Abstract
Background and Objectives
The rapid scale‐up of telehealth services for substance use disorders (SUDs) during the COVID‐19 pandemic presented a unique opportunity to investigate patient experiences with telehealth. This study examined patient perceptions of telehealth in an outpatient SUD treatment program offering individual therapy, group therapy, and medication management.
Methods
Two hundred and seventy adults receiving SUD outpatient treatment were eligible to complete a 23‐item online survey distributed by clinicians; 58 patients completed/partially completed the survey. Data were summarized with descriptive statistics.
Results
Participants were predominately male, White, and well‐educated. The majority (86.2%) were “very satisfied” or “satisfied” with the quality of telehealth care. “Very satisfied” ratings were highest for individual therapy (90%), followed by medication management (75%) and group therapy (58%). Top reasons for liking telehealth included the ability to do it from home (90%) and not needing to spend time commuting (83%). Top reasons for disliking telehealth were not connecting as well with other members in group therapy (28%) and the ability for telehealth to be interrupted at home or work (26%).
Discussion and Conclusions
Telehealth visits were a satisfactory treatment modality for most respondents receiving outpatient SUD care, especially those engaging in individual therapy. Challenges remain for telehealth group therapy.
Scientific Significance
This is the first study examining patients' perceptions of telehealth for outpatient SUD treatment during the COVID‐19 pandemic by treatment service type. Importantly, while many participants found telehealth more accessible than in‐person treatment, there was variability with respect to the preferred mode of treatment delivery.
INTRODUCTION
The expansion of telehealth care for substance use disorder (SUD) treatment has the potential to address longstanding gaps in the receipt of care; only 10.3% of people in the United States with SUDs received treatment in 2019.1 Although the use of telehealth for SUD treatment has been growing over the past 10 years, this growth has occurred at a much slower pace than that for other mental health conditions.2, 3 Obstacles include a more limited evidence base for its efficacy in treating SUDs4 (compared to that for other mental health conditions), and for opioid use disorder (OUD) care specifically, the Ryan Haight Online Pharmacy Consumer Protection Act of 2008, a federal law requiring an in‐person visit to prescribe controlled substances, such as buprenorphine.5
The onset of the COVID‐19 pandemic in the United States brought about a tremendous growth in the use of telehealth across a range of healthcare providers and medical conditions; starting with the federally declared state of emergency in March 2020, in‐person visits decreased dramatically.6, 7, 8 Telehealth enabled providers to maintain patient care while minimizing in‐person visits in an effort to slow the spread of the coronavirus. The rapid uptake of telehealth was further aided by the relaxation of federal, state, and health insurance regulations and payment practices that were more restrictive prior to the pandemic.9, 10 In particular, an emergency exemption was granted to the Ryan Haight Act, which allowed providers to prescribe controlled substances via telehealth without an in‐person visit.11
There is a robust evidence base that demonstrates that telehealth is at least as effective as in‐person care for several behavioral health conditions—particularly for depression and anxiety disorders.12, 13, 14, 15, 16 There is also evidence that patients with behavioral health conditions are generally satisfied with telehealth, both in terms of the patient clinical experience and benefits of improved access to and convenience of care.17 Prior studies of patient perceptions of telehealth, specifically for SUD care, have shown high levels of patient satisfaction with telehealth treatment that are comparable with in‐person treatment.4, 18, 19 However, the existing literature examining SUD care via telehealth is more limited than for other behavioral health conditions, and the quality of the evidence of these studies is variable.4 Moreover, these studies typically examined a singular treatment modality, and the prior literature does not distinguish whether patients might have different perceptions of their experiences in telehealth care based on the type of SUD treatment service. For example, patients may have different experiences/preferences for the delivery of initial assessments, medication management visits, or individual or group therapy, due to the variability in the level of interpersonal interaction and engagement across these service types.
