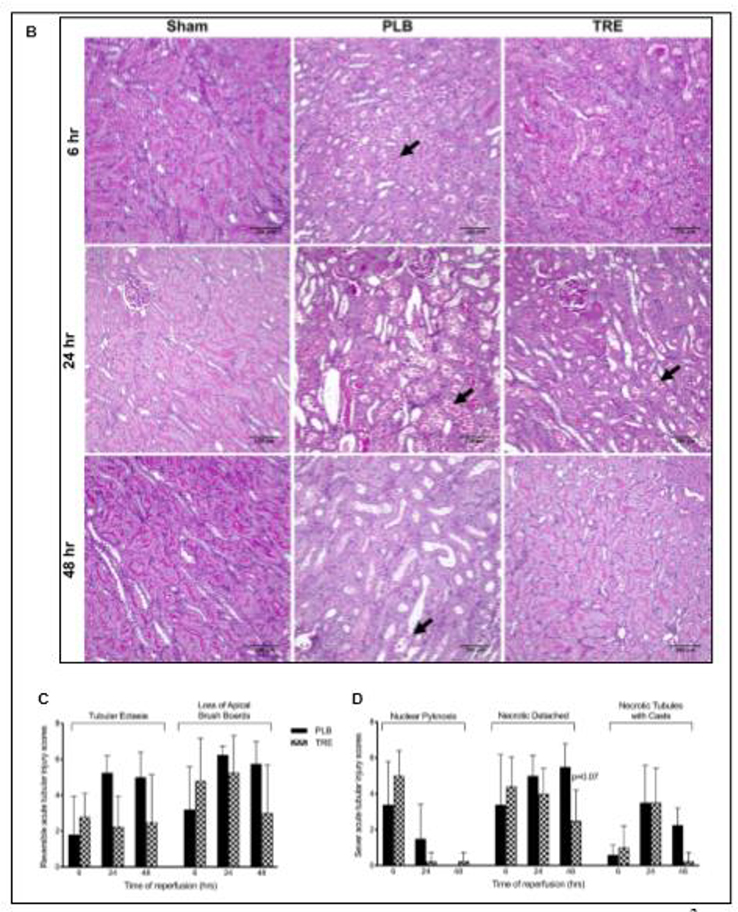
Figure 1. Treprostinil attenuates renal IRI.
(A) Serum creatinine (SCr) concentration, measured before ischemia (pre-IRI) and at 1–72 hours post-reperfusion in CTRL, sham, PLB, and TRE-treated animals. (B) Representative histopathological images of PAS-stained paraffin sections of kidneys from rats sacrificed at 6-, 24-, and 48-hour post-reperfusion and from sham-operated animals (×200, scale bar = 100 μm). Black arrows indicate tubular epithelial cell necrosis and detachment from basement membranes in IRI-placebo animals. Semiquantitative analysis of tubular epithelial injury, histological features associated with (C) reversible tubular epithelial cell injury, consisting of tubular ectasia and loss of apical brush borders; (D) irreversible tubular epithelial cell injury, consisting of epithelial cell nuclear pyknosis, detachment of necrotic epithelial cells from basement membranes and filling of tubule lumens by casts comprising necrotic cell debris. Slides were evaluated in a blinded manner using a grading system: 0: <1%; 1: 1–10%; 2: 10–25%; 3: 25–50%; 4: >50% of all tubules. Data are represented as mean ± SD; ***p<0.001 vs. sham, †p<0.05, ††p<0.01, †††p<0.001 vs. placebo (n = 4–10/group). Two-way ANOVA, Tukey’s multiple comparison test. IRI: Ischemia-reperfusion injury; SCr: Serum creatinine; CTRL: control; PLB: IRI-placebo; TRE: IRI-treprostinil; PAS: Periodic acid–Schiff staining reaction.