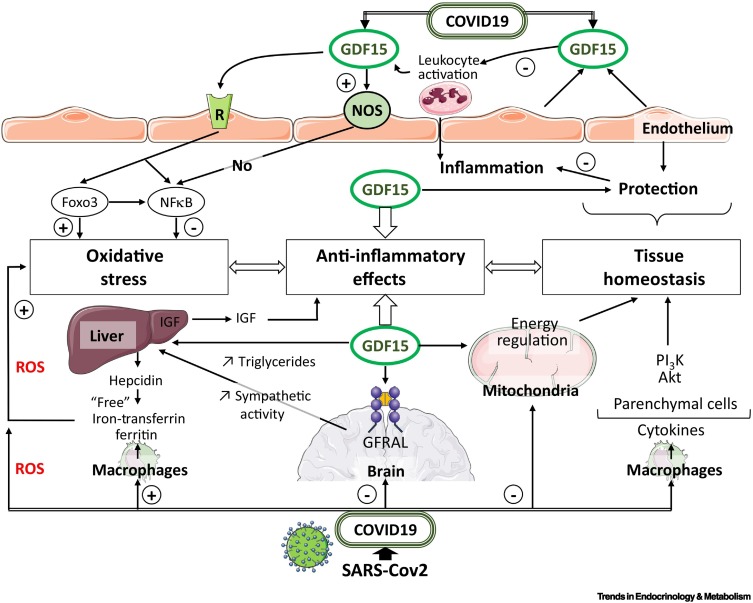
Figure 3.
Pathways contributing to hyperinflammation in coronavirus disease 2019 (COVID-19) and anti-inflammatory effects of growth and differentiation factor 15 (GDF15).
Activated monocyte-derived macrophages contribute to the COVID-19 cytokine storm by releasing massive amounts of proinflammatory cytokines. Macrophage activation and iron metabolism are implicated in COVID-19 infection. The cytokine storm observed in patients with COVID-19 contributes to the endothelial vascular dysfunction inducing endothelialitis. Activated monocytes are recruited to endothelial cells, which are activated by cytokines and produce monocyte chemoattractants and adhesion molecules. During COVID-19, GDF15 is induced and takes into a tissue-protective effect, indicating GDF15 as an inflammation-induced central mediator of tissue tolerance. Cellular stress, and chronic inflammation associated with COVID-19 infection induce the secretion and release of GDF15, which appears in the blood to target specific receptors. GDF15 binds to glial-derived neurotrophic factor (GDNF)-family receptor α-like (GFRAL) in the brain. GDF15 exerts direct effects on immune cells independent of centrally regulated mechanisms and has the potential to affect the outcome of COVID-19 infection as an emerging modulator of immune responses. The GDF15–GFRAL complex mediates the regulation of central and peripheral functions, resulting in activation of nitric oxide synthase (NOS), PI3K/AKT, nuclear factor κB (NF-κB)and the forkhead box (FOX) transcription factors in Foxo3 pathways. These pathways are essential in regulating cellular controls on tissue homeostasis and anti-inflammatory effects. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can trigger disruption of the balance between pro-oxidant and antioxidant mediators; the magnitude of the oxidative stress could reflect the severity of infection and lung injury. Liver injury is common in patients with COVID-19. Interactions occur during the inflammatory process, oxidative stress, iron metabolism, and hepatic functions through ferritin and hepcidin. Moreover, labile iron can promote inflammation by increased production of reactive oxygen species (ROS). Insulin-like growth factor 1 (IGF1), synthesized primarily in the liver, acts as an important modulator of cellular functions. Growth hormone (GH) secreted from the pituitary gland sends signals to the liver to stimulate the production of IGF1. Circulating GDF15 levels influence the liver to inhibit the actions of GH. COVID19-associated multiorgan failure is linked to impaired mitochondrial function. Mitochondria localization may be necessary for SARS-CoV-2 replication.