The present study addresses these limitations in the existing literature by examining patient satisfaction across three treatment modalities for patients seeking treatment for a range of SUDs. The aim of this study is to examine the experiences of patients receiving SUD treatment via synchronous video conferencing telehealth during the COVID‐19 pandemic in an outpatient SUD treatment program, as part of routine care.
METHODS
Setting
Participants were recruited from McLean Hospital's outpatient Alcohol, Drug, and Addiction Treatment Program (ADATP). McLean Hospital is a free‐standing psychiatric hospital near Boston that is part of the Mass General Brigham (formerly Partners HealthCare) health system. The ADATP has approximately 4000 outpatient visits per year.
On March 16, 2020, due to the federal and state declared state of emergency related to COVID‐19, McLean Hospital clinicians were mandated to discontinue in‐person outpatient visits. Clinicians were initially told to maintain phone contact with patients, as the hospital quickly began to set up the capacity to conduct telehealth video visits. Within 2 weeks, the hospital had provisioned its outpatient providers with telehealth video software and training on procedures and technical expertise needed to protect the privacy and security of the patient encounters. By April, McLean had completely transitioned to telehealth, largely conducted by video visits. ADATP outpatient encounters increased during this time, but this is at least partially explained by the fact that as the hospital transitioned to virtual care, the ADATP's partial hospital program transitioned to an outpatient program in which patients could choose from a recommended menu of outpatient services (i.e., individual therapy, group therapy, or individual medical management visits) at a greater frequency than traditional outpatient care. In addition, there was an increase in case management via phone and a cessation of urine toxicology screens due to stay‐at‐home orders.
Participants and procedures
Participants were included in this study if they were 18 years or older and currently engaged in outpatient telehealth treatment in the ADATP.
All study procedures were approved by the Mass General Brigham Institutional Review Board (IRB). The IRB waived the requirement for written informed consent for this study. Participants were informed about the purpose, content, and risks and benefits of the study via a study fact sheet, and eligible subjects indicated their agreement to participate in the study by clicking on a checkbox next to the statement “I agree to participate in this research.”
Clinicians in the ADATP sent a link to the study fact sheet and survey to their current patients enrolled in outpatient treatment. Prior to reviewing the study fact sheet, participants completed prescreening questions to confirm that they were 18 years or older and that they had not previously completed the survey. The survey was active from June 8, 2020 to July 12, 2020. During that time period, there were 270 unique patients in the ADATP. All clinicians were encouraged to invite their patients to complete the survey. We were unable to collect data on the precise numbers of patients who were invited by their clinicians to complete the survey. Participants did not receive any remuneration for participating in the study.
Seventy‐six patients completed prescreening questions, and 65 patients consented to participate in the study. Seven participants did not complete any questions after consenting; therefore, data were analyzed for the 58 participants who completed or partially completed the survey. Descriptive statistics (frequencies, means, and standard deviations) were used to summarize the survey data. Pairwise correlation was used to examine the association between satisfaction with telehealth and length of time in treatment.
Measures
Participants completed the Telehealth Patient Survey, a 23‐item self‐report survey focused on measuring participants' experiences with telehealth in the ADATP. Our focus was on understanding patient experiences with video visits, therefore in the survey instructions participants were informed, “We would like to better understand your experience using Zoom for telehealth.” Questions were derived from the McLean Anxiety Mastery Program Telehealth Satisfaction Questionnaire20 and assessed the frequency and type of services received via telehealth, as well as satisfaction with telehealth for each treatment service, preference for service delivery type (e.g., telehealth, in‐person, a mix of both, no preference), factors they liked and disliked about telehealth, and technical issues accessing telehealth. In addition, participants were asked questions about their demographic characteristics, such as age, gender, and education, and questions about their current substance use.
RESULTS
Demographic and substance use characteristics are summarized in Table 1. The sample was primarily male (66%), White (92%), and well‐educated (45% completed post‐graduate education). Alcohol (59%) was most commonly identified as the substance that had caused participants the most difficulties lately.
Table 1.
Demographics and substance use characteristics (N = 53a)
| Age (years), mean (SD) | 45.5 (14.5) |
| Range | 22–78 |
| Gender, n (%) | |
| Male | 35 (66.0) |
| Female | 18 (34.0) |
| Education, n (%) | |
| High school or less | 4 (7.5) |
| Some college | 10 (18.9) |
| Completed college | 15 (28.3) |
| Post‐graduate | 24 (45.3) |
| Employment, n (%) | |
| Employed full‐time | 23 (43.4) |
| Employed part‐time | 3 (5.7) |
| Unemployed/furloughed/homemaker | 11 (20.8) |
| Retired | 9 (17.0) |
| Disabled | 4 (7.5) |
| Student | 3 (5.7) |
| Race,a n (%) | |
| White | 47 (92.2) |
| Black | 3 (5.9) |
| Asian | 1 (2.0) |
| Hispanic/Latino,a n (%) | 2 (3.8) |
| Substance that has caused the most difficulties lately, n (%) | |
| Alcohol | 31 (58.5) |
| Prescription opioids | 8 (15.1) |
| Other opioids | 4 (7.5) |
| Cocaine | 1 (1.9) |
| Methamphetamine | 1 (1.9) |
| Cannabis | 2 (3.8) |
| No substance difficulties lately | 6 (11.3) |
| Smoking status, n (%) | |
| Smoke cigarettes or other tobacco | 13 (24.5) |
| Vaped in the past month | 6 (11.3) |
Five participants did not complete the demographic and substance use questions. Two additional participants chose not to report their race and one additional participant declined to report ethnicity.
Most participants (78%) were engaged in group therapy; just over half (52%) were receiving individual therapy and 41% were receiving medication management. Few participants (n = 5, 8.6%) reported that they had ever received telehealth treatment services prior to COVID‐19. Very few participants (n = 2, 3.5%) reported having difficulty logging into the telehealth platform; 95% were “satisfied” or “very satisfied” with the sound quality and 86% were “satisfied” or “very satisfied” with the video quality of the telehealth program. Five participants (8.6%) clicked “not applicable” in response to the video quality question, suggesting that these participants were engaged in audio‐only telehealth visits. Table 2 provides descriptive data on telehealth receipt and satisfaction.
Table 2.
Telehealth characteristics (N = 58)
| N (%) | |
|---|---|
| ADATP treatment status | |
| Receiving in‐person treatment before COVID‐19 telehealth | 48 (82.8) |
| Started treatment after transitioning to COVID‐19 telehealth | 10 (17.2) |
| Length of ADATP telehealth treatment | |
| 1–2 weeks | 3 (5.2) |
| 3–4 weeks | 4 (6.9) |
| 5–6 weeks | 19 (32.8) |
| 7+ weeks | 32 (55.2) |
| Frequency of telehealth visits | |
| Once/day | 3 (5.2) |
| Once/week | 28 (48.3) |
| More than once/week | 15 (25.9) |
| More than once/week but less than once/month | 5 (8.6) |
| Once/month or less | 7 (12.0) |
| Ease of logging into telehealtha | |
| Somewhat difficult | 2 (3.5) |
| Neither easy/difficult | 1 (1.8) |
| Somewhat easy | 9 (15.8) |
| Very easy | 45 (78.9) |
| The things I like about telehealth | |
| I can do it from home | 52 (89.7) |
| I don't need to spend time driving and parking or taking public transportation | 48 (82.8) |
| I don't have to sit in a waiting room | 26 (44.8) |
| I don't have to leave work | 20 (34.5) |
| It is easier to find an appointment time | 19 (32.8) |
| It makes childcare or other caretaking responsibilities easier | 13 (22.4) |
| It is easier to talk to my therapist by telehealth | 9 (15.5) |
| It is more confidential | 7 (12.1) |
| I can smoke or use other nicotine or tobacco products | 3 (5.2) |
| I like the fact that people can't see my whole body, just my face | 2 (3.4) |
| I don't like anything about telehealth | 1 (1.7) |
| The things that I don't like about telehealth | |
| There is nothing I dislike about telehealth | 23 (39.7) |
| I don't connect as well with other group members in group therapy | 16 (27.6) |
| I can get interrupted at home/work | 15 (25.9) |
| I like the idea of getting out of the house to go to the clinic | 11 (18.9) |
| I am more likely to discuss difficult topics in person | 10 (17.2) |
| I don't connect as well with my therapist | 9 (15.5) |
| I don't have privacy at home/work | 8 (13.8) |
| I like the idea of a break in my workday to go to the clinic | 5 (8.6) |
| I don't like the idea of just seeing the face of my therapist | 5 (8.6) |
| I feel safer in person | 4 (6.9) |
| I don't have a good enough computer or wi‐fi, the video or sound isn't good | 3 (5.2) |
Abbreviation: ADATP, Alcohol, Drug, and Addiction Treatment Program.
One response missing.
The majority of participants (86.2%) reported that they were “very satisfied” or “satisfied” with the quality of telehealth care. In addition, 82% of the sample indicated telehealth visits met their needs “equally well” or “better” than in‐person visits. Satisfaction was not significantly correlated with length of time in telehealth treatment (r = .108, n = 58, p = .421). Of participants who received these services, a majority reported feeling “very satisfied” with individual therapy (90%) and individual medication management (75%). In contrast, only 58% of participants who received group therapy were “very satisfied” with receiving this service via telehealth (Figure 1).
Figure 1.
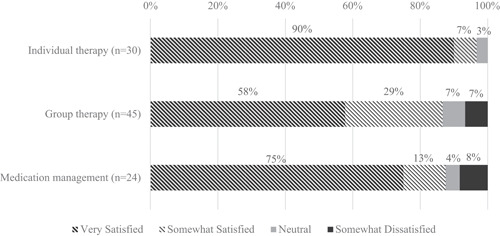
Telehealth satisfaction by treatment type
The preferred mode of treatment delivery was varied (Figure 2). Despite strong ratings of satisfaction, only 36% of participants reported a strong or slight preference for individual therapy via telehealth; 43% and 48% preferred group therapy and medication management visits via telehealth, respectively. Preference (strong or slight) for in‐person individual treatment was equivalent to those preferring individual telehealth (36%), and ratings for in‐person group therapy and medication management were lower than for telehealth delivery of these services. A smaller percentage of participants favored a mix of telehealth and in‐person services (25% for individual therapy, 19% for group therapy, and 22% for medication management).
Figure 2.
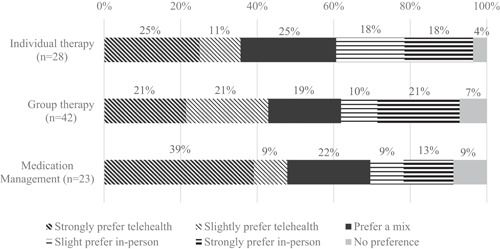
Preferred mode of treatment delivery by treatment type
Participants were asked what they liked and disliked about telehealth (Table 2). Most participants indicated that they liked accessing treatment from home (90%) and that they did not need to dedicate time to traveling to appointments (83%). There was less consensus regarding aspects they disliked. Forty percent of the sample indicated there was nothing they disliked about telehealth. Among the 60% who listed factors that they disliked about telehealth, top‐rated reasons were that they did not connect as well with other group members (28%), they could get interrupted at home or work (26%), and they preferred leaving home to go to the clinic (19%). Of note, not all participants received group therapy. Of those who reported engaging in group therapy, 36% reported that they did not connect as well with other group members via telehealth.
DISCUSSION
This study examined patients' experiences with the rapid scale‐up of SUD telehealth services during the COVID‐19 pandemic in one SUD outpatient clinic. Overall, patients reported high levels of satisfaction with telehealth care. However, when we looked at satisfaction by service type, most participants reported that they were very satisfied with individual therapy and medication management, but less than 60% of people who received group therapy were very satisfied. Although group therapy delivered via telehealth has been shown to be feasible and associated with treatment outcomes similar to in‐person group treatment, there is some evidence of decreased therapeutic alliance for group telehealth treatment compared to in‐person treatment.21, 22 Similarly, in this study, over a quarter of participants indicated that they did not connect as well with other group members in group telehealth therapy, and this was the most commonly reported telehealth factor disliked by participants.
In this study, satisfaction with telehealth overall was quite strong, with over 85% reporting that they were satisfied or very satisfied with services and over 80% reporting that telehealth met their needs at least as well as in‐person care. Despite high ratings of satisfaction for telehealth for individual therapy, only 36% chose telehealth as their preferred mode of treatment delivery. Interestingly, although fewer participants were highly satisfied with group therapy compared with individual therapy (58% vs. 90%, respectively), people were slightly more likely to express a preference for telehealth delivery of group therapy than for individual therapy (43% vs. 36%, respectively). It is possible that this reflects a difference in satisfaction with group compared to individual treatment overall, such that participants are less satisfied with group therapy than individual therapy regardless of whether it is delivered in person or remotely. Nonetheless, this should be interpreted with caution because formal tests comparing these preferences were not conducted in this study. A stronger preference for medication management visits via telehealth may reflect the convenience of avoiding the need to commute to attend a brief appointment. There are likely additional factors that contribute to patient preference beyond treatment satisfaction, such as motivation to engage in the treatment, competing responsibilities (work, childcare, etc.), and availability and ease of transportation. Additional exploration of the factors that contribute to preference of treatment delivery is warranted.
When considering preference for mode of treatment delivery, it is notable that in addition to those who preferred telehealth, 19%–25% preferred a mix of telehealth and in‐person treatment. Therefore, another way to consider these results is that the majority of participants preferred care that included telehealth—either as their sole mode of treatment or as some part of their care combined with in‐person treatment. When the mode of treatment delivery is not dictated by COVID‐19 safety guidelines, it will be important to understand how best to offer telehealth to patients (hybrid or sole mode of treatment), and which individual treatment characteristics to consider.
In addition, while we did not find that satisfaction scores were associated with the duration of telehealth services, it is notable that the majority of participants in our sample (83%) were engaged in SUD treatment in the ADATP prior to the transition to telehealth. Therefore, it is possible that these patients were already established and connected to their treatment provider(s), which may have facilitated the transition to telehealth. There is some evidence of reduced group cohesion and patient‐reported therapeutic alliance with group telehealth for posttraumatic stress disorder.21 It is possible that therapeutic alliance may vary not only by individual differences in the ability to establish an alliance23 but that those with already established providers may find therapeutic alliance more durable with a transition to telehealth than those with new providers.
One of the key potentials of telehealth is in increasing access to care for individuals who have difficulty accessing in‐person treatment services. Few participants in this sample were new to treatment (n = 10); therefore, we were unable to examine whether preferences and satisfaction for telehealth differed for those established in treatment compared with patients new to treatment. For example, telehealth might be more likely to be rated as the preferred mode of treatment delivery in participants who have little to no access to in‐person treatment, compared with those who have equal access to both telehealth and in‐person care. Insurance coverage of telehealth will also likely influence patient preferences for its use. Pre‐pandemic, insurance coverage for telehealth was more limited2, 24 and the future state of insurance coverage for telehealth is an active and unsettled area of health policy. Future research should examine the role of insurance status and type in preferences for telehealth care.
Twelve individuals in this sample (23%) endorsed opioids as the substance that had caused them the most difficulties lately, yet only two of the twelve started treatment in the ADATP after the switch to telehealth. Although regulatory restrictions around prescribing medication treatment for OUD were relaxed in response to COVID‐19, an analysis of data from commercially insured patients found that during the first three months of the pandemic, fewer individuals initiated medication treatment for an OUD compared to the same time period the prior year.8 A qualitative study of clinicians' experiences with telehealth during COVID‐19 revealed that clinicians felt they were able to maintain current OUD patients via telehealth, but they were less comfortable initiating new patients on medication for OUD via telehealth visits.25 If the changes to the Ryan Haight Act remain in place post‐pandemic, it will be important to further understand clinicians' discomfort with telehealth for initiating medication treatment for OUD and to develop guidelines and strategies to address these concerns.
In this sample, patients' reasons for liking telehealth centered around the convenience of accessing treatment from home. There was much less consensus around what patients dislike about telehealth treatment. However, it is important to acknowledge that even for patients who can easily access telehealth care and are seemingly satisfied with telehealth, there were negative factors reported by a subgroup of patients that could affect their treatment. In addition to trouble connecting with group members, 15% of participants reported that they do not connect as well with their therapist via telehealth, and 17% reported that they are more likely to discuss difficult topics in person. Clinicians need to be aware of these potential barriers to treatment. In a recent survey study of clinicians engaged in telehealth for mental health and SUD care, clinicians expressed the importance of discussing with patients the differences between telehealth and in‐person treatment and helping patients process their feelings about telehealth treatment.26 Although few participants reported that they dislike telehealth because they feel safer in person, in light of concerns of increases in intimate partner violence during the COVID‐19 pandemic,27, 28 it is critical for clinicians to assess patient safety.
Racial and ethnic minorities, and those living in poverty encounter more barriers related to accessing telehealth care.29, 30 Participants in this study were predominately White and well‐educated. Moreover, few participants reported issues with logging into the telehealth platform, and only three participants indicated that they did not have a good enough computer or wi‐fi access. It is likely that the sociodemographic characteristics of this sample facilitated an easier transition to telehealth treatment, contributing to patient's high levels of satisfaction. Enthusiasm for telehealth needs to be countered with careful examination of inequities in digital health access. Adequate technology and high‐speed internet access are important for reducing barriers for underserved populations, as well as training for providers in competencies to provide equitable digital health care. The Digital Health Equity Framework proposed by Crawford and Serhal31 stresses the importance of stakeholders at all levels of the health care system (i.e., providers, institutions, insurers, and government) to understand and work toward improving resources to reduce disparities in digital health access.
There are several limitations to this study. First, this is a single‐clinic study, and the sample size is small and not diverse with respect to race and ethnicity. Therefore these findings may not generalize to other clinics and populations. In addition, we recruited participants for this study who were already engaged in telehealth treatment, and thus, by nature, had already overcome initial barriers to access. Second, likes and dislikes were measured as a binary response, rather than a Likert scale; therefore, we were unable to assess the degree to which participants liked or disliked each of the items. In addition, although some of the items implied comparison with in‐person treatment (e.g., I don't connect as well with other group members in group therapy), we did not assess the likes/dislikes of in‐person treatment to make direct comparisons. Third, we do not know how representative the sample is of the total ADATP outpatient treatment population, as we were unable to track the number of patients invited to take the survey and therefore do not know the proportion of patients responding. Selection bias may also have occurred insofar as patients who were more satisfied with treatment may have been more likely to respond to their clinician's invitation to complete the survey.
CONCLUSIONS
In spite of these limitations, to our knowledge, this is the first study examining patients' perceptions of telehealth for outpatient SUD treatment during the COVID‐19 pandemic by treatment service type. Importantly, while there was high overall satisfaction with telehealth services and many participants found telehealth more accessible than in‐person treatment, there was variability with respect to the preferred mode of treatment delivery. Although almost 40% of the sample reported that there was nothing that they dislike about telehealth, some participants also identified important potential barriers, such as difficulty forming connections with other group members, difficulties discussing sensitive topics, lower feelings of safety through telehealth, and difficulty with internet connectivity. With the goal of using telehealth to potentially increase access to SUD outpatient treatment services, it will be important for new research to examine the relationship among patient preferences for telehealth versus in‐person treatment services, treatment access, engagement, retention, and SUD treatment outcomes.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENTS
The authors would like to thank Elizabeth Fox for supplying outpatient encounter data and Angela Perrault for providing data on unique patient visits. The authors would like to acknowledge the support from NIDA K23DA050780 (DES) and R01DA048533 (ABB and SFG), and the Charles Engelhard Foundation.
Sugarman DE, Busch AB, McHugh RK, et al. Patients' perceptions of telehealth services for outpatient treatment of substance use disorders during the COVID‐19 pandemic. Am J Addict. 2021;30:445‐452. 10.1111/ajad.13207
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020. [Google Scholar]
- 2.Huskamp HA, Busch AB, Souza J, et al. How is telemedicine being used in opioid and other substance use disorder treatment? Health Aff. 2018;37:1940‐1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uscher‐Pines L, Cantor J, Huskamp HA, Mehrotra A, Busch AB, Barnett M.Adoption of telemedicine services by substance abuse treatment facilities in the U.S. J Subst Abuse Treat. 2020;117:108060. 10.1016/j.jsat.2020.108060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin LA, Casteel D, Shigekawa E, Weyrich MS, Roby DH, McMenamin SB.Telemedicine‐delivered treatment interventions for substance use disorders: a systematic review. J Subst Abuse Treat. 2019;101:38‐49. [DOI] [PubMed] [Google Scholar]
- 5.Drug Enforcement Agency . Implementation of the Ryan Haight Online Pharmacy Consumer Protection Act of 2008. Interim final rule with request for comments. Fed Regist. 2009;74:15595‐15625. [PubMed] [Google Scholar]
- 6.Bosworth A, Ruhter J, Samson LW, et al. Mediciare beneficiary use of telehealth vistis: early data from the start of the COVID‐19 pandemic. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services; 2020. [Google Scholar]
- 7.Mehrotra A. The impact of the COVID‐19 pandemic on outpatient visits: a rebound emerges [published online ahead of print May 19, 2020]. To the Point (blog); 2020. 10.26099/ds9e-jm36 [DOI]
- 8.Huskamp HA, Busch AB, Uscher‐Pines L, Barnett ML, Riedel L, Mehrotra A.Treatment of opioid use disorder among commercially insured patients in the context of the COVID‐19 pandemic. JAMA. 2020;324:2440‐2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Federation of State Medical Boards . U.S. states and territories modifying requirements for telehealth in response to COVID‐19. September 22, 2020. https://www.fsmb.org/siteassets/advocacy/pdf/states‐waiving‐licensure‐requirements‐for‐telehealth‐in‐response‐to‐covid‐19.pdf. Accessed September 24, 2020.
- 10.Center for Connected Health Policy . COVID‐19 related state actions; 2020. https://www.cchpca.org. Accessed September 10, 2020.
- 11.Center for Connected Health Policy . COVID‐19 telehealth coverage policies; 2021. https://cchp.nyc3.digitaloceanspaces.com/2021/04/Spring2021_COVIDPolicies.pdf. Accessed May 19, 2021.
- 12.Drago A, Winding TN, Antypa N.Videoconferencing in psychiatry, a meta‐analysis of assessment and treatment. Eur Psychiatry. 2016;36:29‐37. [DOI] [PubMed] [Google Scholar]
- 13.Hubley S, Lynch SB, Schneck C, Thomas M, Shore J.Review of key telepyschiatry outcomes. World J Psychiatry. 2016;6:269‐282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osenbach JE, O'Brien KM, Mishkind M, Smolenski DJ.Synchronous telehealth technologies in psycotherapy for depresssion: a meta‐analysis. Depress Anxiety. 2013;31:1058‐1067. [DOI] [PubMed] [Google Scholar]
- 15.Rees CS, Maclaine E.A systematic review of videoconference‐delivered psychological treatment for anxiety disorders. Aust Psychol. 2015;50:259‐264. [Google Scholar]
- 16.Sloan DM, Gallagher MW, Feinstein BA, Lee DJ, Pruneau GM.Efficacy of telehealth treatments for posttraumatic stress‐related symptoms: a meta‐analysis. Cogn Behav Ther. 2011;40:111‐125. [DOI] [PubMed] [Google Scholar]
- 17.Cowan KE, McKean AJ, Gentry MT, Hilty DM.Barriers to use of telepsychiatry: clinicians as gatekeepers. Mayo Clin Proc. 2019;94:2510‐2523. [DOI] [PubMed] [Google Scholar]
- 18.King VL, Brooner RK, Peirce JM, Kolodner K, Kidorf MS.A randomized trial of Web‐based videoconferencing for substance abuse counseling. J Subst Abuse Treat. 2014;46:36‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tarp K, Mejldal A, Nielsen AS.Patient satisfaction with videoconferencing‐based treatment for alcohol use disorders. Addict Disord Treat. 2017;16:70‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gittins Stone DI, Sperling JB, Potter MP, Boger KD. McLean Anxiety Mastery Program Telehealth Satisfaction Questionnaire (MAMP‐TSQ) [Unpublished Questionnaire]; 2020.
- 21.Gentry MT, Lapid MI, Clark MM, Rummans TA.Evidence for telehealth group‐based treatment: a systematic review. J Telemed Telecare. 2019;25:327‐342. [DOI] [PubMed] [Google Scholar]
- 22.Jenkins‐Guarnieri MA, Pruitt LD, Luxton DD, Johnson K.Patient perceptions of telemental health: systematic review of direct comparisons to in‐person psychotherapeutic treatments. Telemed J E Health. 2015;21:652‐660. [DOI] [PubMed] [Google Scholar]
- 23.Urbanoski KA, Kelly JF, Hoeppner BB, Slaymaker V.The role of therapeutic alliance in substance use disorder treatment for young adults. J Subst Abuse Treat. 2012;43:344‐351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hser YI, Ober AJ, Dopp AR, et al. Is telemedicine the answer to rural expansion of medication treatment for opioid use disorder? Early experiences in the feasibility study phase of a National Drug Abuse Treatment Clinical Trials Network Trial. Addict Sci Clin Pract. 2021;16:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uscher‐Pines L, Sousa J, Raja P, Mehrotra A, Barnett M, Huskamp HA.Treatment of opioid use disorder during COVID‐19: experiences of clinicians transitioning to telemedicine. J Subst Abuse Treat. 2020;118:108124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sugarman DE, Horvitz LE, Greenfield SF, Busch AB. Clinicians' perceptions of rapid scale‐up of telehealth services in outpatient mental health treatment [published online ahead of print February 18, 2021]. Telemedicine and e‐Health. 10.1089/tmj.2020.0481 [DOI] [PMC free article] [PubMed]
- 27.Jarnecke AM, Flanagan JC.Staying safe during COVID‐19: How a pandemic can escalate risk for intimate partner violence and what can be done to provide individuals with resources and support. Psychol Trauma. 2020;12:S202‐S204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization . COVID‐19 and violence against women: What the health sector/system can do [published online ahead of print March 26, 2020].
- 29.Anderson M, Kumar M. Digital divide persists even as lower‐income Americans make gains in tech adoption [published online May 7, 2019]. Fact Tank: News in the Numbers.
- 30.Perrin A, Turner E.Smartphones Help Blacks, Hispanics Bridge Some‐But Not All‐Digital Gaps With Whites. Washington DC: Pew Research Center; 2019. [Google Scholar]
- 31.Crawford A, Serhal E.Digital health equity and COVID‐19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. 2020;22:e19361. [DOI] [PMC free article] [PubMed] [Google Scholar]


